Pomegranate, the jewel-toned fruit revered across cultures and centuries, is more than just a vibrant addition to your plate. Science is now catching up with tradition, revealing that this antioxidant-rich fruit holds remarkable digestive benefits. Whether consumed as juice, fresh arils, or potent peel extract, pomegranate has the power to nourish your gut, tame inflammation, and promote a healthier microbiome.
In this post, we’ll explore what makes pomegranate a digestive superhero, dive into the latest scientific findings (2024–2025), and offer practical, evidence-backed ways to include it in your daily routine. We’ll also look into how pomegranate interacts with the gut-brain axis, what its metabolites do at the cellular level, and what future research is likely to uncover.
1. What Makes Pomegranate Special for Digestion?
At the core of pomegranate’s digestive power lies a combination of:
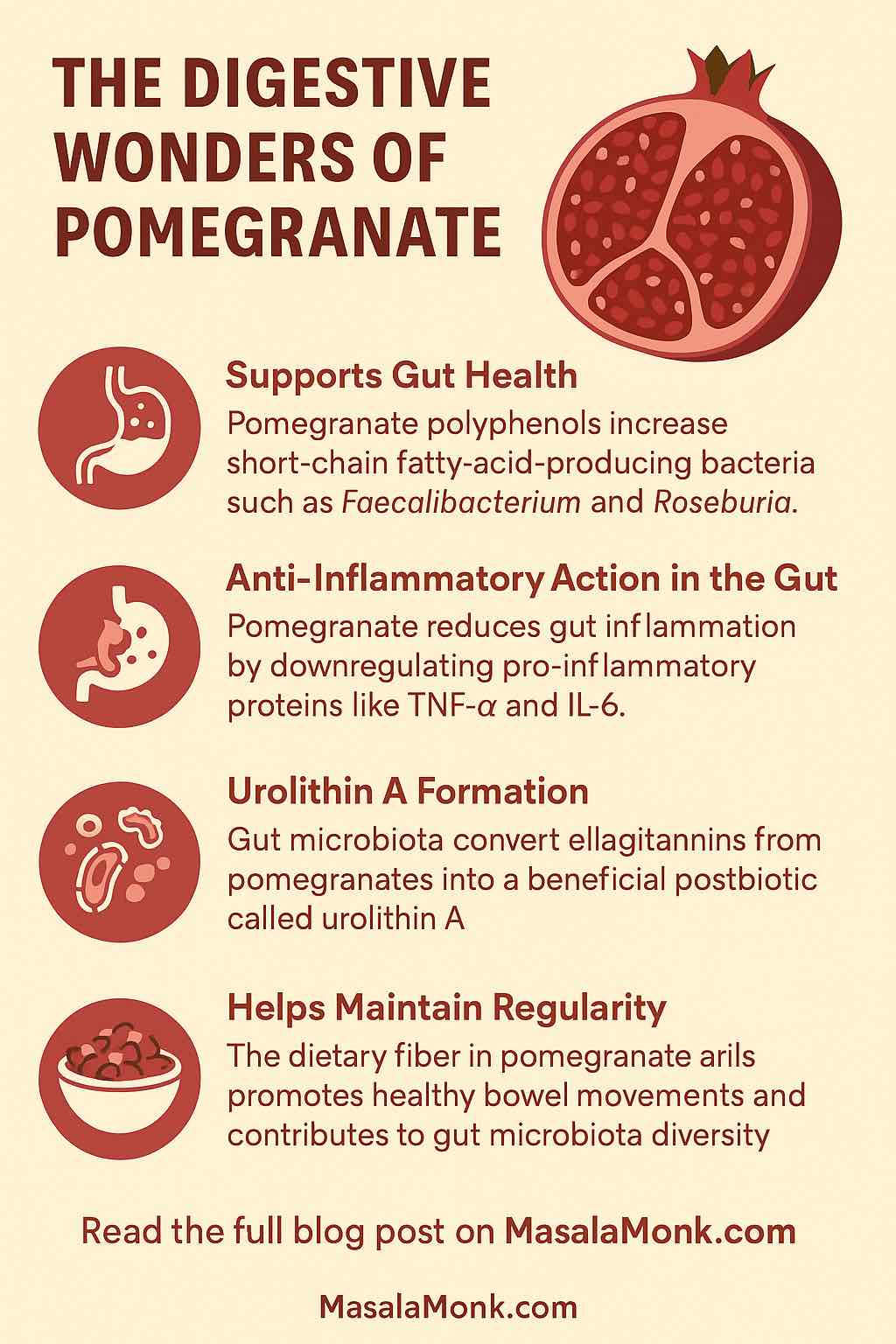
- Polyphenols (especially punicalagins and ellagic acid): potent antioxidants that support gut lining and modulate inflammation. These polyphenols are hydrolyzed into ellagic acid and then transformed by gut microbes into bioavailable metabolites like urolithins.
- Dietary Fiber: found in the seeds (arils), fiber acts as a substrate for fermentation by beneficial gut bacteria, contributing to short-chain fatty acid (SCFA) production and stool regularity.
- Urolithins: postbiotic metabolites such as urolithin A are known to improve mitochondrial function, reduce intestinal inflammation, and support epithelial barrier integrity.
These components work synergistically to support your gut in multiple ways—from encouraging beneficial bacteria and tightening the gut lining to reducing oxidative stress and systemic inflammation.
2. Gut Health Benefits: Backed by the Latest Research (2024–2025)
Let’s dig into what recent studies reveal about how pomegranate works in your digestive system:
✅ Boosts Beneficial Bacteria and SCFA Production
A 2024 randomized controlled trial using a standardized pomegranate extract (Pomella®, 75 mg punicalagins/day) found:
- Increased populations of SCFA-producing bacteria like Roseburia faecis, Coprococcus eutactus, and Faecalibacterium prausnitzii, known for their anti-inflammatory properties.
- Circulating propionate levels significantly increased, with acetate trending upward. SCFAs are crucial for maintaining colonic pH, fueling colonocytes, and supporting immune balance.
✅ Modulates Microbiota Composition
A 2025 dietary intervention in healthy female students in Egypt showed that consuming ~130g of fresh pomegranate arils daily:
- Shifted the microbiota toward beneficial taxa like Prevotella and Enterococcus.
- Decreased pro-inflammatory genera like Dysosmobacter and Collinsella, indicating a more resilient and anti-inflammatory gut profile.
✅ Supports Gut Barrier and Reduces Inflammation
In a 12-week pilot trial involving patients with inflammatory bowel disease (IBD) in remission:
- Daily pomegranate juice reduced fecal calprotectin and plasma endotoxin levels, both markers of intestinal inflammation and permeability.
- Upregulated genes responsible for mucosal immunity and tight junction protein expression, including AHR (aryl hydrocarbon receptor), NFIL3, and NCF4.
✅ Depends on Your Microbiome (Urolithin Metabotypes)
Not everyone can convert pomegranate polyphenols into urolithins. Only ~40% of individuals are classified as “urolithin A producers.” This depends on the presence of specific bacterial species such as Enterocloster bolteae and Gordonibacter urolithinfaciens.
People who do produce urolithins may experience more pronounced systemic effects, including improved glucose uptake in muscle cells, anti-aging mitochondrial signaling, and anti-inflammatory immune modulation.
3. How to Use Pomegranate Practically
Incorporating pomegranate into your diet can be simple and enjoyable. Here’s a breakdown of forms, suggested doses, and practical applications:
| Form | How to Use | Digestive Benefits |
|---|---|---|
| Fresh Arils | Eat 1/2 to 1 cup daily | Adds fiber, polyphenols; supports regularity and microbiota balance |
| Juice (100% pure) | 100–200 ml/day | Delivers polyphenols; helps reduce gut inflammation and oxidative stress |
| Peel Extract Capsules | Follow product dosage (standardized to punicalagins) | Antimicrobial and anti-inflammatory action in the gut |
| Fermented Products (e.g. pomegranate yogurt/kombucha) | 1 serving/day | Combines probiotics + polyphenols for synergistic gut benefits |
Pro Tips:
- Pair with prebiotics like inulin or resistant starch to further enhance SCFA production.
- For better urolithin conversion, consider periodic microbiome testing to identify your metabotype.
- Use a variety of delivery forms (e.g. alternating between fresh fruit and extract) to ensure broad spectrum benefits.
4. Exploring the Gut-Brain Axis and Beyond
Recent research suggests that polyphenols and urolithins may influence not just gut health, but also mood and cognition via the gut-brain axis. Some mechanisms include:
- Modulation of neurotransmitter-producing bacteria like Bifidobacterium adolescentis.
- Reduction of systemic inflammation that contributes to mood disorders.
- Enhancement of vagal tone through improved gut barrier function and SCFA-mediated signaling.
This means that regular pomegranate consumption might help not just with digestion, but also with stress resilience and mental clarity.
5. Who Should Be Cautious?
While pomegranate is generally safe, it’s important to be mindful of certain interactions:
- Blood pressure: Pomegranate juice may enhance the effects of antihypertensive medications.
- Blood thinners: It may interact with warfarin and other anticoagulants by affecting cytochrome P450 enzymes.
- Allergic reactions: Rare but possible; particularly with peel extract supplements.
- High-dose extract use: Start with a low dose to assess tolerance, especially in sensitive individuals.
6. Final Thoughts: Small Fruit, Big Impact
The latest science confirms what ancient traditions always suspected: pomegranate is a potent ally for digestive health. From modulating the gut microbiome to reinforcing intestinal integrity and even influencing mood, this fruit delivers multi-level support.
You don’t need a drastic change to see benefits. Start small: a handful of seeds with breakfast, a glass of juice post-workout, or a supplement during your gut-healing protocol. Consistency is key.
By aligning your diet with microbiome-friendly choices like pomegranate, you can take a proactive role in your digestive wellness—naturally, effectively, and deliciously.
🔍 Frequently Asked Questions (FAQs)
1. How much pomegranate should I consume daily for digestive benefits?
For most adults, ½ to 1 cup of fresh arils or 100–200 ml of pure pomegranate juice per day provides sufficient polyphenols and fiber to support gut health.
2. Can pomegranate help with IBS or IBD symptoms?
Yes, studies show that pomegranate juice and extracts can reduce gut inflammation markers like calprotectin and endotoxins, especially in IBD patients in remission. It may also ease IBS-related discomfort by modulating gut bacteria.
3. What is urolithin A, and why is it important?
Urolithin A is a postbiotic compound created by gut bacteria from pomegranate polyphenols. It supports mitochondrial health, reduces inflammation, and helps maintain the intestinal barrier—making it central to pomegranate’s digestive benefits.
4. What if I can’t produce urolithin A?
Only about 40% of people can naturally produce it. You can still benefit from other polyphenols and fiber in pomegranate, and combining it with prebiotics (like inulin) may help support the microbial pathways needed to convert ellagitannins.
5. Are there any side effects of consuming pomegranate regularly?
For most people, it’s safe. However, large amounts of juice or concentrated peel extract may cause GI upset. If you’re on blood thinners or antihypertensives, consult your doctor first.
6. Is pomegranate peel safe to consume?
Pomegranate peel contains high levels of punicalagins but is not edible raw. Use it in standardized extract form (e.g., capsules) under dosage guidance to safely harness its antimicrobial and anti-inflammatory properties.
7. Should I choose juice, whole fruit, or extract?
Each has benefits:
- Juice: Easy source of polyphenols, fast absorption.
- Fresh arils: Adds fiber and prebiotics, ideal for gut microbiota.
- Extracts: High potency for targeted benefits (e.g., inflammation, SCFA support).
8. Can children benefit from pomegranate for gut health?
Yes, but serve small, age-appropriate portions. The fiber and antioxidants can support microbiome development. Avoid giving supplements to children unless guided by a healthcare provider.
9. Is there a best time of day to consume pomegranate?
There’s no strict rule, but morning or mid-day consumption may better align with digestive activity and microbiota circadian rhythms. Juice post-workout may also help with inflammation recovery.
10. Can pomegranate help with bloating or irregularity?
Yes. The fiber in arils promotes regular bowel movements, and the polyphenols reduce inflammatory triggers that can contribute to bloating and discomfort.