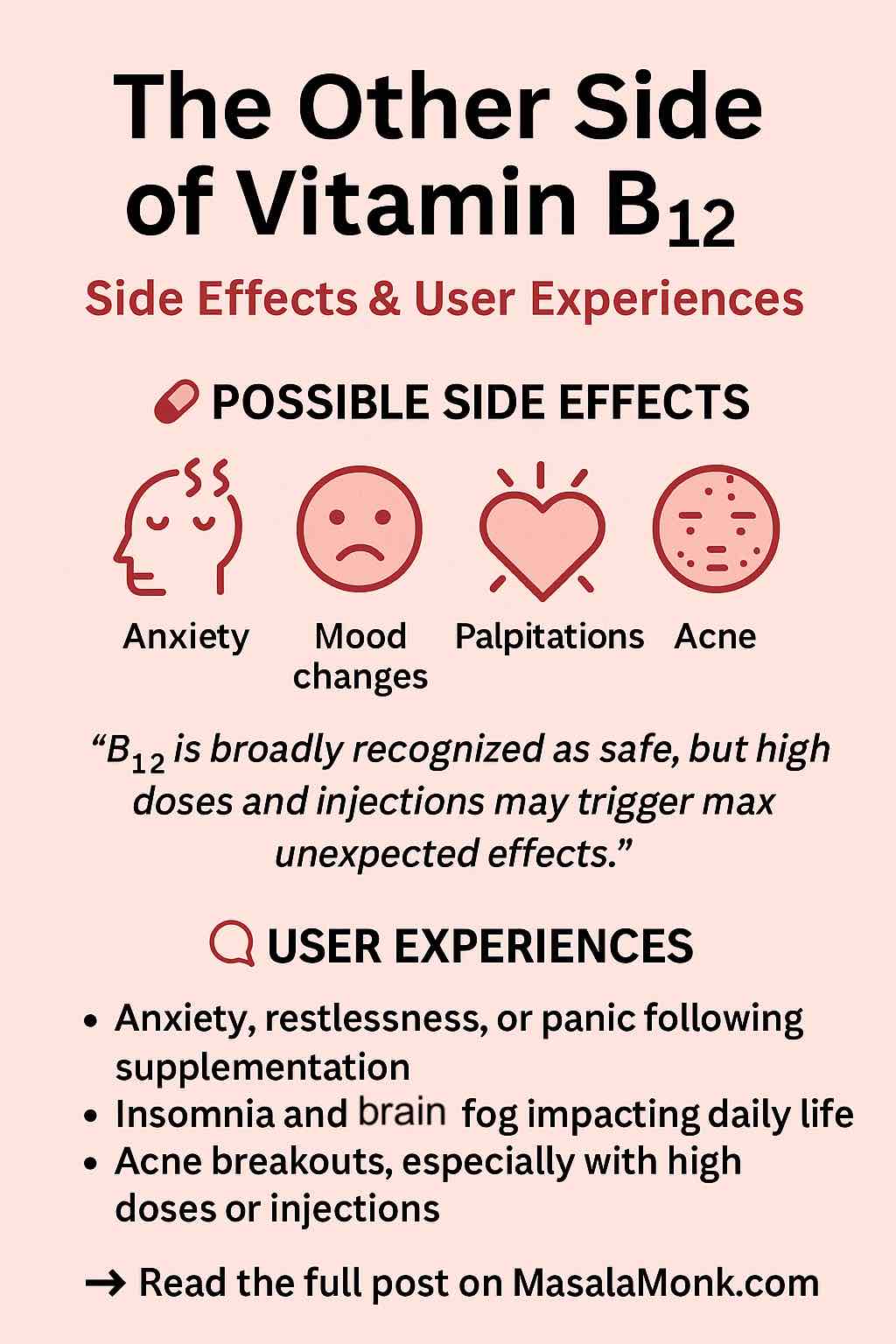
The Other Side of Vitamin B12: Side Effects, User Experiences & What You Should Know
Vitamin B12, often hailed as a vital nutrient for energy, nerve function, and red blood cell production, has gained immense popularity in recent years. With shelves full of B12 supplements and wellness influencers promoting high-dose injections, it’s easy to assume this water-soluble vitamin is universally safe and side-effect-free. But as with anything we put in our bodies, there is nuance—and in this case, growing awareness of side effects, both clinical and anecdotal.
In this comprehensive post, we’ll break down everything you need to know about Vitamin B12 side effects—from established medical research to real-world user stories—and what that means for you practically. Whether you’re supplementing due to a deficiency or looking for a cognitive boost, this is your deep dive into the other side of B12.
Quick Overview: What is Vitamin B12?
Vitamin B12 (cobalamin) is a water-soluble vitamin crucial for:
- DNA synthesis
- Energy metabolism
- Red blood cell production
- Neurological function
It’s naturally found in animal products like meat, eggs, dairy, and fish. Many people—especially vegetarians, vegans, older adults, and those with absorption issues—take supplements in the form of oral pills, sublingual tablets, nasal sprays, or intramuscular injections.
The Standard View: Safe and Beneficial
In clinical practice, B12 is considered extremely safe—even at high doses. Being water-soluble, excess B12 is typically excreted through urine. For example, dosages of 1,000 mcg or more are routinely used to treat deficiencies without major concern for toxicity. The Institute of Medicine has not established an upper limit for B12 intake, reflecting its low toxicity profile.
However, safety doesn’t mean no effects. Let’s unpack what current science and users are saying.
Common Side Effects: What Clinical Literature Says
According to sources like Drugs.com and the Mayo Clinic, the following side effects are rare but possible:
Mild to Moderate Side Effects:
- Headache
- Nausea or upset stomach
- Mild diarrhea
- Skin rash or itching
- Pain or redness at injection site
More Serious (but Rare) Side Effects:
- Dizziness or confusion
- Hypokalemia (low potassium) in cases of rapid red blood cell production
- Allergic reactions (especially with injectable cyanocobalamin), including swelling, shortness of breath, or anaphylaxis
Real-World User Experiences: Reddit, Forums & Case Studies
While official data suggest B12 is benign, thousands of personal stories online tell a more complex tale.
1. Neurological and Psychiatric Effects
Some users report experiencing:
- Brain fog
- Anxiety or panic attacks
- Insomnia
- Restlessness
- Palpitations
- Feelings of dissociation or derealization
These effects are usually associated with high-dose supplementation (500 mcg to 5000 mcg daily) or B12 injections. In some Reddit threads, users describe feeling overstimulated or mentally “off” after starting B12—symptoms sometimes lasting days or even weeks after stopping.
2. Dermatological Issues
A subset of people report:
- Acne flare-ups (particularly cystic acne)
- Itchy skin or rashes
These reactions appear more commonly with the cyanocobalamin form of B12.
3. Gastrointestinal Distress
Despite its role in metabolism, B12 can sometimes irritate the stomach:
- Nausea
- Abdominal discomfort
- Loss of appetite
4. Individual Case Reports
A 2024 case study published in The Parker Journal of Health Science described a woman who developed anxiety, palpitations, acne, and insomnia after taking 1,000 mcg of cyanocobalamin daily for 12 days. Her symptoms resolved after discontinuation.
Another study from Frontiers in Hematology detailed three elderly women whose severe B12 deficiencies caused hemolytic anemia. While supplementation improved their health, it highlighted how B12 therapy must be monitored—especially during the initial correction phase.
Why Do These Effects Happen?
Several possible explanations include:
- Cobalt sensitivity: B12 contains cobalt, which may cause allergic or histamine reactions in sensitive individuals.
- Rapid red blood cell turnover: Can cause electrolyte shifts (especially low potassium), leading to dizziness or fatigue.
- Metabolic effects: B12 influences methylation pathways, which affect neurotransmitter production. Imbalances may lead to anxiety, irritability, or overstimulation.
- Genetic factors: Variants in genes like MTHFR or COMT may alter how your body processes B12 and related nutrients.
Practical Guidelines: How to Use B12 Safely
1. Start Low and Go Slow
If you’re supplementing preventively (not correcting a deficiency), start with low doses (e.g., 100–250 mcg/day). Increase only if needed and tolerated.
2. Choose the Right Form
- Cyanocobalamin: Most common but more likely to cause reactions.
- Methylcobalamin: Active form; generally better tolerated.
- Hydroxocobalamin: Often used for injections; longer-lasting in the body.
3. Watch for Symptoms
Track your mood, sleep, energy, skin, and digestion. Discontinue or adjust if you experience negative effects.
4. Balance with Other Nutrients
Ensure adequate intake of folate, B6, magnesium, and potassium, especially if you’re correcting a deficiency.
5. Consult a Healthcare Provider
Particularly if you:
- Are pregnant or breastfeeding
- Have kidney or liver disease
- Are taking medications like metformin, PPIs, or antipsychotics
- Experience unusual or severe symptoms
Conclusion: Respecting the Nuance
Vitamin B12 is undoubtedly essential—and often life-changing—for people with true deficiencies. But as the trend of high-dose supplementation grows, so does the importance of understanding potential side effects.
While many people tolerate B12 perfectly well, others may experience unexpected physical, neurological, or psychological symptoms. Whether due to dose, form, or individual biology, these effects deserve attention, not dismissal.
Approach B12 with the same respect you’d give any potent nutrient: stay informed, start cautiously, and listen to your body.
Have you experienced side effects from B12? Share your story in the comments below or let us know what worked for you!
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice.
🔍 Frequently Asked Questions (FAQs)
1. Is it possible to have side effects from Vitamin B12?
Yes, although Vitamin B12 is generally safe, some people—especially when taking high doses or injections—report side effects like anxiety, insomnia, acne, or palpitations. Most are mild and reversible.
2. What’s the most common side effect of B12 supplementation?
Mild digestive upset (like nausea or diarrhea), headache, and skin reactions are among the most frequently reported. Injection-site discomfort is common if using B12 shots.
3. Can B12 supplements cause anxiety or mood swings?
Yes, some users report increased anxiety, restlessness, or even panic attacks after starting high-dose B12, likely due to overstimulation of the nervous system or changes in neurotransmitter activity.
4. How long do B12 side effects last?
Most side effects subside within a few days to two weeks after stopping or adjusting the dosage. However, in rare cases, symptoms like insomnia or anxiety may linger longer.
5. Which form of B12 is least likely to cause side effects?
Methylcobalamin and hydroxocobalamin tend to be better tolerated than cyanocobalamin, which may cause more allergic or dermatological reactions in sensitive individuals.
6. Can you overdose on B12?
It’s very difficult to overdose on B12, especially orally, because excess is excreted in urine. However, high doses can still trigger unwanted symptoms in sensitive individuals.
7. What should I do if I feel worse after taking B12?
Stop supplementation temporarily and monitor your symptoms. Consider switching forms (e.g., from cyanocobalamin to methylcobalamin) or lowering the dose. Always consult your healthcare provider if symptoms are significant.
8. Are side effects more common with B12 injections?
Yes. Injections can deliver a large dose rapidly, which may trigger more noticeable side effects like flushing, dizziness, or anxiety—especially in first-time users.
9. Can B12 affect skin or cause acne?
Yes, acneiform eruptions—especially cystic acne—have been reported, particularly with high doses or injections of cyanocobalamin.
10. Should I take B12 daily or weekly?
It depends on your needs. Daily low-dose B12 is usually sufficient for maintenance. If you’re correcting a deficiency, your doctor may recommend high-dose daily or weekly doses, often via injection.