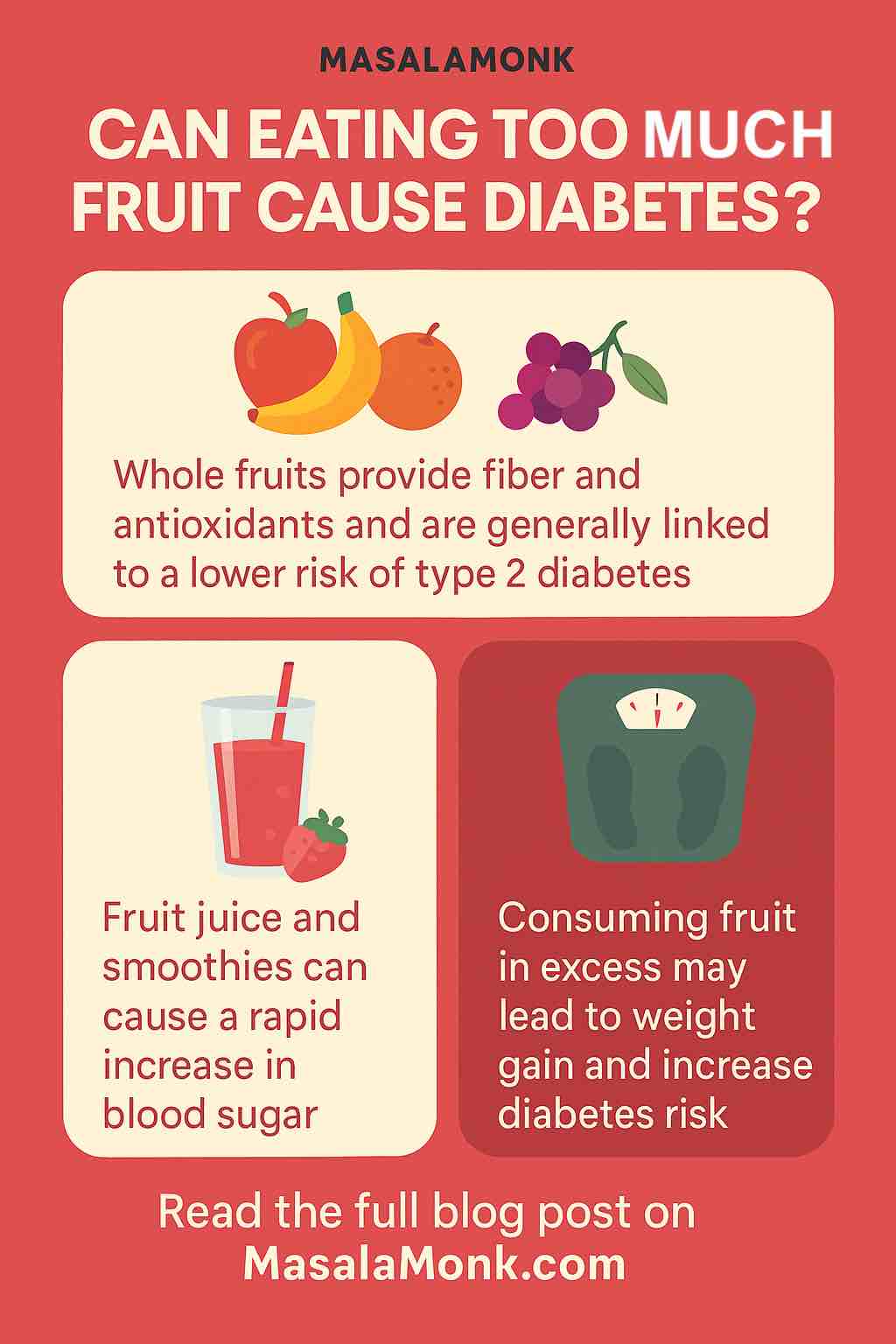
Fruit is nature’s candy: colorful, sweet, and packed with nutrients. But in the era of rising diabetes and insulin resistance, the question often arises: Can eating too much fruit actually cause diabetes? This blog post takes a detailed, science-backed look at the relationship between fruit consumption and diabetes risk—including what forms of fruit are helpful or harmful, how much is too much, and how to make the healthiest choices.
🌐 Understanding the Diabetes Landscape
Diabetes, particularly Type 2 diabetes, is a metabolic disorder where the body either resists insulin or doesn’t produce enough of it. It is driven primarily by:
- Chronic overnutrition (especially from processed foods)
- Sedentary lifestyles
- Genetics
- Hormonal imbalances
Rising rates of obesity and insulin resistance are strongly tied to excess calorie consumption, especially from refined carbohydrates and added sugars.
🍏 Fruit: What Makes It Unique?
Fruits contain natural sugars (mainly fructose and glucose), but they’re also rich in:
- Dietary fiber
- Vitamins and minerals (like vitamin C, potassium)
- Phytochemicals and antioxidants (like flavonoids and anthocyanins)
These compounds work synergistically to slow sugar absorption, reduce inflammation, and improve overall metabolic health. That makes fruit fundamentally different from added sugars or sugar-sweetened beverages.
⚡️ What the Science Says: Whole Fruit and Diabetes Risk
The Protective Power of Whole Fruit
- A 2022 Chinese cohort study of 76,000+ adults showed that consuming fresh fruit ≥ 7 times per week was linked to a 16% lower risk of Type 2 diabetes.
- A meta-analysis from Harvard found that people who ate 3 or more servings per week of blueberries, grapes, and apples had a significantly lower diabetes risk.
- Whole fruit improves insulin sensitivity and supports healthy weight management due to its fiber and nutrient content.
But What About Too Much?
While moderate fruit consumption is beneficial, extremely high intake (think 8-10+ servings per day) could become problematic if:
- It leads to excess calorie intake and weight gain
- You already have insulin resistance or prediabetes
That said, there’s little evidence that even high fruit intake directly causes diabetes—but calorie balance still matters.
🍽️ The Real Villains: Juice, Smoothies & Dried Fruits
❌ Fruit Juice
Even 100% fruit juice lacks fiber and delivers concentrated sugar. Studies show:
- Regular juice consumption is associated with a 15% increased diabetes risk.
- Replacing juice with whole fruit reduces diabetes risk.
❌ Smoothies
Often loaded with bananas, dates, or juice, many smoothies pack a sugary punch. Without the chewing and fiber content of whole fruit, they can spike blood glucose quickly.
❌ Dried Fruits
While rich in nutrients, they’re calorie-dense and easy to overconsume. A handful of raisins equals the sugar of a whole bunch of grapes.
Bottom line: It’s not fruit that’s the issue—it’s how it’s consumed.
🫰 Who Should Be More Cautious?
If you have prediabetes, insulin resistance, or are managing type 2 diabetes, you can still enjoy fruit—but with mindfulness:
- Prioritize low-glycemic fruits: berries, apples, pears, kiwi, citrus
- Limit high-sugar fruits: grapes, mangoes, bananas (especially overripe)
- Pair fruit with protein or healthy fat to slow absorption (e.g., apple + almond butter)
- Stick to 1 serving per sitting, spaced across the day
Consult with a registered dietitian if you’re managing blood sugar.
🔄 Practical Tips: Enjoying Fruit the Right Way
- Stick to 2–4 servings per day (1 serving = 1 medium apple or ½ cup berries)
- Avoid fruit juice; opt for infused water or whole fruit instead
- Blend smartly: Use fiber-rich fruit (like berries) and add protein (e.g., Greek yogurt)
- Be portion-wise with dried fruit; combine with nuts to blunt sugar spikes
- Eat fruit with meals, not alone, to slow glucose release
📖 Conclusion: Nature’s Sweetness in Balance
Eating fruit doesn’t cause diabetes. On the contrary, whole fruits are protective when eaten in moderation. The real concern lies in how much, what type, and what form you eat.
So go ahead—enjoy that crisp apple, bowl of blueberries, or juicy orange. Just skip the juice bar, watch your portions, and savor fruit as part of a balanced, whole-food lifestyle.
Key Takeaway: Fruit is not the enemy. Ultra-processed food, sugary beverages, and overconsumption are.
Stay sweet—the natural way.
Sources: WHO dietary guidelines, PMC meta-analyses (2022-2024), Harvard School of Public Health, Nutrition & Metabolism Journal (2024)
✅ FAQs
1. Can eating too much fruit cause diabetes?
Answer: Not directly. Whole fruit contains fiber and antioxidants that generally help prevent diabetes. However, excessive intake—especially if it leads to excess calories and weight gain—can indirectly increase risk, particularly in people with prediabetes or insulin resistance.
2. Is fruit sugar (fructose) bad for you?
Answer: Naturally occurring fructose in whole fruits is not harmful due to the fiber, water, and nutrients that slow sugar absorption. The problem arises with added fructose in sweetened beverages and processed foods, which can increase insulin resistance and fat buildup in the liver.
3. How many servings of fruit per day are safe and healthy?
Answer: Most health organizations recommend 2–4 servings per day. One serving equals about 1 medium apple, ½ cup of berries, or 1 small banana.
4. Which fruits are best for people with prediabetes or diabetes?
Answer: Choose low-glycemic fruits like berries, apples, pears, citrus fruits, and kiwi. Avoid high-glycemic or very ripe fruits like bananas, mangoes, and grapes in large amounts.
5. Should I avoid fruit juice completely?
Answer: Yes, in most cases. Even 100% fruit juice lacks fiber and causes a rapid blood sugar spike. Studies show it increases the risk of Type 2 diabetes when consumed regularly.
6. Are smoothies healthy or risky for blood sugar?
Answer: It depends on ingredients. Smoothies with multiple fruits, juice, and sweeteners can spike blood sugar. Choose recipes with whole fruits, fiber (e.g., chia, oats), and protein (e.g., Greek yogurt) to balance blood sugar response.
7. Is dried fruit bad for you?
Answer: Not inherently, but it’s very calorie-dense and easy to overeat. A small handful of raisins has the same sugar as a bunch of grapes. If you eat dried fruit, watch portions and pair it with healthy fats like nuts.
8. Can fruit help prevent diabetes?
Answer: Yes. Numerous studies show that eating moderate amounts of whole fruit, especially blueberries, apples, and grapes, is associated with reduced risk of developing Type 2 diabetes—up to 26% lower risk for some fruits.
9. What’s the best time of day to eat fruit for blood sugar control?
Answer: Eat fruit with meals, not on an empty stomach, to slow sugar absorption. Combining fruit with protein or fat (e.g., apple + peanut butter) can also reduce blood glucose spikes.
10. Is it safe for diabetics to eat fruit every day?
Answer: Yes, if chosen and portioned wisely. Diabetics can safely eat 1–3 servings of whole fruit per day, focusing on lower-sugar options and avoiding juices and dried fruits unless medically advised.