Few foods evoke as much nostalgia, flavor, and curiosity as mango pickle. Whether you grew up sneaking tangy bites from a glass jar in your grandma’s kitchen or recently discovered its punchy magic at a local Indian restaurant, mango pickle is a condiment like no other. But is it just a treat for the taste buds, or does it also have health benefits? Can it be harmful? And what makes the varieties across India and beyond so fascinating? This blog dives deep into the world of mango pickle—backed by the latest science, regional stories, and practical advice for anyone who loves (or is curious about) this spicy delight.
What is Mango Pickle?
At its core, mango pickle is a traditional preserve made from raw (unripe) mangoes, spices, oil, and salt. It’s a staple in Indian, Pakistani, Bangladeshi, and Sri Lankan homes, often accompanying rice, roti, paratha, or even humble khichdi. The beauty of mango pickle is in its infinite variations, each shaped by local traditions, climate, and the creativity of home cooks.
Why is Mango Pickle So Popular?
- Flavor Explosion: Sour, salty, spicy, sometimes sweet—each bite is a sensory adventure.
- Preservation: Before refrigeration, pickling was how families enjoyed mangoes all year round.
- Cultural Ritual: Pickle-making is a time-honored family activity, often passed down through generations.
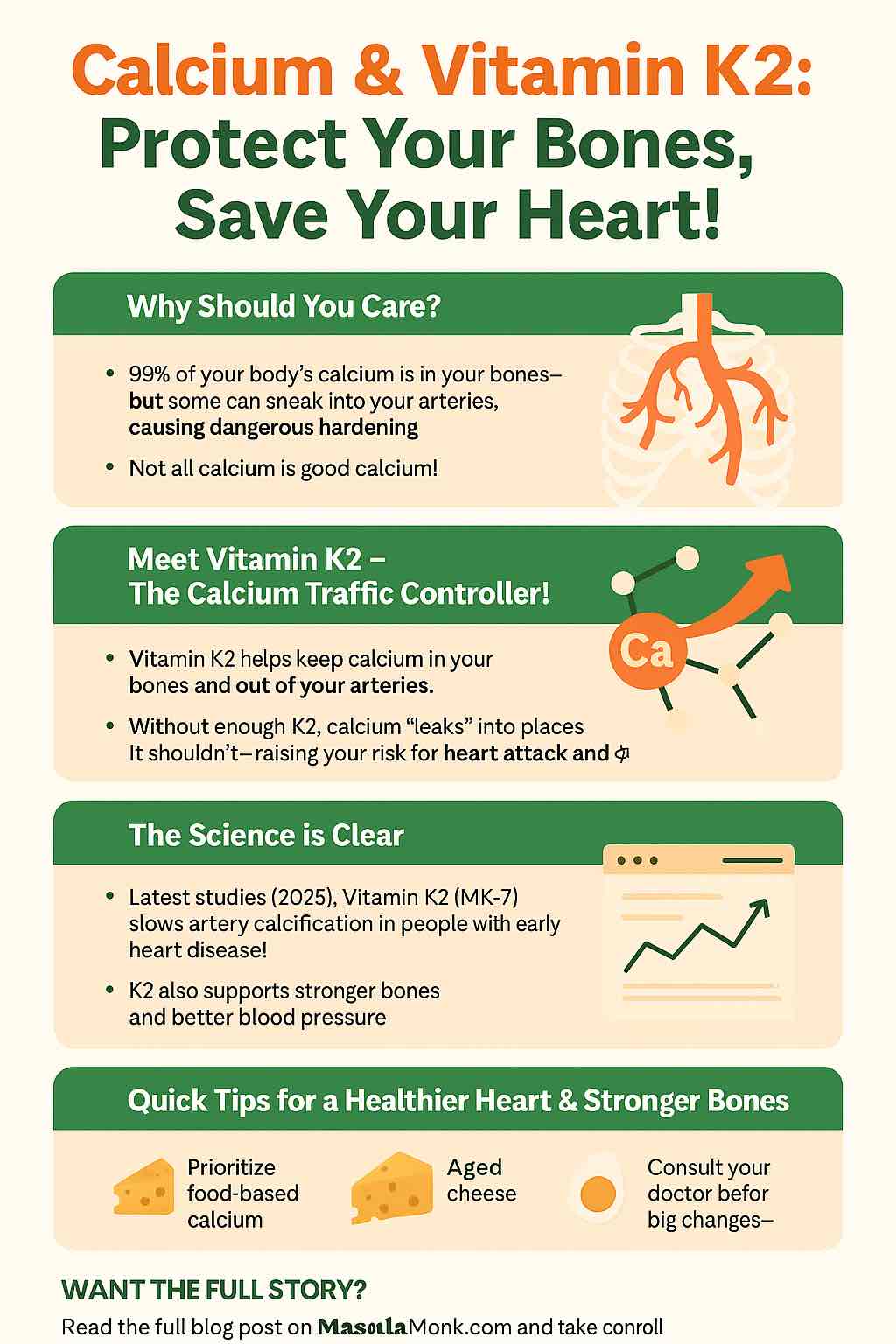
Health Benefits of Mango Pickle (Latest Insights)
1. Gut Health & Probiotics
If you’re eating a naturally fermented mango pickle (not one with vinegar or preservatives), you’re likely getting a dose of beneficial probiotics. These live bacteria can support gut health, aid digestion, reduce bloating, and may even help with nutrient absorption. Research in 2024 highlights that traditional, fermented pickles improve gut microbiome diversity, which is increasingly linked to overall wellness.
2. Digestive Enzyme Support
Spices like mustard seeds, fenugreek, asafoetida, and fennel aren’t just for flavor—they stimulate digestive enzymes, helping your body process food more efficiently. A teaspoon of mango pickle with a meal can genuinely aid digestion, which explains its classic role as a “side” on Indian thalis.
3. Rich in Antioxidants and Micronutrients
Raw mangoes provide Vitamin C, Vitamin A, and fiber, while spices like turmeric and fenugreek offer powerful antioxidants. These compounds fight free radicals, potentially slowing cell aging, reducing inflammation, and supporting immune health.
4. Boosts Appetite & Palatability
Pickle’s tangy and spicy flavors increase saliva secretion, making bland foods more appetizing. This is especially helpful for those recovering from illness or dealing with low appetite.
5. Potential Support for Skin, Heart, and Vision
- Turmeric and mango antioxidants support skin repair and may have anti-inflammatory effects.
- Potassium and magnesium (from mango and some spices) support healthy blood pressure.
- Vitamin A and carotenoids in mango can help with vision and skin glow.
6. Aiding in Weight Control (In Moderation)
Recent research notes that some spices used in mango pickle—like mustard, chili, and fenugreek—may have thermogenic (metabolism-boosting) effects. But here’s the catch: the actual impact on weight is supportive, not transformative. In other words, pickle can add a metabolic edge to a balanced meal, but isn’t a weight-loss food by itself.
Potential Side Effects and Risks (What Science and Doctors Say)
1. High Sodium Content
Pickles are inherently salty—salt is what preserves them. Regular, excessive intake can contribute to high blood pressure, water retention, and kidney stress. If you have hypertension or kidney issues, keep intake very moderate.
2. Oil Overload
Traditional recipes use plenty of oil (often mustard or sesame), which aids preservation and taste. However, some commercial brands use cheaper, less healthy oils or even hydrogenated fats. Too much oil increases calories and can raise cholesterol if the oil quality is poor.
3. Acidic & Spicy: Not for All
If you have acid reflux, gastritis, ulcers, or IBS, the acidity and spice can aggravate symptoms. Fermented pickles can also cause mild GI upset in sensitive individuals, as per recent studies.
4. Preservatives, Additives, and Spoilage
Commercial pickles may contain artificial preservatives and colors. Home-pickled jars, if not handled or stored properly, can develop molds or harmful bacteria. Always use a clean, dry spoon and store in airtight containers.
5. Potential Carcinogenic Risk (Heavily Salted/Preserved Foods)
Some studies (especially from East Asia) have linked very high intake of heavily salted, preserved vegetables to increased risk of certain cancers. For typical, moderate mango pickle consumption, risk remains low—especially with clean, home-prepared versions.
Mango Pickle Variations Across India (and Beyond!)
1. Andhra Avakaya
- Famous for: Intense heat, bold mustard flavor, and bright red color.
- Key Ingredients: Raw mango, red chili powder, mustard powder, fenugreek, sesame oil.
- Texture: Chunky, fiery, and deeply aromatic.
2. Punjabi Aam ka Achar
- Famous for: Pungent aroma (from mustard oil), slightly bitter edge (from fenugreek), and robust spices.
- Key Ingredients: Raw mango, mustard oil, fennel seeds, nigella seeds, asafoetida.
3. Gujarati Chhundo
- Famous for: Sweetness and translucence.
- Key Ingredients: Grated mango, sugar, mild spices.
- Usage: Great with theplas and snacks.
4. Kerala Kadumanga
- Famous for: Use of whole baby mangoes.
- Key Ingredients: Tiny mangoes, mustard, chili, turmeric, coconut oil (sometimes).
5. Bengali Aam-er Achar
- Famous for: Balance of tang and sweet.
- Key Ingredients: Mango, sugar, panch phoron (five-spice blend).
Pro Tip: Each state—and often each family—has its own twist. Some add garlic, some add jaggery, some use sun-drying, others ferment for weeks. There are even fusion versions using olive oil or global spices!
How to Choose and Eat Mango Pickle for Health
- Opt for Homemade or Artisanal Brands: Less likely to use preservatives or poor-quality oil.
- Go Fermented if Possible: Naturally fermented pickles offer the added benefit of probiotics.
- Watch the Serving Size: 1–2 teaspoons per meal is plenty.
- Pair with Whole Foods: Enjoy with dal, rice, and veggies—not just with fried or heavy foods.
- Store Smart: Always use clean, dry utensils. Keep jars tightly closed, and refrigerate after opening if possible.
Practical Recipes: Try Your Own Mango Pickle!
Quick Mango Pickle (No Fermentation Needed)
Ingredients:
- 2 cups raw mango, chopped
- 2 tbsp salt
- 1 tbsp chili powder
- 1 tsp turmeric
- 1 tbsp mustard seeds
- 1 tbsp fenugreek seeds
- 1 cup mustard or sesame oil
Instructions:
- Mix mango, salt, chili, and turmeric.
- Heat oil, add mustard and fenugreek seeds, let splutter, then cool.
- Combine oil and spices with mango. Store in a glass jar.
- Can be eaten after 24 hours—keeps in fridge for 2–3 weeks.
For Fermented Pickle:
Let the spiced mangoes sit in the jar (covered with muslin) at room temp for 5–7 days, stirring daily, before topping with oil and storing airtight.
Frequently Asked Questions
1. What is the healthiest way to eat mango pickle?
The healthiest way is in moderation—about 1–2 teaspoons per meal—alongside a balanced meal. Choose homemade or small-batch artisanal pickles that use natural oils, minimal salt, and avoid artificial preservatives.
2. Are store-bought mango pickles as good as homemade ones?
Homemade pickles are generally healthier, as you can control the quality of oil, salt, and spices. Many commercial brands use preservatives, artificial colors, or low-quality oils. Always check the label for clean, minimal ingredients.
3. Can mango pickle really help digestion?
Yes, mango pickle can stimulate digestive enzymes, thanks to spices like fennel, mustard, and asafoetida. Fermented pickles may also offer probiotic benefits, which support gut health.
4. Who should avoid eating mango pickle?
People with high blood pressure, kidney issues, acid reflux, gastritis, or ulcers should limit or avoid mango pickle due to its high salt, oil, and spice content.
5. How long does mango pickle last, and how should it be stored?
Properly prepared and stored in airtight, dry containers, mango pickle can last up to a year. Always use a dry spoon, avoid moisture, and refrigerate after opening if possible to prevent spoilage.
6. Is mango pickle suitable for children?
In small amounts, yes—provided it is not overly spicy or salty. Always introduce gradually and observe for any digestive discomfort.
7. Does mango pickle contain probiotics?
Only naturally fermented mango pickles (those not made with vinegar or preservatives) contain live probiotics. Most commercial pickles are not fermented and thus lack probiotic benefits.
8. Can eating mango pickle daily be harmful?
Eating small amounts daily is generally safe for healthy individuals, but overconsumption can lead to high sodium and fat intake, raising risks of hypertension or weight gain.
9. What are the different types of mango pickle found in India?
Popular varieties include Andhra Avakaya (spicy), Punjabi Aam ka Achar (aromatic and pungent), Gujarati Chhundo (sweet), Kerala Kadumanga (whole baby mangoes), and Bengali Aam-er Achar (sweet-tangy).
10. Can mango pickle help with weight loss?
Mango pickle can slightly boost appetite and digestion, but it is not a weight-loss food. The high oil and salt content mean moderation is crucial; it should be viewed as a flavorful condiment, not a health food.
In Conclusion
Mango pickle is a celebration of flavor, tradition, and yes—a little bit of science! Enjoyed in moderation, it can spice up your meals and may support digestive health, thanks to natural fermentation and healthful spices. Just remember: moderation is your friend, and homemade (or trusted small-batch) versions are usually best.
So next time you reach for that vibrant jar, know you’re savoring not just a condiment, but a slice of culinary history and well-being.
Do you have a family pickle recipe or a regional favorite? Share your story in the comments below!
Want more recipes, brand reviews, or science-backed tips? Let us know what you’d like to read next!
References:
- EatingWell: Scientists May Have Discovered a Surprising Health Benefit of Mango
- Ojas Nature: Mango Pickle and Weight Loss Benefits and Side Effects
- FarmDidi: Is Mango Pickle Good for Your Skin?
- Times of India: Lesser-Known Health Benefits One Can Get from Desi Mango Pickle
Craving more food wisdom? Follow us for in-depth guides on traditional foods, modern health, and the joy of eating well!