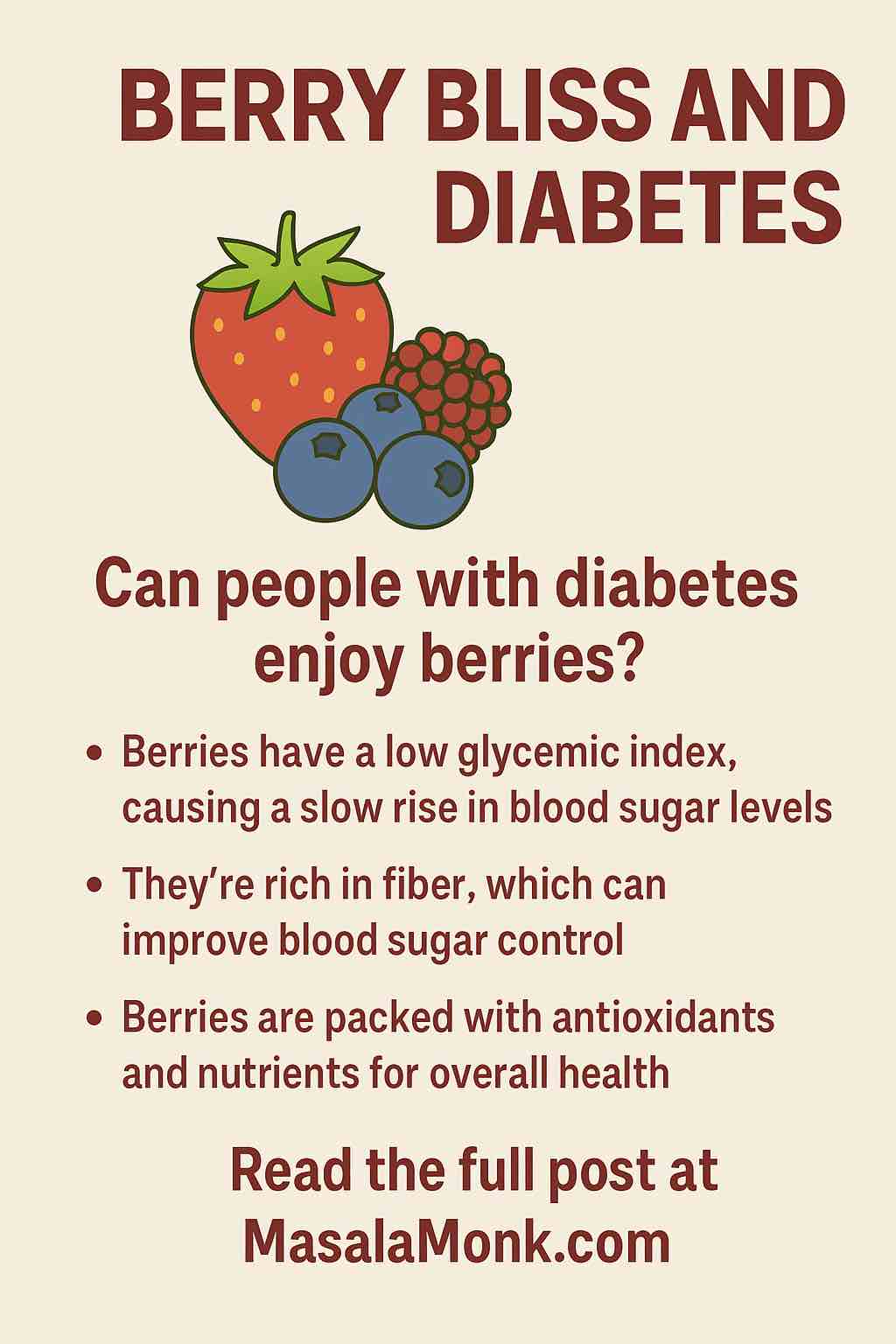
Can berries really be part of a diabetes-friendly lifestyle? If you’re diabetic—or supporting someone who is—you know that not all fruits are created equal when it comes to blood sugar. But berries, those vibrant jewels of summer, stand out as one of the healthiest, most versatile, and most enjoyable choices for people watching their glucose.
Let’s dig deep into the science, the servings, and the tastiest ways to fit more “berry bliss” into your diabetic diet—backed by the freshest research as of 2025.
5 Key Questions About Berries & Diabetes: Answered by Science
1. Are Berries Safe for Diabetics?
Yes—berries are not only safe, but highly recommended.
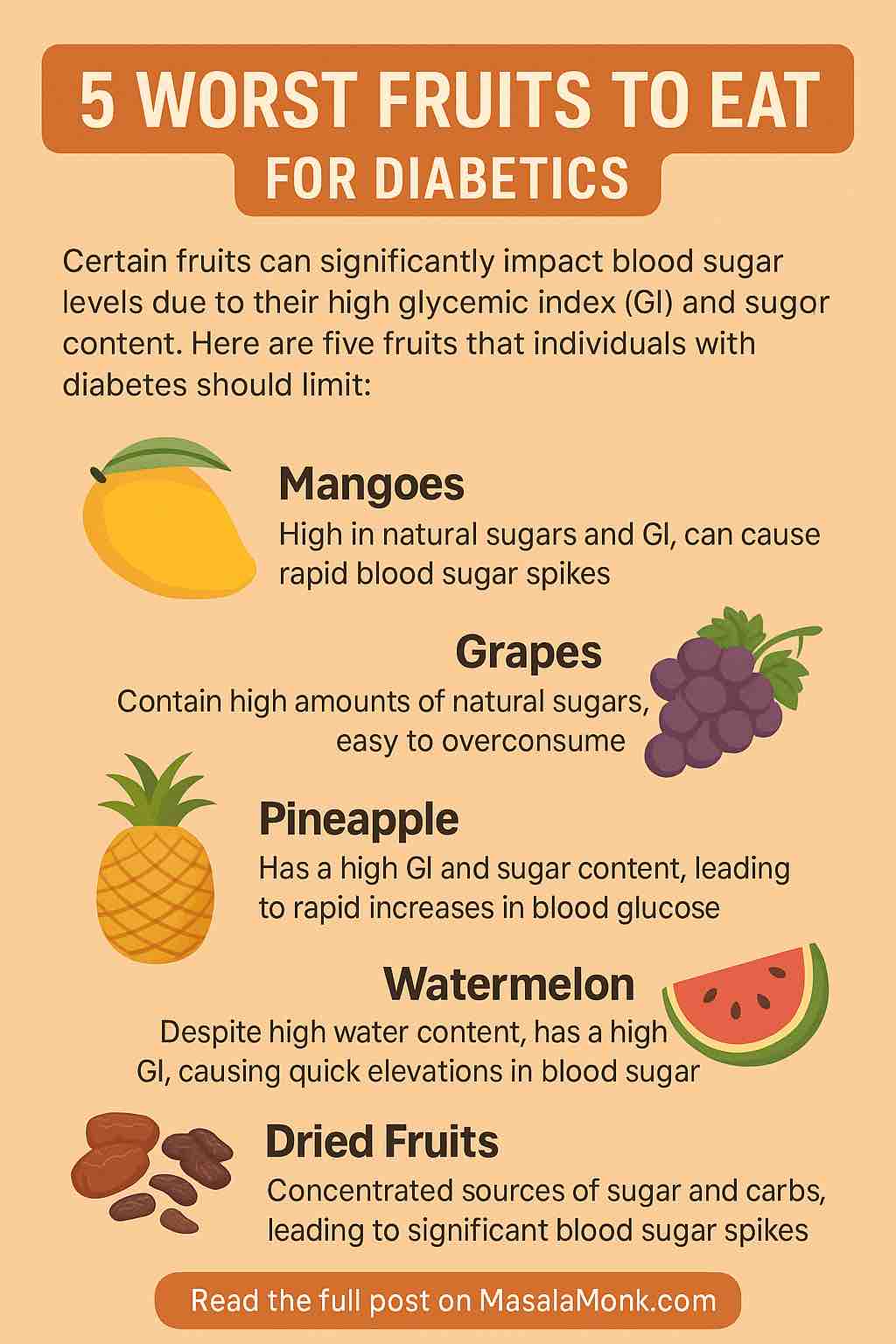
Strawberries, blueberries, raspberries, blackberries, and elderberries are all low to moderate on the glycemic index (GI), meaning they cause a much gentler rise in blood sugar than higher-GI fruits like watermelon or pineapple. Most berries have a GI below 40. They’re also bursting with fiber, antioxidants, vitamins C and K, and plant compounds called polyphenols, which actively help manage inflammation and blood sugar swings .
2. What’s the Ideal Serving Size for Blood Sugar Control?
The consensus:
¾ to 1 cup of fresh or frozen berries per serving = about 15 grams of carbohydrate (the standard “carb exchange”).
For most people with diabetes, this fits well into a balanced meal plan. The fiber content (3–8g per cup, depending on the berry) slows the absorption of sugar, minimizing spikes. Even the American Diabetes Association recommends berries as a “free fruit” for many plans, especially when paired with protein or healthy fats .
3. Do Berries Actually Help Lower Blood Sugar?
Emerging studies say YES.
- Anthocyanins—the pigments that make berries so colorful—help improve insulin sensitivity and reduce after-meal blood glucose, especially when the berries are consumed whole (not juiced).
- A 2025 study found elderberry juice reduced fasting blood sugar by 24% and insulin by 9% after one week, alongside improved gut microbiome health. However, more research is needed for long-term recommendations .
- Strawberries remain a star, delivering anti-inflammatory benefits and modestly lowering post-meal glucose when eaten regularly.
4. Should I Choose Fresh, Frozen, or Canned Berries?
All are good—if unsweetened.
- Fresh or frozen berries (with no added sugar) are nutritionally similar.
- Canned berries are OK if packed in water or their own juice—avoid syrup!
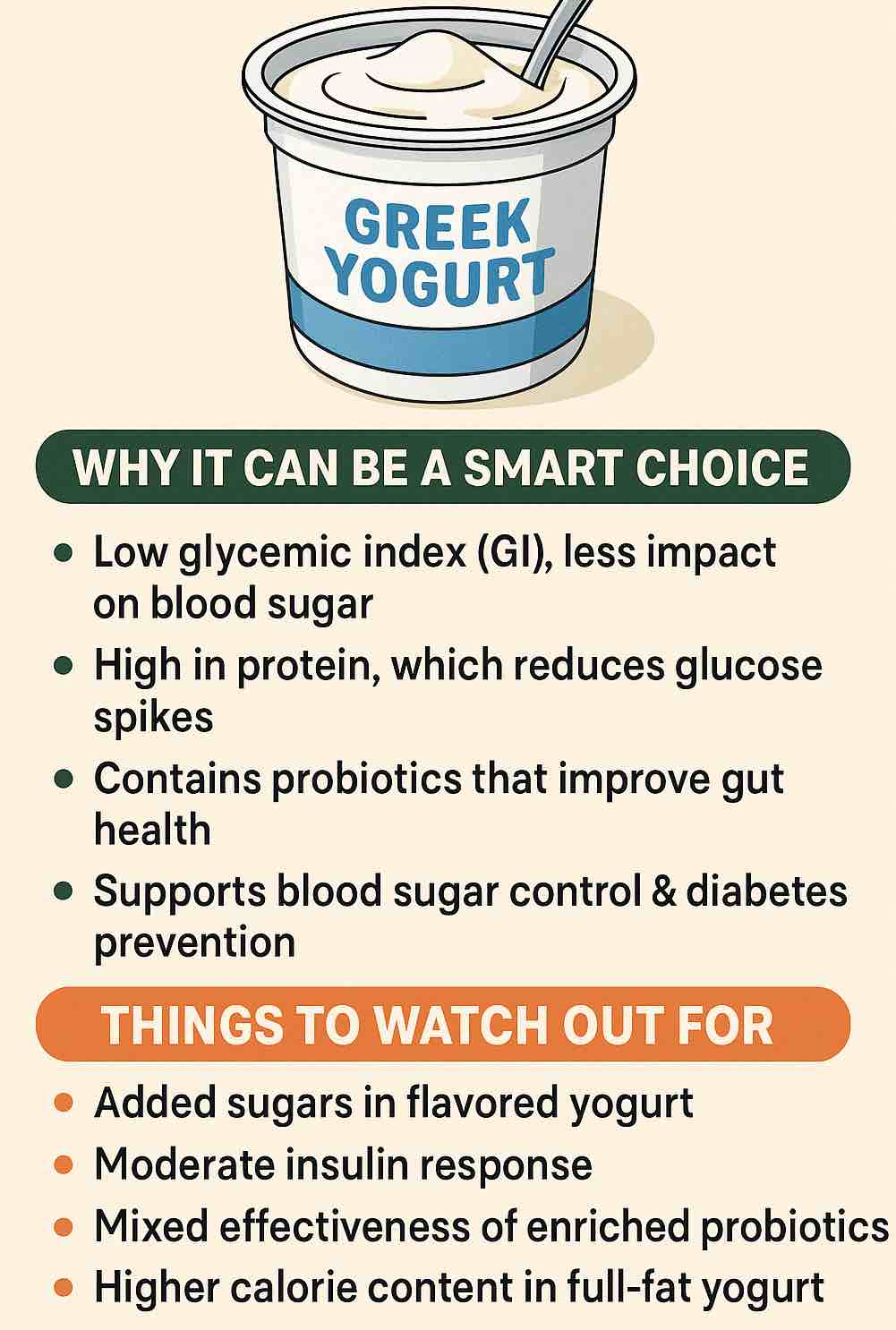
- Smoothies: Whole-berry smoothies (with seeds and pulp) are a smart way to slow sugar absorption. Add yogurt or protein powder to further flatten any glucose rise.
- Juice: Generally not recommended—juicing removes fiber and can rapidly spike blood sugar. Exception: Elderberry juice shows promise in short, controlled cycles.
5. What’s the Latest Science on Berries and Diabetes?
- Berries are linked to an 18% lower risk of developing type 2 diabetes (meta-analysis, 2024).
- Whole fruit is best: Eating fruit whole (vs. juice) does not increase diabetes risk, even for those at high risk (BYU, 2025).
- Blueberry studies are mixed: Some show significant benefit, while others see little effect on fasting glucose. Processing (fresh vs. freeze-dried) and pairing with protein may influence results.
5 Berrylicious Ways to Add Berries to Your Diabetic Diet
Get creative and have fun! Here are five deliciously practical ways to enjoy more berries, without sabotaging your blood sugar.
1. Berry & Greek Yogurt Power Parfait
Layer ¾ cup mixed berries with plain Greek yogurt (high in protein, low in sugar) and a sprinkle of chia or ground flaxseed. The combo of fiber, protein, and healthy fat makes for a perfect breakfast or snack.
2. Refreshing Berry-Spinach Salad
Toss fresh spinach or baby greens with sliced strawberries or blueberries, a handful of walnuts, and crumbled feta. Drizzle with a splash of balsamic vinegar for a sweet-savory salad that stabilizes blood sugar and delights your palate.
3. Quick-Fix Berry Chia Jam
Mash 1 cup fresh berries and simmer with 1–2 tablespoons chia seeds and a touch of stevia or monkfruit (if needed). In 10 minutes, you’ll have a spreadable, low-carb jam for whole grain toast or oatmeal—without the added sugars of store-bought jams.
4. Easy Berry Crisp (No Sugar Added)
Mix berries with a sprinkle of cinnamon and top with a blend of oats, almond flour, and chopped pecans. Bake until bubbly—serve warm with a dollop of Greek yogurt for a fiber-rich dessert.
5. Diabetic-Friendly Berry Smoothie
Blend 1 cup berries with ½ cup unsweetened almond milk, a scoop of protein powder, and 1 tablespoon nut butter. Enjoy as a meal or post-workout refuel—the fat and protein slow sugar absorption, while the berries add flavor and nutrients.
Practical Pro Tips (2025 Edition)
- Always read labels: Watch for added sugars in frozen, canned, or dried berries.
- Stick with whole berries: Whole fruit preserves fiber, which is crucial for blood sugar control.
- Pair with protein/fat: Yogurt, cottage cheese, nuts, or seeds all help minimize sugar spikes.
- Portion is key: Even the healthiest berry can spike sugar in excess; stick to ¾–1 cup servings.
- Experiment with variety: Each berry brings unique nutrients. Rotate for the full spectrum of health benefits.
Final Thoughts: Berry Bliss, Every Day
Berries aren’t just “allowed” on a diabetic diet—they’re celebrated! Loaded with antioxidants, fiber, and natural sweetness, berries satisfy cravings, support blood sugar, and add color to every meal.
Remember: It’s not about restriction, but about smart, delicious choices. With berries on your side, “diabetes-friendly” can be deliciously fun.
Want personalized berry recipes or more meal-planning tips? Drop your questions below!
10 FAQs About Berries and Diabetes
1. Can people with diabetes eat berries every day?
Yes, as long as portions are controlled (about ¾–1 cup per serving). Berries are low on the glycemic index and provide fiber and antioxidants that support blood sugar management.
2. Are frozen berries as healthy as fresh?
Absolutely. Frozen berries are picked and frozen at peak ripeness, preserving nutrients. Just ensure they are unsweetened and check the ingredient list for added sugars.
3. Should I avoid dried berries if I have diabetes?
Usually, yes. Dried berries are concentrated sources of sugar and calories, often with added sweeteners. If you eat them, use very small amounts and read labels carefully.
4. Which berries are best for diabetes?
All common berries—strawberries, blueberries, raspberries, blackberries, and even elderberries—are excellent choices. They’re all high in fiber and antioxidants, with only minor differences in sugar content per serving.
5. Are berry smoothies good for diabetics?
They can be. The healthiest options use whole berries, include protein (like Greek yogurt or protein powder), and contain no added sugars. Avoid commercial smoothies that often use juice or syrups.
6. Can I eat berries with other fruits?
Yes, but be mindful of your total carbohydrate intake. Berries are generally lower in sugar than most fruits, so mixing with high-sugar fruits (like bananas or mangoes) can increase your meal’s impact on blood sugar.
7. How do berries help with blood sugar control?
Berries are rich in fiber, which slows glucose absorption, and polyphenols (like anthocyanins), which may improve insulin sensitivity and reduce after-meal glucose spikes.
8. Are berry juices safe for people with diabetes?
Generally, no. Juicing removes most fiber and concentrates the sugar, causing a rapid blood sugar rise. Exception: New research suggests elderberry juice may have unique benefits, but it should be used with caution and not as a staple.
9. What’s the best way to sweeten berries if they taste sour?
Add a sprinkle of cinnamon or a non-nutritive sweetener like stevia, monk fruit, or erythritol. Avoid sugar, honey, or syrups, which can spike blood sugar.
10. How can I tell if a berry product is diabetic-friendly?
Read the label: Look for unsweetened, no added sugar, and minimal ingredients. Avoid products with syrups, concentrated fruit juice, or “glazed” coatings.