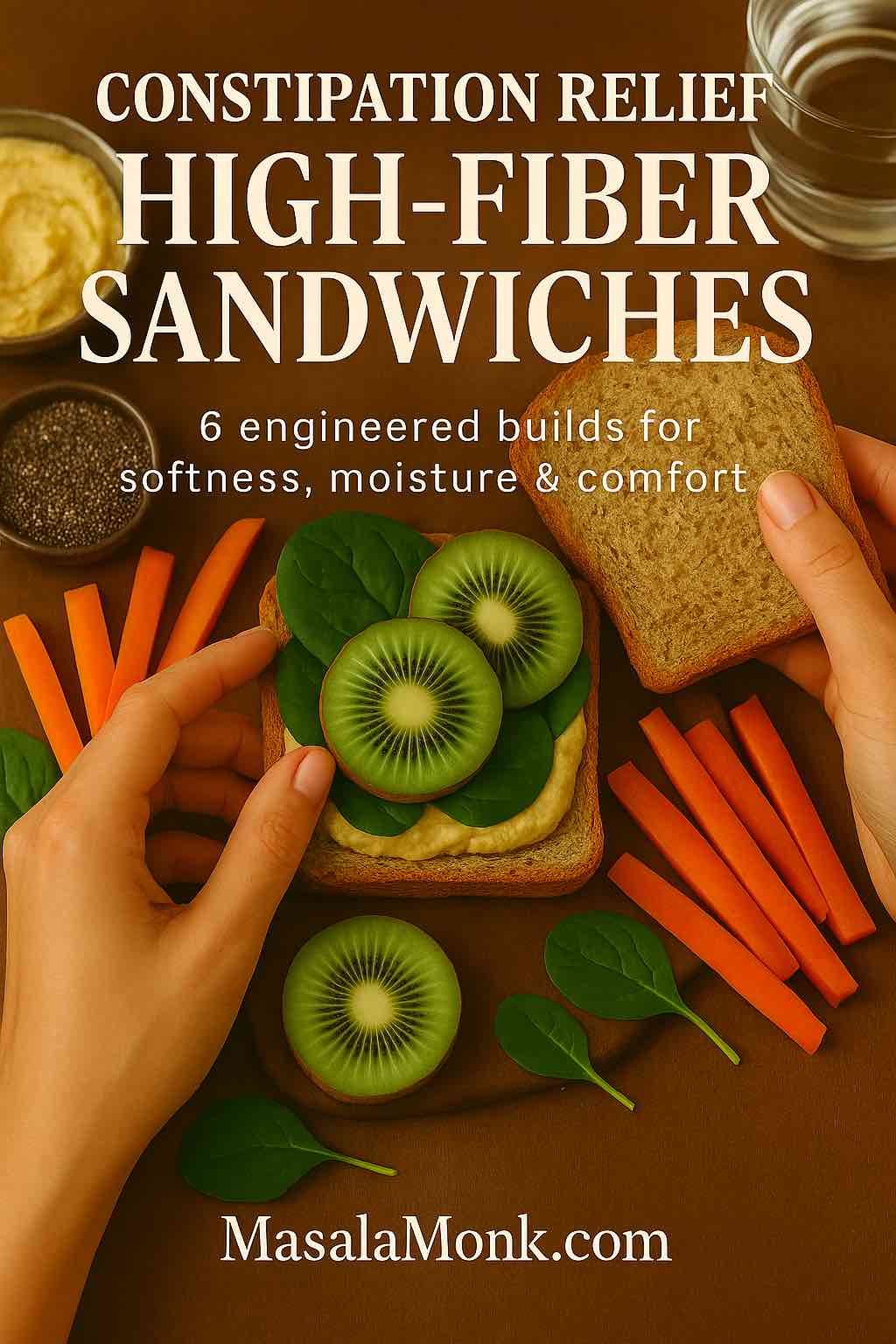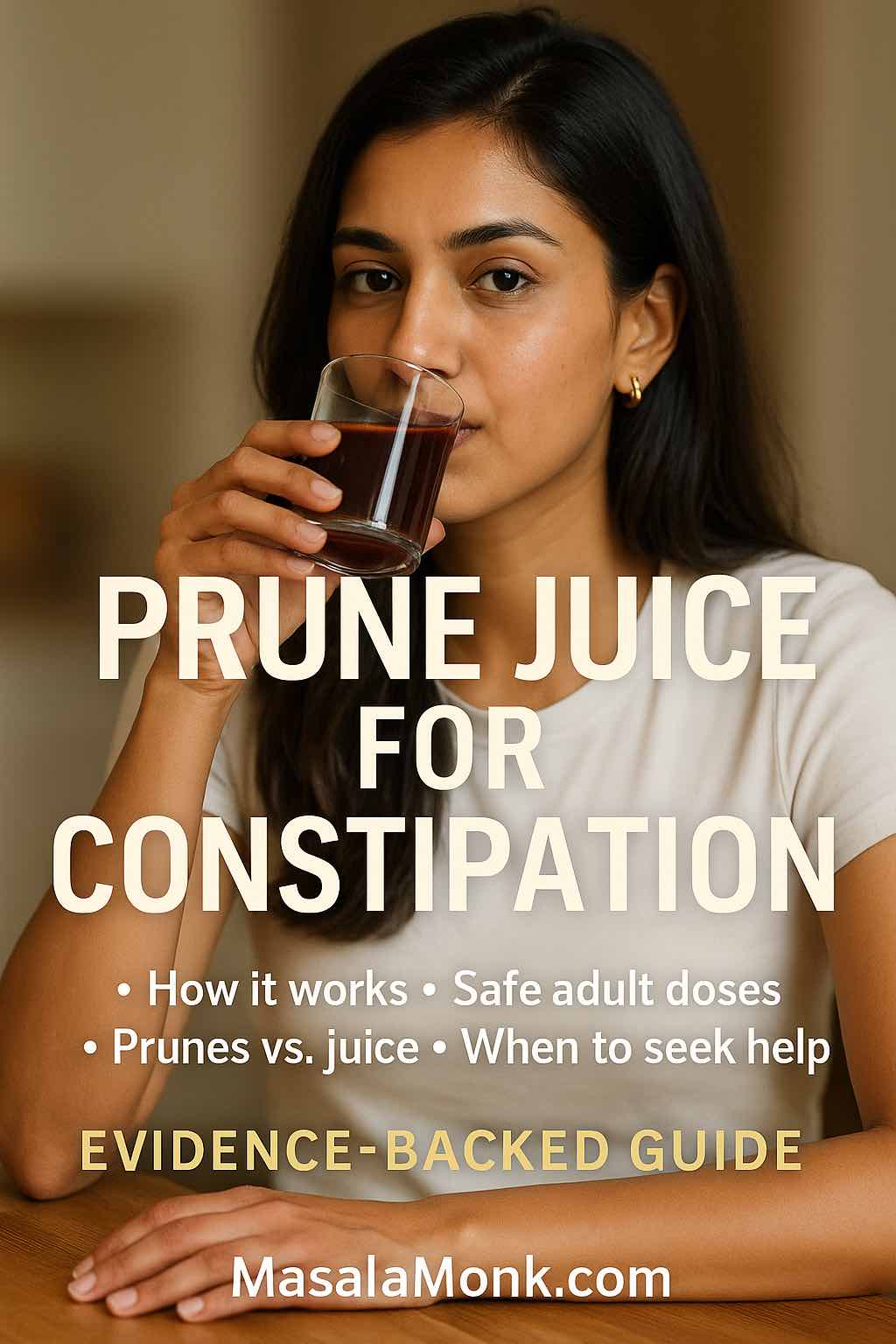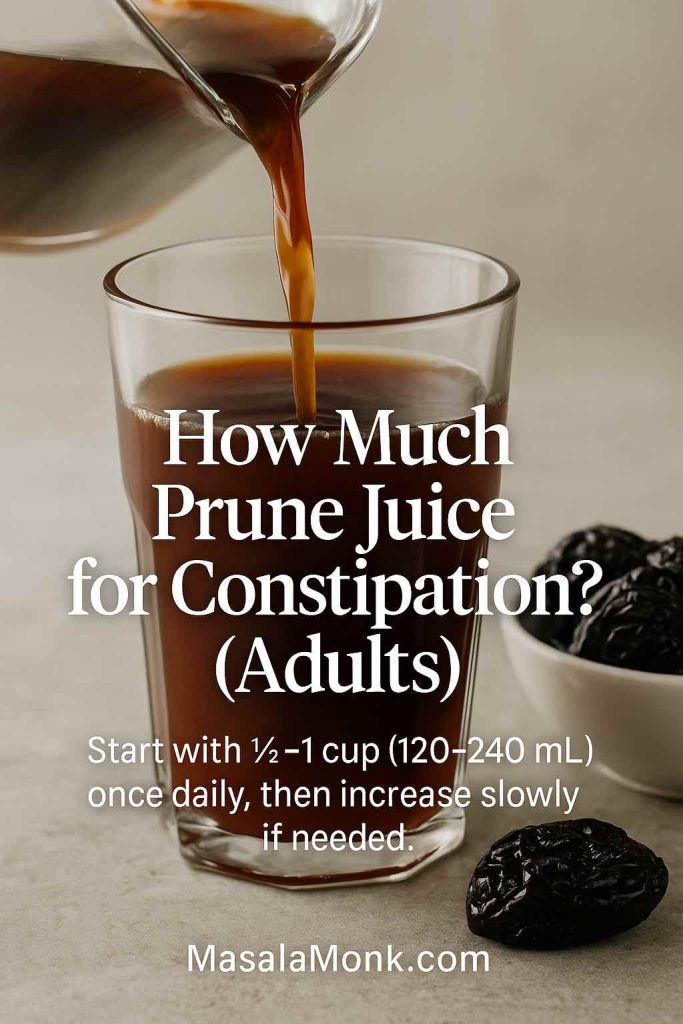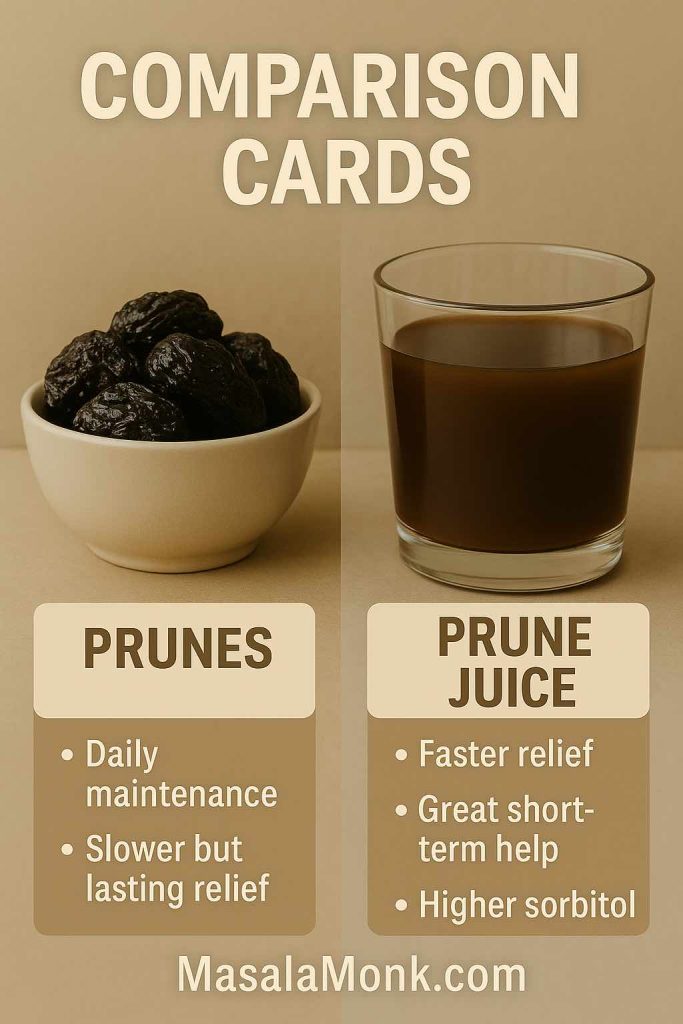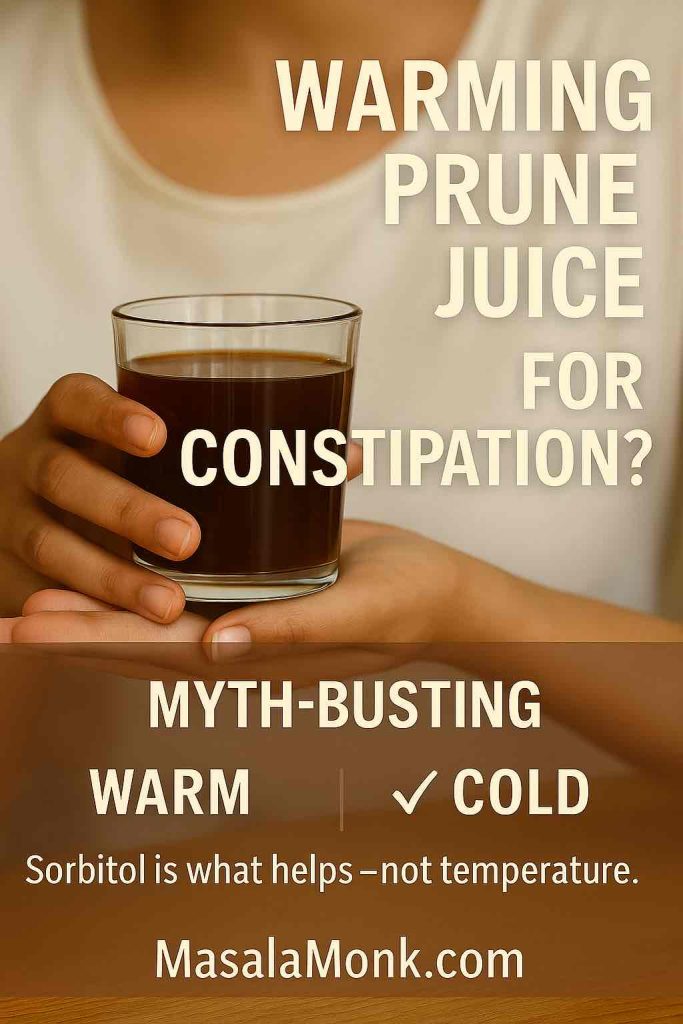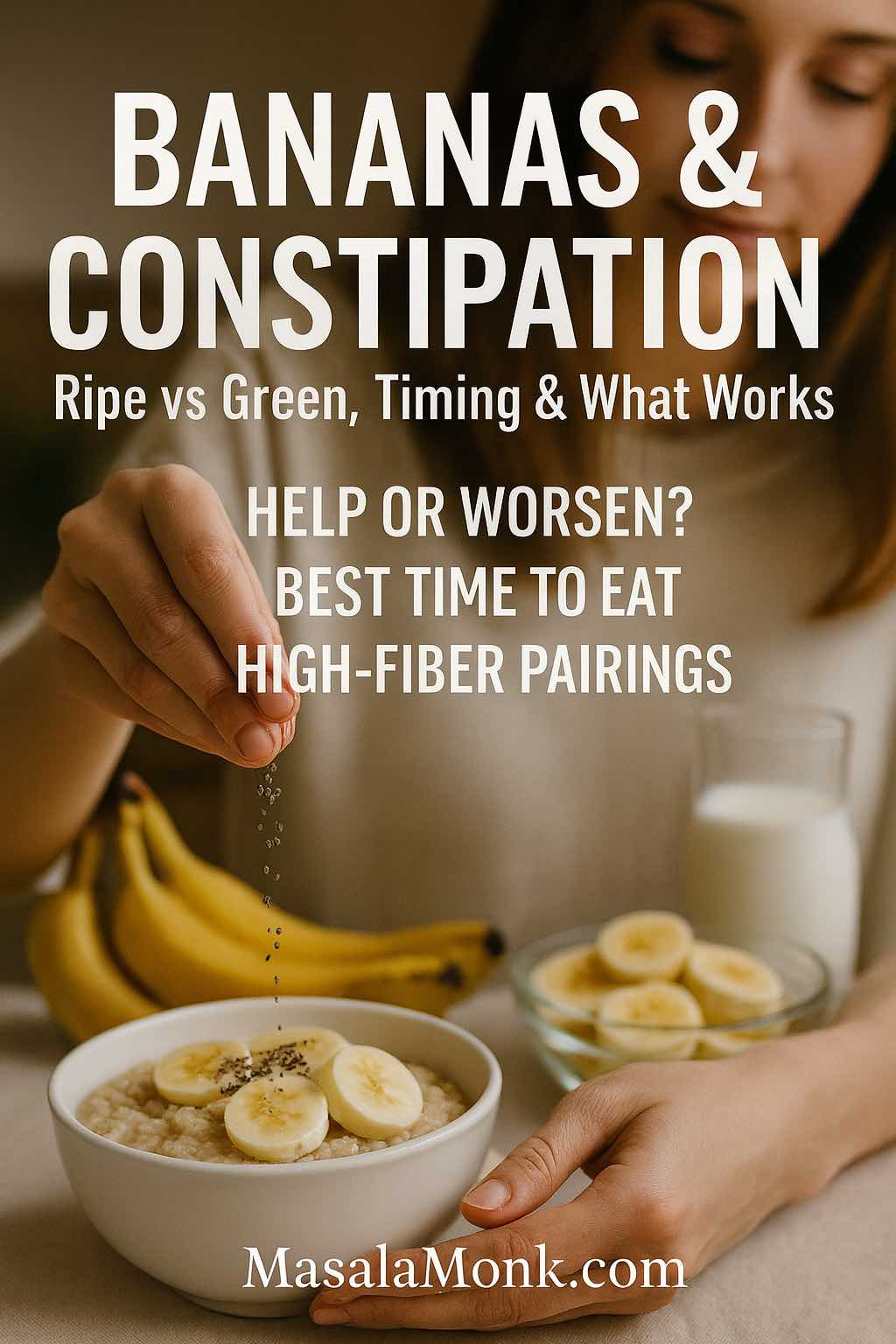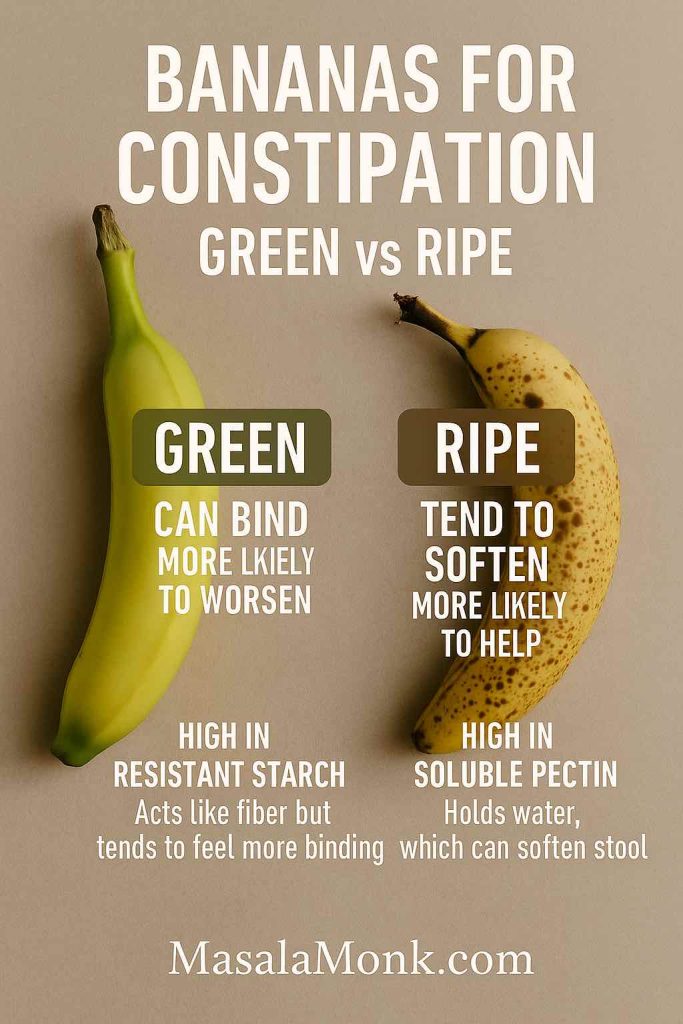
Constipation steals time, energy, and patience. If you’re here hunting for the best probiotics and prebiotics for constipation, you probably want something that works in real life—without upsetting your stomach or emptying your wallet. This guide speaks human. You’ll get a simple plan, friendly food ideas, strain names that actually matter, and clear signs it’s working. Along the way, we’ll link to evidence you can check yourself and to a few supportive reads on MasalaMonk—like prune juice & prunes: timing and how much, high-fibre sandwiches that don’t taste like cardboard, and bananas & digestion—ripe vs green, what really matters—so you can turn ideas into a routine.
Before we dive in, one honest note: probiotics can help, but they aren’t magic. Results are usually modest and strain-specific—often one extra bowel movement a week or softer, easier stools. That picture matches careful summaries of randomized trials (see the NIH overview of probiotics). By contrast, prebiotics—the fibres that feed your good gut microbes—often offer more reliable improvements in stool frequency and consistency when you choose well-studied types and increase the dose gradually (for example, a broad NDOs/GOS meta-analysis).
And if constipation keeps hanging on despite your best efforts, evidence-based care still starts with fibre and proven OTC laxatives, then steps up to prescription tools when needed. You can skim that ladder here: ACG/AGA guidance summary and the CIC pharmacologic guideline abstract.
Why gentle expectations make everything easier
When you know what “success” looks like, you can stop chasing miracle claims and start building a routine. First, effects build gradually; therefore, give each change 2–4 weeks. Second, strain matters; thus, pick probiotics that name the exact letters/numbers after the species (otherwise you’re buying a mystery). Third, measure wins kindly: +1 weekly bowel movement, less straining, or consistently softer stools are meaningful. Finally—and importantly—if you notice red flags (blood in stool, persistent severe pain, fever, unexplained weight loss), seek medical care now, not later.
Meanwhile, most people do better with a small plan that repeats daily, not a complicated overhaul. So let’s keep it simple.
Also Read: Hemorrhoids High Fiber Diet: Best Foods, What to Avoid, and a 7-Day Plan
A two-step plan using the best probiotics and prebiotics for constipation
- Step 1 — Start with a prebiotic for 2–4 weeks.
- Step 2 — If you still want support, add exactly one probiotic for 2–4 weeks.
- Step 3 — Keep what clearly helps; drop what doesn’t.
Why this order? Because prebiotics pull water into stool and feed your resident microbes—consequently softening, bulking, and improving regularity. Then, if needed, a targeted probiotic can gently amplify what’s already improving.
Also Read: Flax Seeds: The Tiny Powerhouse for Strong Digestion
The best probiotics and prebiotics for constipation—begin with the friendliest fibres
PHGG (Partially Hydrolyzed Guar Gum): easy to mix, easy on the belly
What it is (in plain English). PHGG is a soluble fibre made from guar beans, processed so it dissolves smoothly and is usually well tolerated.
Why it often helps first. It blends into tea, coffee, water, yoghurt/curd, dal, or a smoothie with minimal taste or thickness. Because it’s low-viscosity, it’s often gentler than thick fibres.
How to begin. Start with 3–5 g/day for 3–4 days; then, if you’re comfortable, increase toward 5–10 g/day. Sip water steadily rather than chugging.
What the evidence suggests. In a double-blind, 4-week trial among older adults in care facilities, PHGG significantly reduced laxative use versus placebo—practical proof of better regularity with good tolerance (PubMed summary; journal version: Clinical Nutrition ESPEN).
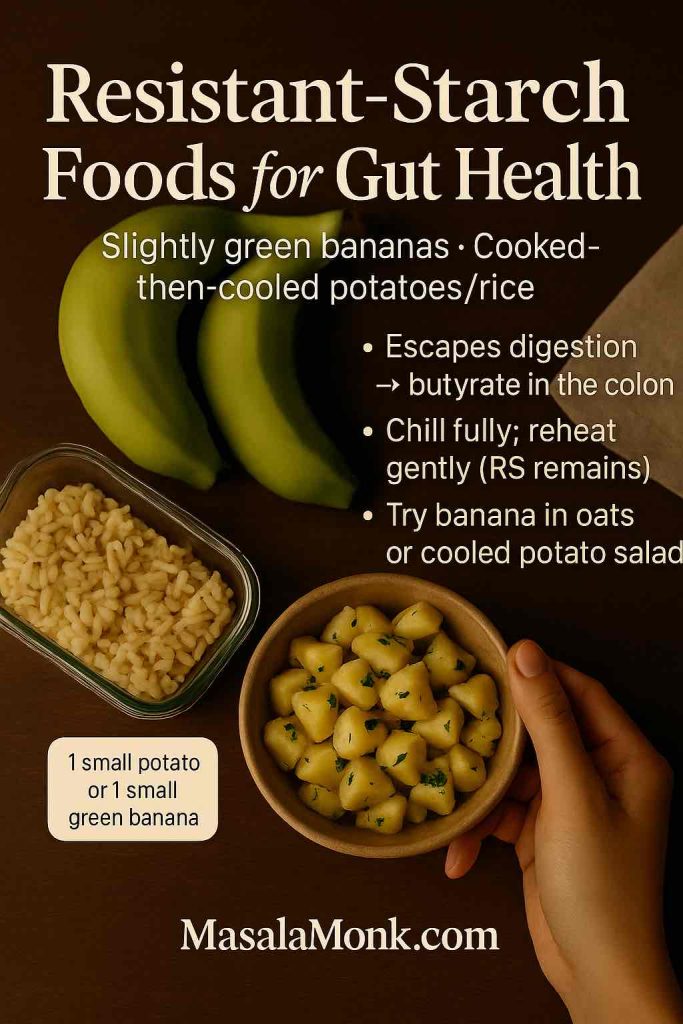
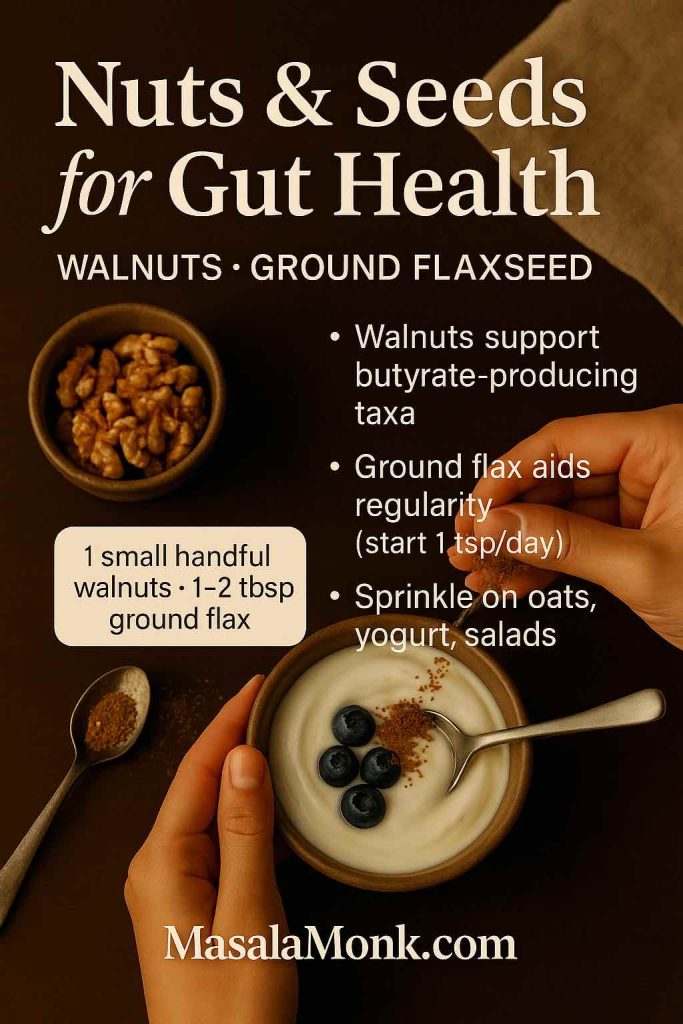
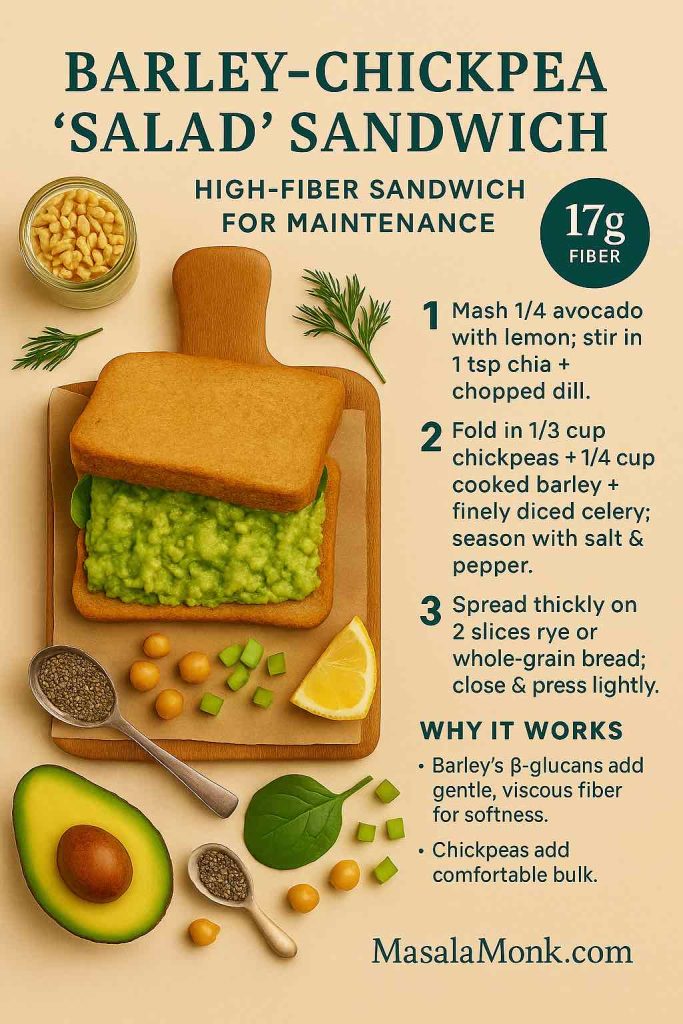
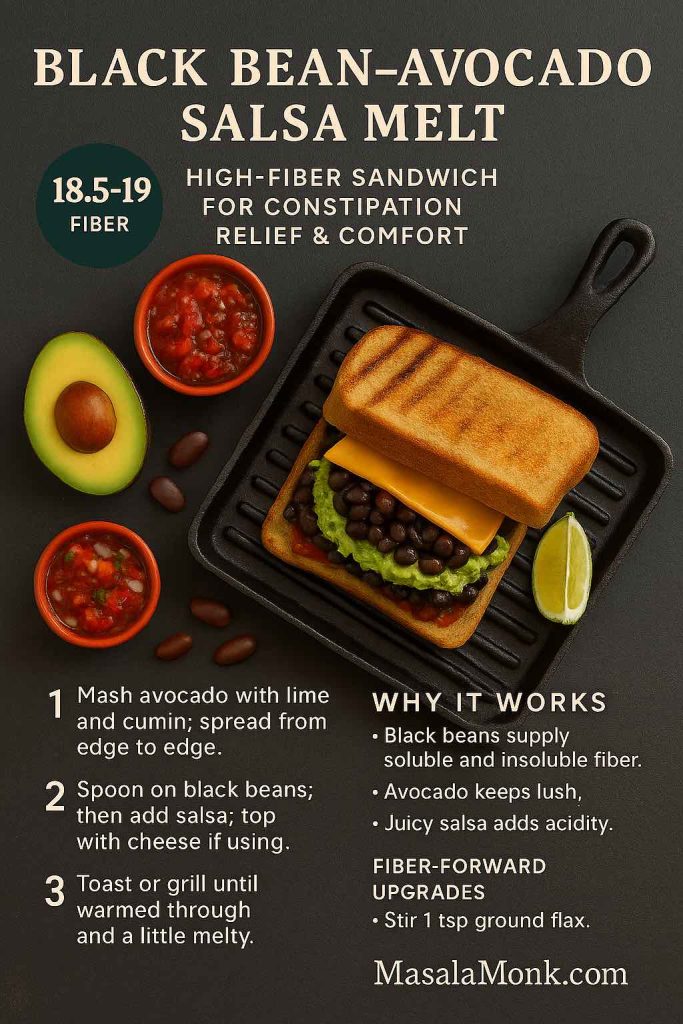
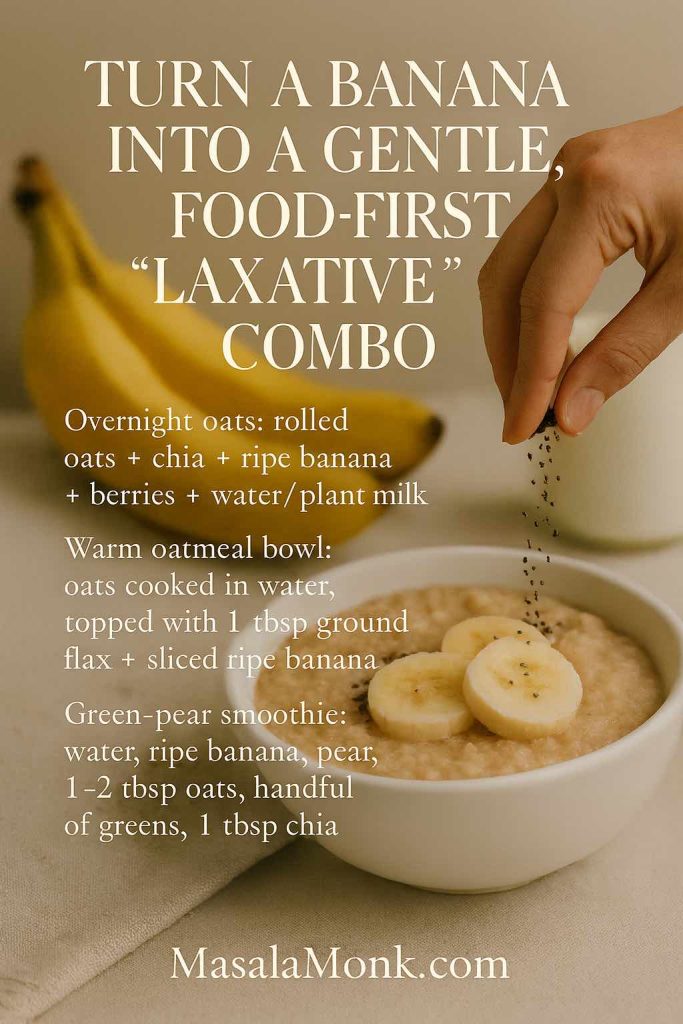
Friendly food pairings. For a comfortable start, try curd with ripe banana and flax; oats with chia and kiwi; or one of these fibre-rich sandwiches that feel like real lunch, not a chore.
Also Read: Chia Seed Water: Benefits, Recipes & Best Time to Drink for Weight Loss
GOS (Galacto-oligosaccharides): the “friendly feeder” for your microbes
What it is. GOS are small carbohydrate chains that selectively nourish beneficial gut bacteria.
Why it’s useful. It supports stool frequency and consistency and layers beautifully after PHGG once your belly feels settled.
How to begin. Start at ~5 g/day; then, if you’re comfortable, nudge toward 10–12 g/day over one to two weeks. Increase in tiny steps to reduce gas.
What the evidence suggests. An adult RCT using 11 g/day of GOS significantly increased stool frequency in people with low baseline frequency and in those with self-reported constipation (full text; PubMed). Moreover, a broader analysis across non-digestible oligosaccharides (including GOS) reports roughly one extra bowel movement per week in constipated adults (Nutrients meta-analysis).
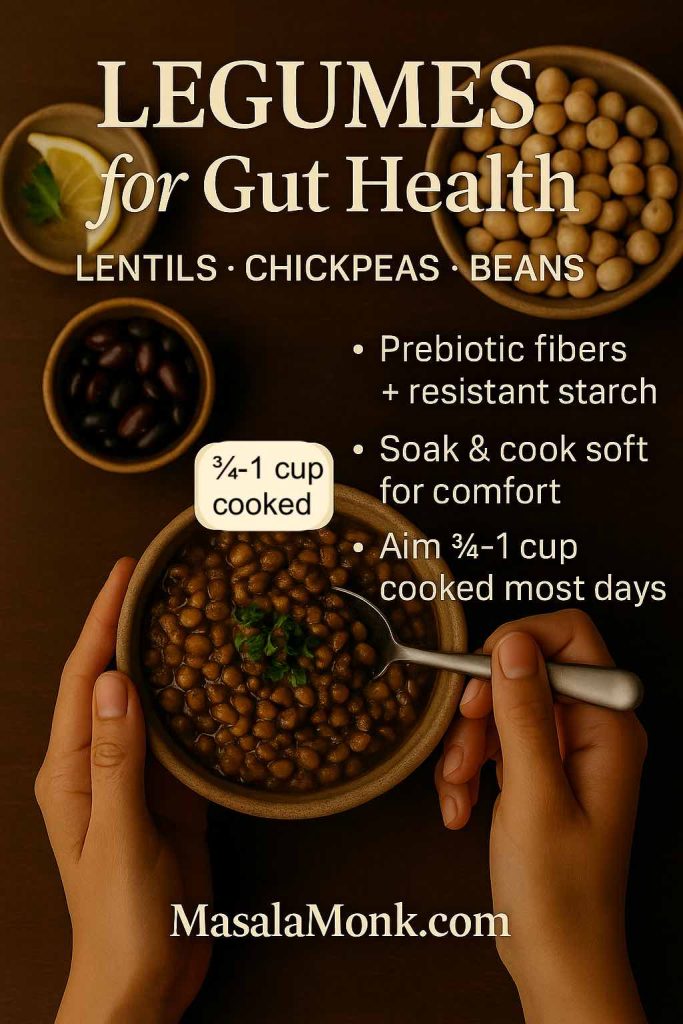
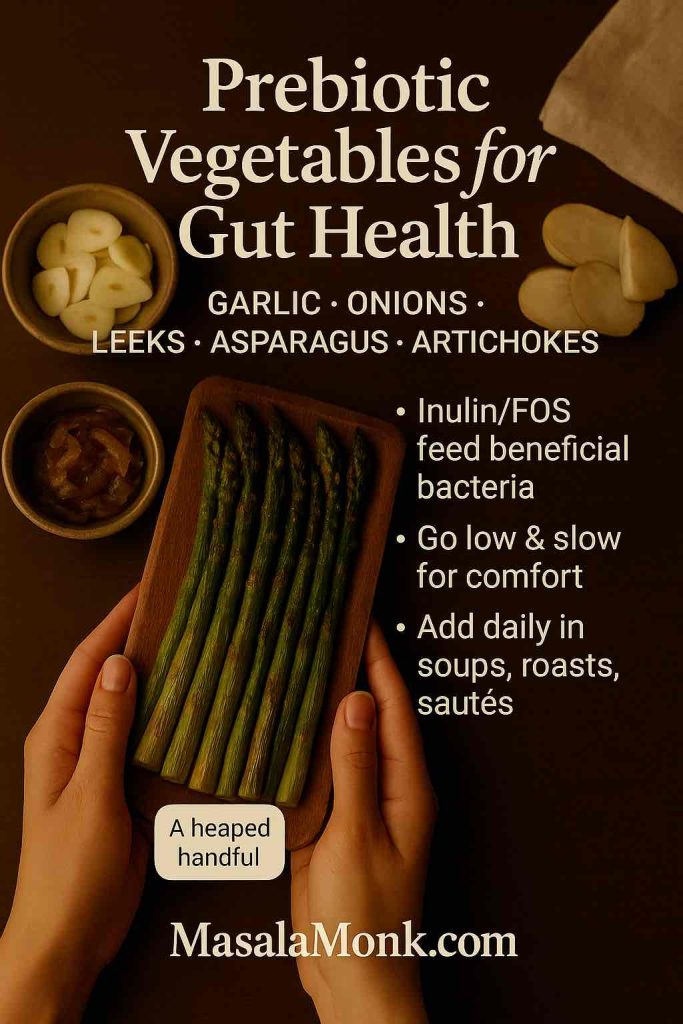
Simple kitchen support. Legumes provide natural GOS—soak chickpeas, rajma, moong, or masoor well; cook thoroughly; and season with ginger/hing. If you want a predictable nudge, match your fibre routine with prune juice at the same time daily for two weeks and see how you feel.
Also Read: Benefits of Flax Seeds and How to Incorporate Them into the Indian Diet
The best probiotics and prebiotics for constipation—choose probiotic strains that actually have data
Probiotics are “good bacteria,” yes; nevertheless, strains behave differently. Your label should show the letters/numbers after the species name (e.g., Bifidobacterium animalis subsp. lactis BB-12). If that’s missing, choose a more transparent product. Below is a plain-English shortlist of best probiotic strains for regularity with human outcomes.
| Strain (what it means for you) | Where you’ll see it | Typical daily amount | What people often notice | When to try it |
|---|---|---|---|---|
| BB-12 — a friendly Bifidobacterium that helps “move things along” | Capsules labelled BB-12; some fermented dairy | ~1–10 billion CFU | Slightly more frequent, easier stools after ~4 weeks in adult trials | First probiotic to pair with fibre (full text; PubMed) |
| HN019 — a cousin of BB-12 with mixed findings | Single-strain HN019 capsules | ~5–10 billion CFU | Earlier hints of faster transit; however, a large 2024 RCT didn’t beat placebo on the main outcome | Try only if you’ll stop quickly if no change (JAMA Network Open; PubMed) |
| DN-173 010 — a culture used in research yoghurts | Selected Activia lines (varies by country; read the carton) | One serving/day | Food-first support for transit and stool comfort in IBS-C/constipation-prone groups | Prefer yoghurt to capsules? Start here (healthy women RCT; IBS-C trial) |
| LcS (Shirota) — the Yakult strain | Yakult fermented milk | One small bottle/day | For some adults, better stool consistency and comfort | Want a tiny, repeatable habit? This fits (study page; open access) |
How long to trial a probiotic. Two to four weeks, then decide. Most RCTs use that window, which makes it a fair real-world test (for instance, see the BB-12 trial duration). If nothing changes by the end, stop or switch—no capsule museum on your shelf.
Do probiotics cause constipation? Rarely. Usually, responders report softer stools or improved frequency; even so, some people feel gassy while adjusting. If you’re not clearly better after two weeks, it’s reasonable to stop or change course (general overview: NIH ODS).
Also Read: Top 10 Foods for Gut Health (+ Pre/Probiotics, Best Drinks, Gut-Reset Plan)
A day that quietly supports regularity (and feels like real life)
Morning
- Tall glass of water on waking.
- Tea or coffee with PHGG stirred in (begin low).
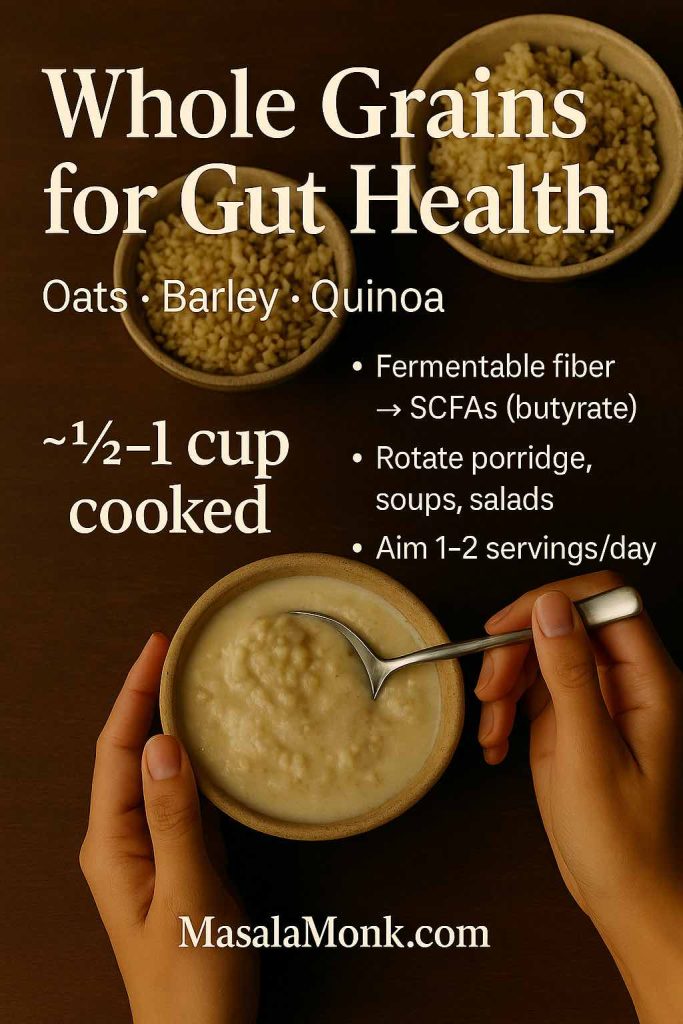
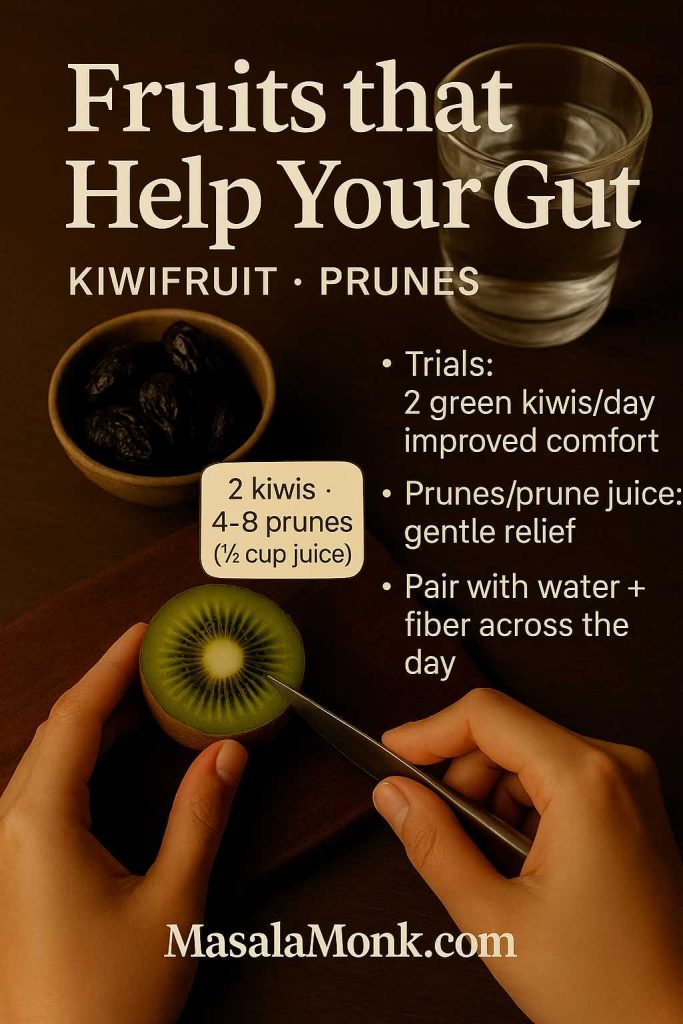
- Breakfast tilted toward soluble fibre—oats, chia, kiwi, pears, or ripe bananas (for timing tips, see bananas & digestion).
- A 10–15 minute walk to ride your natural gastro-colic reflex.
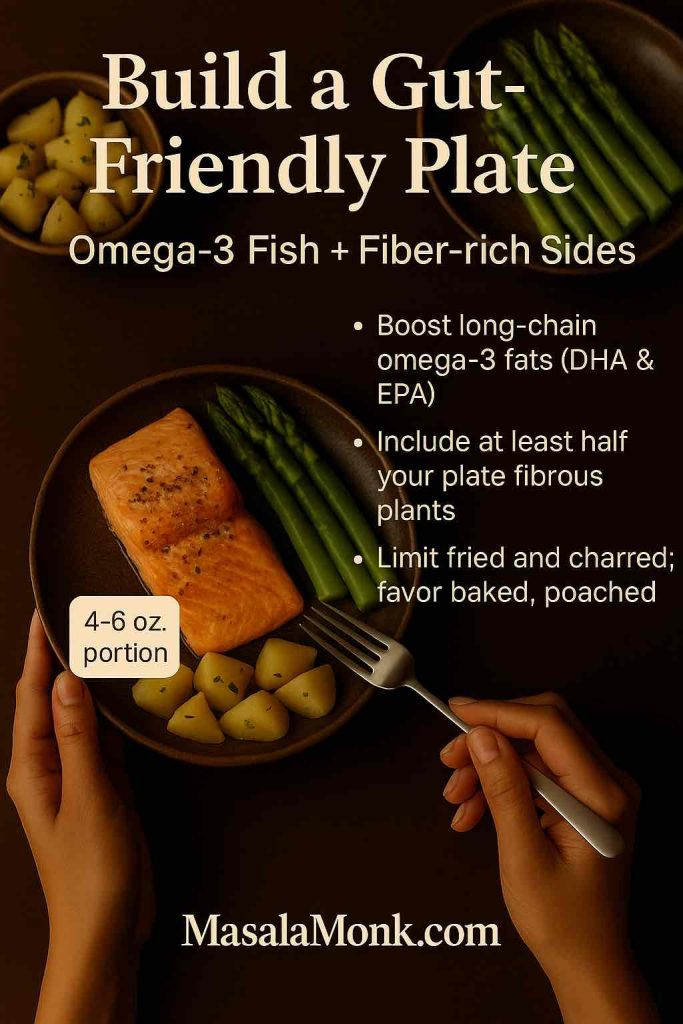
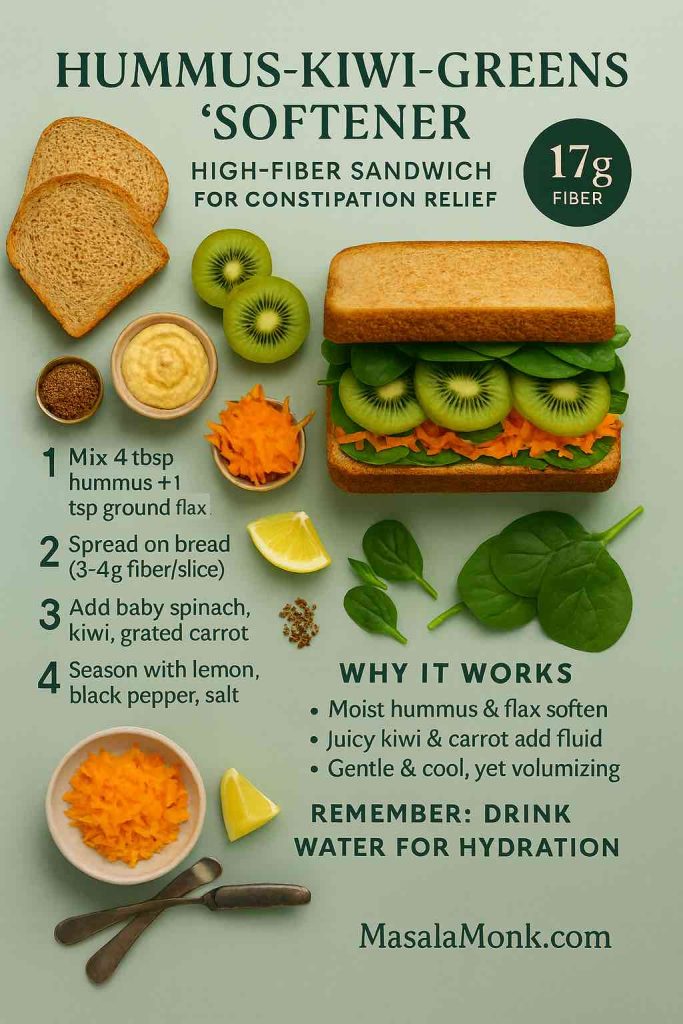
Midday - Whole-grain + bean lunch—chickpeas, rajma, or moong (soaked, well-cooked, and seasoned kindly), or one of these high-fibre sandwiches.
- Steady sips of water through the afternoon; small and frequent beats a single chug.
Evening - Veg-forward dinner with a drizzle of olive oil (a little “slip” helps).
- If you’re testing a probiotic, take one strain with food during week one.
- If it suits you, add a small prune-juice window at the same time daily.
Anytime reminders - When the urge hits, go—holding back trains the bowel to be shy.
- Light stretching or a relaxed after-dinner stroll still counts.
Also Read: Psyllium Husk (Isabgol/Ispaghula) Side Effects: Risks, Benefits & How to Take It Safely
Troubleshooting—so your belly stays comfortable
- Start low, step slow. Increase PHGG or GOS in 1–2 g steps every few days. If gas shows up, pause the increase until things settle.
- One change at a time. Find a comfortable prebiotic dose before adding a probiotic; otherwise, you won’t know what’s helping.
- Hydration matters. Fibre needs water to soften stool—keep a bottle nearby and sip throughout the day.
- Routine beats willpower. Warm drink + breakfast + short walk quietly trains a dependable rhythm.
- Spices can help. Ginger, ajwain, and jeera often make legume-heavy meals feel kinder.
Also Read: Ginger for Heartburn and Acid Reflux: Natural Relief or Digestive Myth?
Best probiotics and prebiotics for constipation—food-first ways (if you don’t want pills)
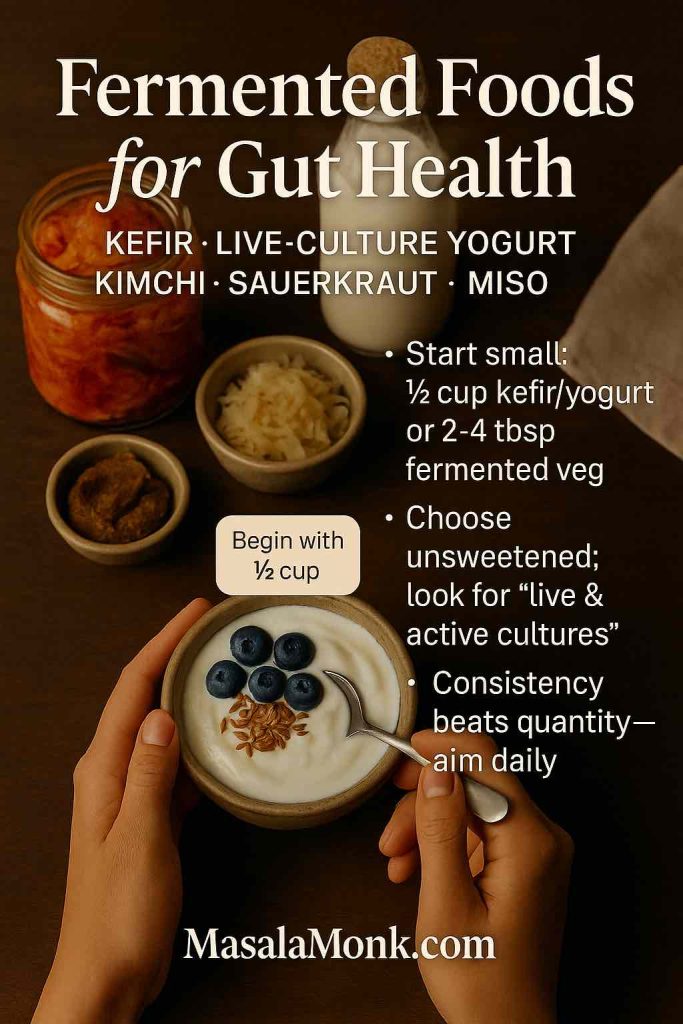
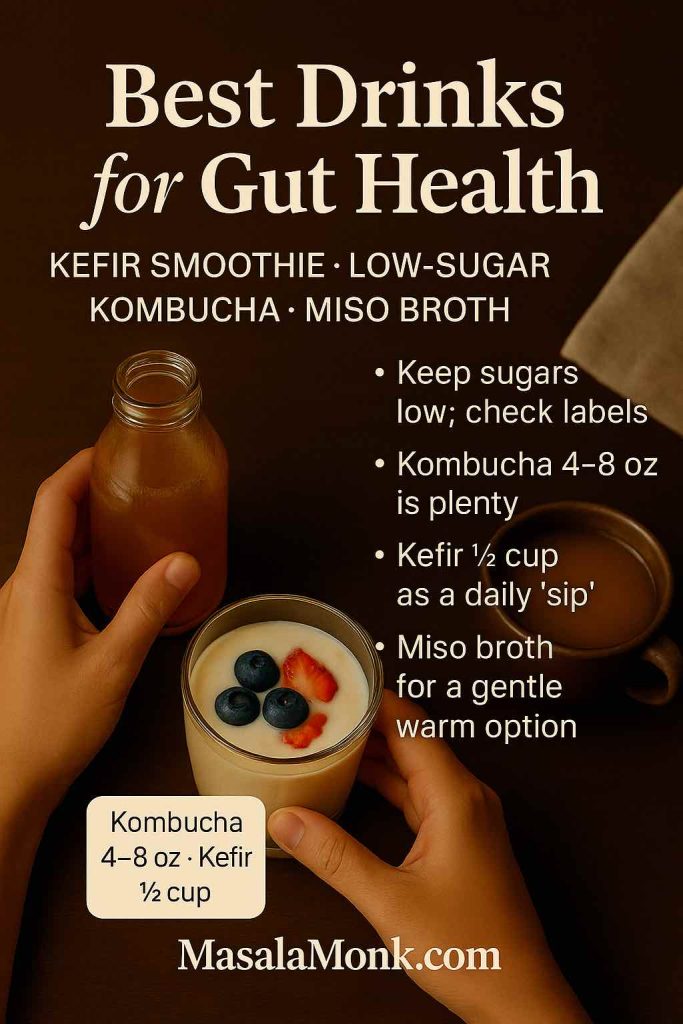
- Fermented dairy with DN-173 010 (some Activia lines). Check the carton for strain info; where available, a daily serving is an easy habit. Trials show shorter transit and better comfort in constipation-prone groups (healthy women RCT; IBS-C multicentre trial). Pair it with oats and chia to double down on soluble fibre.
- Yakult (LcS). One small bottle a day is pleasantly low effort. Several adult studies note improved stool consistency and symptom comfort (see journal page and open-access summary).
- Plain yoghurt + PHGG. Stir in a spoonful; add ripe banana or pear and a sprinkle of flax or chia.
- Legumes for natural GOS. Chana, rajma, masoor, moong—soak, cook well, and season kindly. Food provides smaller GOS amounts than powders; nevertheless, it all adds up (NDOs/GOS meta-analysis).
For more kitchen help, circle back to the sandwich ideas or schedule a small, consistent prune routine to keep things predictable.
Special situations—women, pregnancy, travel, IBS-C, iron
IBS-Constipation (IBS-C). Begin with PHGG or GOS. If you add a probiotic, consider BB-12 or a food-first DN-173 010 yoghurt where labelled. Trials suggest improvements in transit or stool comfort for some, though results vary (BB-12 trial; DN-173 010 study). Ease into legumes, then expand as comfort allows.
Pregnancy. Food-first shines: yoghurt + fruit, smaller PHGG doses, steady hydration. If you’re on iron, fibre and fluids help a lot; medication choices should be individualized within the standard care pathway (ACG/AGA overview).
Travel constipation. Pack PHGG sachets, keep your morning coffee + short walk, and stick with one probiotic you already tolerate. Travel is for maintenance—not experiments.
Iron-related constipation. Pair iron with vitamin-C-rich foods (citrus, guava, capsicum), keep your fibre rhythm, and ask your clinician about gentler iron forms if you’re struggling.
Also Read: Iron Deficiency Anemia Symptoms: 15 Signs You Are Iron Deficient
How to shop without second-guessing every label
- PHGG. Search for “Partially Hydrolyzed Guar Gum” or the raw-material name “Sunfiber.” Neutral taste; mixes into almost anything.
- GOS. Look for “Galacto-oligosaccharides” or “GOS prebiotic powder.” Legumes and some dairy provide small natural amounts; however, powders make it easier to reach study-level doses (GOS RCT—11 g/day).
- Probiotics for regularity. Choose products that state the exact strain (e.g., BB-12, HN019). If a label only says “Bifidobacterium” or “Lactobacillus” without letters/numbers, pick something more specific.
- Probiotic foods for constipation. Where available, Activia lines listing DN-173 010 and Yakult for LcS have human data behind them (DN-173 010 studies; IBS-C trial; Yakult data).
If you want food-forward routines, revisit prunes & prune juice and our high-fibre sandwich guide—small, steady choices that make the rest of this plan easier.
Also Read: Significance of Fiber in Diet: Understanding Its Health Benefits
A 28-day, no-stress plan using the best probiotics and prebiotics for constipation
Days 1–3 — Start gentle
- PHGG 3–5 g once daily in a warm drink you already have.
- Regular water sips.
- 10–15-minute walks after meals.
- Quick log: frequency, comfort, gas.
Days 4–14 — Find your comfortable dose - If you’re fine, nudge PHGG toward 5–10 g/day.
- Prefer GOS? Begin 5 g/day, then ease toward 10–12 g/day as comfortable.
- Layer a food nudge: yoghurt + chia, kiwi or pear, or a small prune-juice window at the same time daily.
Days 15–28 — Add one probiotic (only if you still want more support) - Choose one: BB-12 capsule, a DN-173 010 yoghurt (where labelled), or Yakult (LcS).
- Take it with food during week one.
- By day 28, decide with clarity: keep what clearly helps; drop what doesn’t. If you trial HN019, manage expectations— a large 2024 RCT didn’t meet its primary endpoint on complete spontaneous BMs (JAMA Network Open).
Also Read: Kiwi Fruit: Nutrition, Benefits, and How to Eat It 🥝🌱
When to escalate (and why that’s absolutely okay)
If you’ve given this plan an honest try and you’re still struggling, there’s no shame in getting more help. Over-the-counter polyethylene glycol (PEG) is strongly recommended and can make a clear difference; if that’s not enough, prescription options like linaclotide, plecanatide, or prucalopride have robust evidence and often change lives (clinical guidance summary; guideline abstract). Please seek care promptly for red flags such as blood in stool, persistent severe pain, fever, or unexplained weight loss.
Also Read: How to Make Lentil Patties that Are Better Than Meat? Vegan Protein-Rich Recipe
Bottom line
The best probiotics and prebiotics for constipation are the ones you can use consistently without turning your life upside down. A gentle prebiotic (PHGG or GOS), optionally one well-chosen probiotic, everyday movement, steady hydration, and familiar meals—together, these small habits usually shift you from stuck to steady. And if progress stalls, there’s a clear, evidence-based next step.
For practical food support alongside this plan, keep these open: prune timing & dose, high-fibre sandwiches, and bananas & digestion—ripe vs green. Keep it small, steady, and kind—your gut will thank you.
FAQs
1) What are the best probiotics and prebiotics for constipation, in plain English?
To begin with, prebiotics like partially hydrolyzed guar gum (PHGG) and galacto-oligosaccharides (GOS) often deliver steady improvements in stool frequency and softness. Then, for many people, adding a strain-specific probiotic—such as BB-12, DN-173 010 (in select yogurts), or LcS (Shirota)—provides a gentle extra nudge. Importantly, choose one product at a time, dose low, go slow, and give your gut 2–4 weeks before judging results.
2) Prebiotic vs probiotic for constipation—which should I try first?
Generally, start with a prebiotic because it draws water into the stool and feeds your existing good bugs; consequently, it often softens and regularizes bowel movements without much fuss. Afterward, if you want more support, add one targeted probiotic for a short trial. In short: fiber first, then a strain with evidence.
3) What’s the best probiotic for regularity if I want a simple choice?
If you prefer a straightforward option, BB-12 is a common pick for regularity; meanwhile, people who like food-first approaches sometimes choose DN-173 010 yogurt or a daily LcS drink. Nevertheless, responses vary, so evaluate honestly after a few weeks and keep only what clearly helps.
4) Which probiotic strains for constipation are worth knowing?
A practical short list includes: Bifidobacterium animalis subsp. lactis BB-12; B. animalis DN-173 010; and Lacticaseibacillus paracasei Shirota (LcS). Conversely, some strains help IBS symptoms broadly without always changing stool frequency. Therefore, check the label for exact strain names and avoid products that hide them.
5) Do probiotics cause constipation, or do they help you poop?
Usually, probiotics do not cause constipation; instead, they may modestly improve stool frequency and comfort. However, some folks feel gassy during the first week. Consequently, start low, take with food at first, and reassess after 2–4 weeks. If things don’t improve, there’s no harm in stopping.
6) What’s the best prebiotic for constipation if I’m sensitive to bloat?
For many, PHGG is the “easy-mixer” that’s gentle and dissolves well. Similarly, GOS supports stool frequency, though you may want to increase in tiny steps. Moreover, sip water across the day; fiber works best when well hydrated.
7) Is there a best probiotic for female constipation?
Women can use the same evidence-backed strains—BB-12, DN-173 010, or LcS—paired with PHGG or GOS. Nonetheless, iron supplements or hormonal shifts may change bowel rhythm, so, consequently, keep an eye on triggers (iron timing, coffee routine, travel, stress) while testing your probiotic.
8) What about the best probiotic for IBS-constipation (IBS-C)?
With IBS-C, start gently with PHGG or GOS, then layer one strain—commonly BB-12 or a food-first DN-173 010 yogurt—once gas feels manageable. Additionally, consider a small daily walk and a consistent breakfast routine to train timing. Ultimately, keep the least complicated combo that works.
9) Which is better: prebiotic or probiotic for constipation if I can only choose one?
If you must choose, opt for a prebiotic first—because, as a rule, it’s more predictable for stool softness and frequency. Even so, if you already tolerate a specific probiotic and feel it helps, stick with that single winner.
10) How long until the best probiotics and prebiotics for constipation start working?
Typically, prebiotics show benefits within 1–2 weeks, while probiotics may take 2–4 weeks. Therefore, pick one change at a time, track how often you go, and use a simple “comfort score” so you can see progress clearly rather than guessing.
11) What’s the best probiotic for bloating, gas, and constipation—can one product do it all?
Sometimes, yes—but set expectations kindly. BB-12 or LcS may help comfort and stool form, yet bloating can also reflect dose or diet pace. Accordingly, increase prebiotics in small steps, chew slowly, and consider short post-meal walks to minimize trapped gas.
12) Are probiotic foods for constipation (like yogurt drinks) as good as supplements?
Often they’re easier to use consistently. For instance, a daily serving of a yogurt cultured with DN-173 010 or a small LcS drink can be “no-brainer” habits. Conversely, if you need tight dose control or prefer dairy-free, a capsule plus PHGG may feel cleaner.
13) What’s the best probiotic for constipation and weight loss?
There isn’t a single “weight-loss probiotic” that also guarantees regularity. Nevertheless, people sometimes find that when their bowels are regular, they feel lighter and less bloated. Consequently, prioritize regularity first with PHGG or GOS, then consider lifestyle tweaks for body composition.
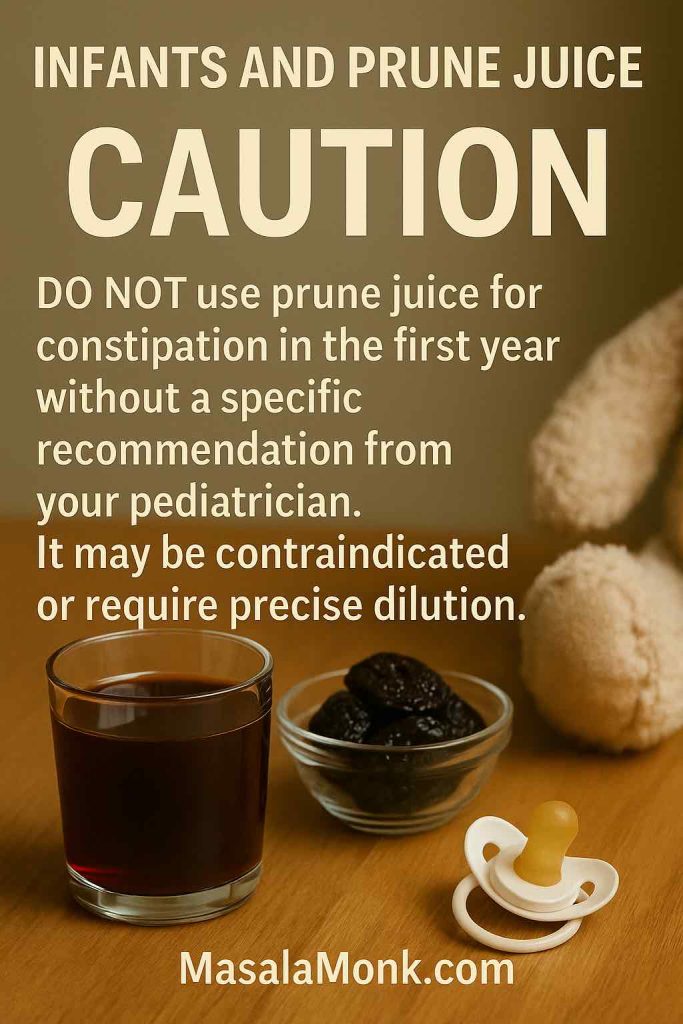
14) Can I use probiotics for newborn or infant constipation?
Infant guts are different; therefore, speak with your pediatrician before using any drops or powders. Moreover, feeding patterns, hydration, and formula type often matter more than a probiotic alone at that age.
15) Are there best probiotics for constipation during pregnancy?
During pregnancy, begin with food-first moves plus modest PHGG, and review any probiotic or supplement with your obstetric provider. Additionally, iron can tighten things up; timing doses and pairing with fiber-rich meals may help. Above all, keep changes gentle and well supervised.
16) What’s the best probiotic for gas and constipation if I’ve tried psyllium and felt worse?
Alternatively to thick fibers, consider PHGG or GOS first, then test one strain (for example, BB-12). Meanwhile, use tiny dose steps and steady hydration. If psyllium felt heavy, low-viscosity prebiotics are often better tolerated.
17) Do probiotics help with regular bowel movements if my problem is “hard stools” more than frequency?
Yes—sometimes the stool becomes easier to pass even if frequency barely changes. Therefore, measure “ease of passage” and straining, not just count. Additionally, PHGG or GOS often soften stool; afterward, a probiotic may add comfort rather than a big frequency jump.
18) Is there a best probiotic for constipation and IBS-bloating when I travel?
For travel, keep it simple: PHGG sachets and one familiar probiotic strain (not a new one). Consequently, combine with a morning routine—warm drink, small breakfast, quick walk—to trigger the gastro-colic reflex despite schedule changes.
19) What’s the best OTC probiotic for constipation if I’m shopping fast?
Choose a product that clearly lists the strain and CFU, e.g., BB-12 or LcS, and avoid mystery blends. Additionally, pair it with a measured prebiotic—PHGG or GOS—so you can adjust by the gram. Ultimately, the winner is the product you can use daily without side effects.
20) Which prebiotic vs probiotic for constipation works best for “hard stool” days?
On hard-stool days, prioritize prebiotics (PHGG or GOS) because of their water-holding and stool-softening effects. Then, once comfortable, add a probiotic for added regularity. Importantly, sip water throughout; fiber needs fluid to do its job.
21) What’s the best women’s probiotic for constipation if I’m also dealing with PMS-related swings?
Women often do well with the same strains (BB-12, DN-173 010, LcS). Nevertheless, hormone fluctuations can alter gut rhythm. Accordingly, keep your routine steady—prebiotic dose, breakfast timing, brief walks—and judge your probiotic across a full cycle for a fair read.
22) Can probiotics help you poop if stress is the trigger?
Sometimes, yes; however, stress often slows motility through the gut-brain axis. Consequently, pairing a simple breathing practice or a short after-meal stroll with your prebiotic/probiotic routine can make the difference between “some days” and “most days.”
23) What’s the best probiotic for bowel regularity if I’m lactose-sensitive?
Consider a lactose-free capsule strain (e.g., BB-12 in a dairy-free format), plus PHGG. Alternatively, try plant-based yogurts fortified with specific cultures—provided the strain names are disclosed and you tolerate the base.
24) Do I need a probiotic stool softener, or will fiber be enough?
Usually, fiber (PHGG or GOS) is the first and most dependable stool-softener. Meanwhile, a probiotic may make bowel movements feel easier, particularly if your stool is already trending softer. Therefore, keep the probiotic as a complement—not the only tool.
25) Which is the best probiotic to help poop quickly before an important day?
Realistically, probiotics are not “quick fix” tools; they’re steady-builders. If you need immediate relief, that’s a different category (e.g., osmotic laxatives under guidance). For sustainable rhythm, stick with prebiotic first, then a proven strain; consequently, you’ll rely less on last-minute tactics.
26) Are probiotics for SIBO constipation a good idea?
It depends. Some people with SIBO feel worse with certain strains or doses. Thus, start with prebiotic steps cautiously—or pause them if you flare—then consult a clinician for targeted care. In short, SIBO is a “go slow, personalize” scenario.
27) What’s the best probiotic for constipation and IBS-C bloating if my belly is sensitive?
Choose the lowest-friction path: PHGG in tiny steps, then one strain (BB-12 or LcS) at a low CFU to start. Additionally, reduce speed-eating, add a 10-minute walk after meals, and keep carbonated drinks modest while you test.
28) Should I use prebiotics and probiotics together for constipation, or separately?
You can use them together; however, to pinpoint what helps, it’s wiser to stage them: prebiotic first for 2–4 weeks, then add one probiotic. Consequently, you’ll know what to keep long-term without paying for extras you don’t need.
29) What’s the best probiotic for constipation during travel when food is unpredictable?
Pick the strain you already tolerate (for example, LcS or BB-12) and bring PHGG sachets. Moreover, anchor your mornings with a warm beverage, light breakfast, and a short walk; that routine often matters more than the specific cuisine of the day.
30) Final takeaway: how do I decide my personal best probiotics and prebiotics for constipation?
Start small with PHGG or GOS, give it a fair two-week run, and track comfort plus frequency. Then, if you still want support, add one strain—BB-12, DN-173 010, or LcS—and reassess at 2–4 weeks. Ultimately, keep the fewest things that work, so your gut—and your routine—feel calm, predictable, and genuinely sustainable.