In the world of skincare, few natural ingredients can boast both thousands of years of Ayurvedic tradition and the backing of modern clinical studies. Amla (Emblica officinalis), also known as Indian Gooseberry, stands out as one such rare gem. Revered for centuries in India as a healing powerhouse, Amla is now gaining well-deserved global recognition for its profound benefits for facial skin health and overall dermal wellness.
In this comprehensive guide, we will dive into:
- The rich nutritional profile of Amla
- Its scientifically validated skin benefits
- How it works on a cellular level
- Various ways to incorporate Amla into your skincare routine
- Precautions, tips, and real-world application advice

What is Amla?
Amla is a small, green fruit native to India and parts of Southeast Asia. The fruit has a tart, slightly bitter taste and is traditionally consumed fresh, dried, pickled, or as juice or powder.
In Ayurveda, Amla is classified as a Rasayana — a rejuvenating tonic believed to promote longevity, immunity, and vitality. But it’s not just traditional medicine singing its praises — recent scientific studies have validated many of Amla’s skin-friendly properties.
The Nutritional Powerhouse
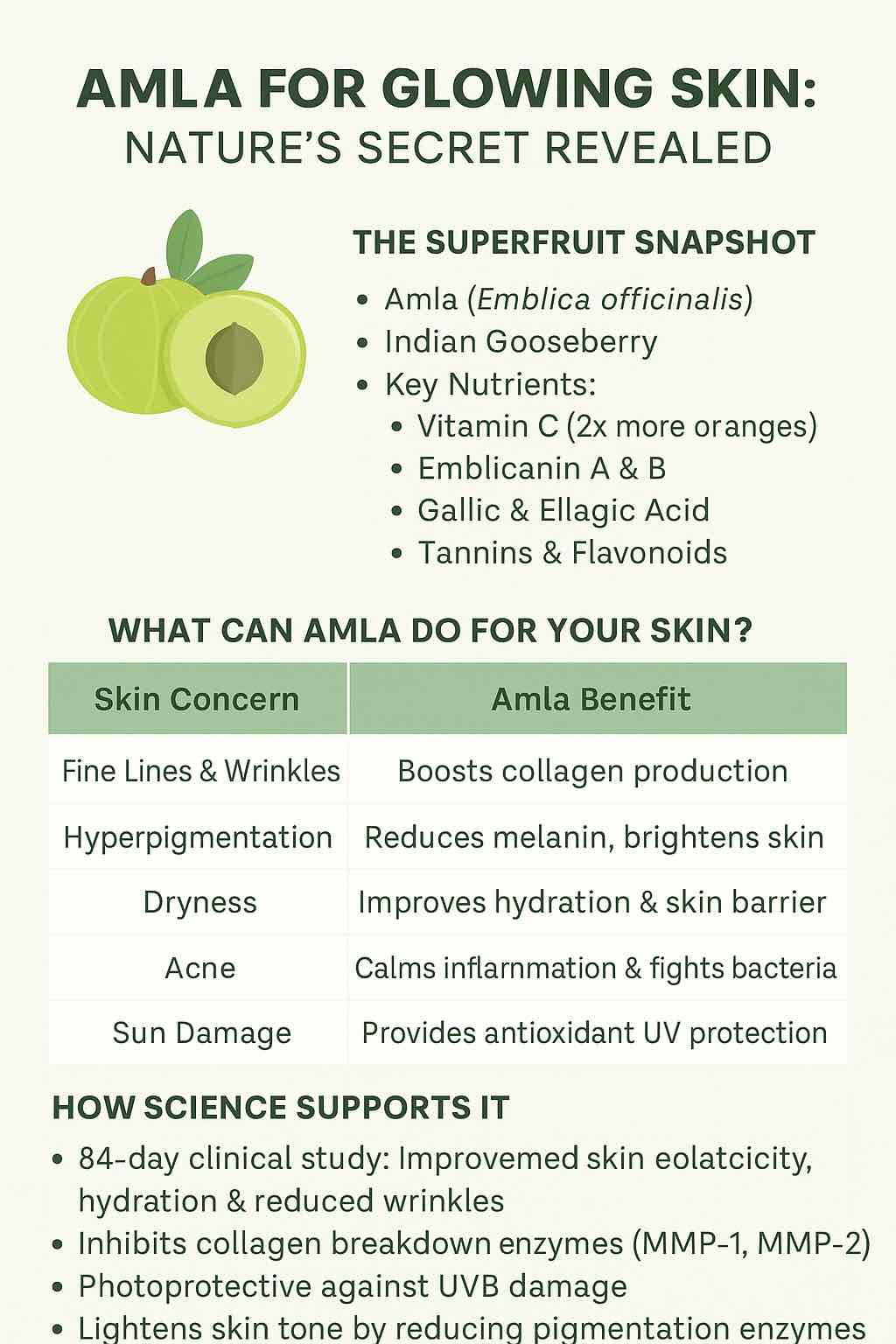
At the heart of Amla’s remarkable skin benefits lies its unmatched nutritional content:
| Compound | Benefits |
|---|---|
| Vitamin C (ascorbic acid) | Potent antioxidant, collagen synthesis booster |
| Emblicanin A & B | Long-lasting antioxidant protection |
| Gallic acid, ellagic acid, quercetin | Anti-inflammatory, brightening, DNA protection |
| Tannins, polyphenols, flavonoids | Neutralize free radicals, support skin health |
| Amino acids, minerals | Cellular repair, hydration, and metabolic balance |
With up to 20 times more vitamin C than oranges, Amla is one of the richest natural sources of ascorbic acid, making it a superb agent for skin health.
Summary of research-backed skin benefits
| Benefit | Evidence Source |
|---|---|
| ↓ Wrinkles, ↑ elasticity/hydration | 84-day topical gel clinical trial |
| ↑ Collagen / ↓ collagen breakdown | In vitro studies on procollagen & MMP inhibition |
| ↓ UV-induced damage, ↓ pigmentation | Peptide combination study |
| ↑ Skin brightness, ↓ acne | Oral juice + blood purification |
| ↑ Hydration, thickness, ↓ fine lines | Oral supplementation studies |
The Science-Backed Skin Benefits of Amla
1️⃣ Potent Antioxidant and Anti-Aging Agent
- Amla combats oxidative stress by neutralizing free radicals that cause premature aging, sagging, and wrinkles.
- It inhibits matrix metalloproteinases (MMPs), the enzymes that break down collagen and elastin fibers in the skin.
- Amla extract has been shown to stimulate procollagen synthesis, promoting youthful skin structure.
📊 Clinical studies on topical application of Amla extract demonstrated significant improvement in skin elasticity, hydration, and reduction of fine lines over a 12-week period.
2️⃣ Brightening and Pigmentation Control
- Amla inhibits melanin production by downregulating the enzyme tyrosinase.
- Its polyphenols, such as gallic acid and ellagic acid, contribute to a more even skin tone and reduced dark spots.
📊 In a controlled clinical trial, a 0.1% Amla extract gel visibly lightened skin pigmentation and improved overall complexion.
3️⃣ Hydration and Skin Barrier Support
- Amla helps improve epidermal hydration by supporting natural moisturizing factors (NMF) and lipids.
- It strengthens the skin barrier, reducing transepidermal water loss and maintaining plumpness.
4️⃣ UV Protection and DNA Repair Support
- Combined with collagen peptides, Amla has shown photoprotective properties in studies, reducing UVB-induced damage, DNA fragmentation, and sun-related aging.
- It also minimizes epidermal thickening caused by chronic sun exposure.
5️⃣ Acne Reduction and Anti-Inflammatory Benefits
- Its anti-inflammatory, antibacterial, and astringent properties help calm acne-prone skin.
- Amla purifies the blood when consumed orally, indirectly benefiting skin clarity and reducing breakouts.
6️⃣ Holistic Skin Wellness from Within
- Ingesting Amla as a supplement, juice, or powder delivers internal support:
- Promotes collagen synthesis
- Improves skin thickness and elasticity
- Reduces fine lines
- Brightens overall complexion
How to Incorporate Amla into Your Skincare Routine
🧴 Topical Application
- Serums & Creams: Choose professionally formulated products where “Emblica officinalis extract” appears high on the ingredient list.
- DIY Masks: Mix Amla powder with ingredients like yogurt, honey, or rose water for a brightening and calming face mask.
- Example Recipe:
- 1 tsp Amla powder
- 2 tsp plain yogurt
- 1 tsp honey
- Apply for 10-15 minutes, rinse with lukewarm water.
- Example Recipe:
- Toners or Mists: Amla-infused water can be used as a hydrating mist.
📝 Tip: Always patch-test any new topical application to check for sensitivity.
🥤 Oral Consumption
- Amla Powder: 1–3 grams daily mixed with warm water or smoothies.
- Amla Juice: 15–30 ml daily on an empty stomach for maximum absorption.
- Capsules/Tablets: Follow recommended dosages on certified supplement brands.
📝 Note: Consistency is key for noticeable skin benefits — results often appear after 8-12 weeks of daily use.
Precautions and Safety
- Generally well-tolerated for most people.
- Those on blood thinners, diabetic medication, or hypotensive drugs should consult a healthcare provider before starting regular Amla consumption.
- Excessive intake may cause mild gastrointestinal discomfort in some individuals.
Real People, Real Results
Many skincare enthusiasts who’ve incorporated Amla into their routine report:
- Brighter, more even-toned complexion
- Reduced appearance of fine lines and pigmentation
- Softer, plumper skin texture
- Fewer acne breakouts and clearer skin
The combination of antioxidant power + anti-inflammatory action + collagen support makes Amla uniquely multi-functional — working both at the surface and deep within the skin layers.
The Final Word
In an era where people are increasingly seeking safe, effective, and natural skincare alternatives, Amla stands out as a gold standard botanical ingredient. Its synergy of ancient wisdom and cutting-edge science offers a holistic path to radiant, youthful skin.
Whether applied topically or consumed orally, Amla delivers a range of benefits unmatched by most single-ingredient solutions. If you’re looking to elevate your skincare game naturally — with real scientific backing — Amla might just be your skin’s best new friend.
🌿 Pro Tip: Combine Amla with…
- Hyaluronic Acid for extra hydration
- Vitamin E to boost antioxidant synergy
- Niacinamide for pigmentation and pore refinement
- Collagen supplements to maximize firming benefits
FAQs
1️⃣ Is Amla safe for all skin types?
Yes, Amla is generally safe for most skin types including sensitive, oily, and dry skin. However, due to its high vitamin C content, some individuals with very sensitive skin may experience mild irritation. Always do a patch test before applying any new Amla-based product to your face.
2️⃣ How long does it take to see visible results on the skin with Amla?
Clinical studies and anecdotal reports suggest noticeable improvements in skin brightness, hydration, and elasticity within 8 to 12 weeks of consistent use, either topically or orally.
3️⃣ Can I use Amla directly on my face?
Yes, you can apply Amla powder mixed with other soothing agents like yogurt, honey, or aloe vera. However, pure Amla juice or undiluted powder may be too strong and acidic for some people, so always dilute it and do a patch test.
4️⃣ Can I take Amla supplements for better skin?
Absolutely. Oral supplementation of Amla — whether as powder, juice, or capsules — provides internal antioxidant support, improves collagen production, hydration, and can reduce pigmentation and acne from within.
5️⃣ Is Amla good for acne-prone skin?
Yes. Thanks to its antibacterial, anti-inflammatory, and astringent properties, Amla can help reduce acne breakouts, calm inflammation, and promote clearer skin when used both topically and orally.
6️⃣ Can Amla help with hyperpigmentation and dark spots?
Yes. Amla inhibits the enzyme tyrosinase, which reduces melanin production. Regular use can help fade hyperpigmentation, dark spots, and even out skin tone.
7️⃣ Does Amla protect against sun damage?
Yes, Amla provides antioxidant protection against UV-induced oxidative stress. While it is not a replacement for sunscreen, using Amla alongside SPF can provide an extra layer of defense against photoaging and sun damage.
8️⃣ Is it safe to use Amla daily?
For most people, daily use is safe both orally and topically when used in appropriate amounts. However, consult a healthcare provider if you have any medical conditions or are on medications (especially for diabetes, blood pressure, or blood thinning).
9️⃣ Can pregnant or breastfeeding women use Amla for skin care?
In small dietary amounts, Amla is typically considered safe, but pregnant or breastfeeding women should consult their healthcare provider before starting any supplements or new skincare products.
🔟 What is the best time to take Amla for skin benefits?
Taking Amla first thing in the morning on an empty stomach maximizes nutrient absorption. For topical use, applying Amla-based products in the morning can enhance antioxidant protection throughout the day.