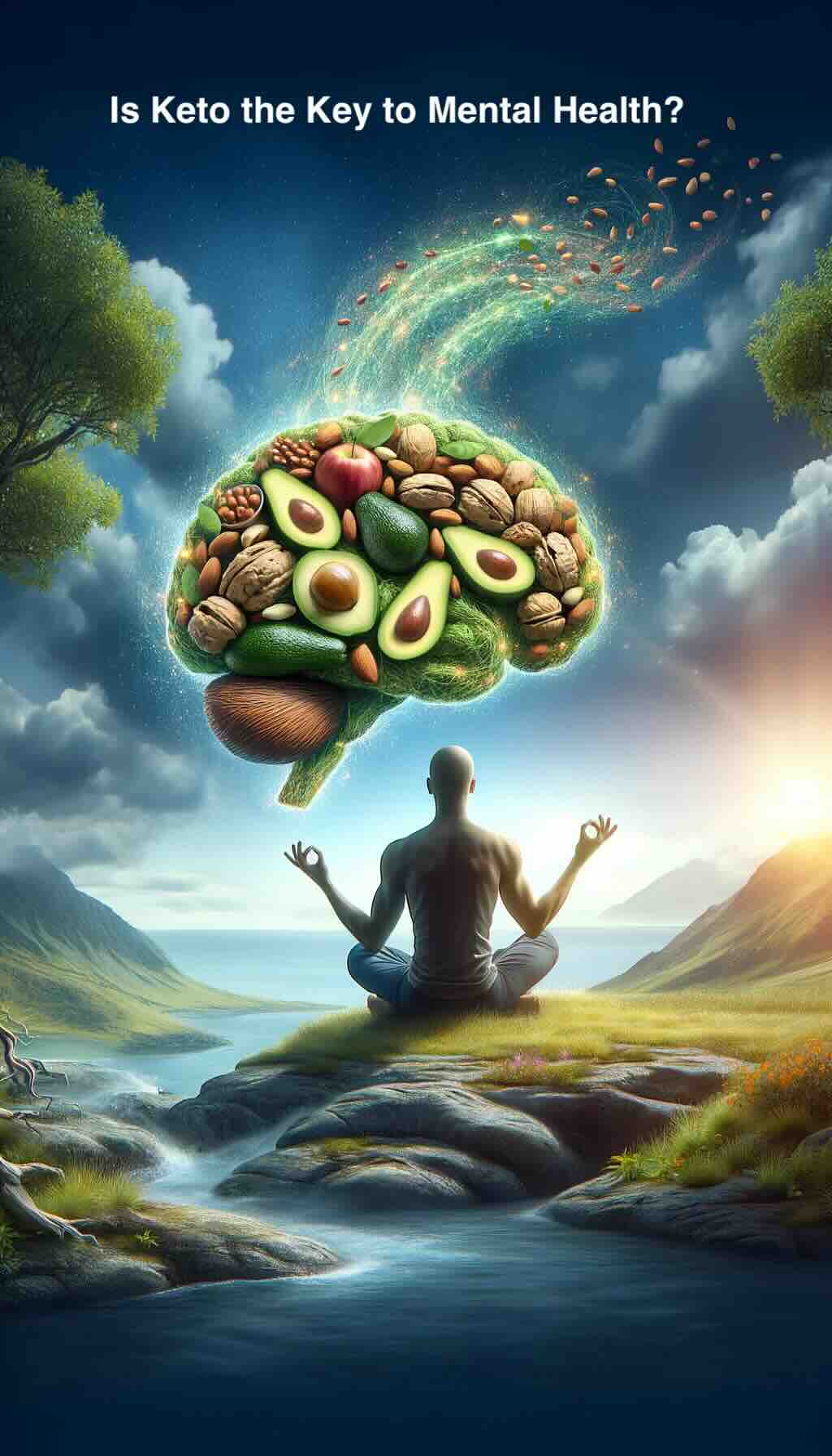
In the realm of mental health, innovative treatments are constantly being explored, and one such promising approach is the ketogenic diet. Traditionally heralded for its success in managing epilepsy, this high-fat, low-carbohydrate diet is now making waves in the field of psychiatry. Let’s dive into the fascinating intersection of nutrition and mental wellness, uncovering how altering our diet can potentially transform mental health care.
Understanding the Ketogenic Diet
At its core, the ketogenic diet involves drastically reducing carbohydrate intake and replacing it with fat, pushing the body into a state of ketosis. In ketosis, the body becomes incredibly efficient at burning fat for energy and produces ketones from fat in the liver, which can supply energy for the brain.
From Epilepsy to Mental Health
The journey of the ketogenic diet from a treatment for epilepsy to a potential solution for mental health issues is a testament to the intricate link between our diet and brain function. Research suggests that the diet’s impact on brain metabolism can have therapeutic effects beyond controlling seizures.
The Science Behind the Diet and Mental Health
- Metabolic Influence on Mental Disorders
Emerging evidence points to metabolic dysfunction as a contributing factor to various mental disorders. The ketogenic diet, by altering the body’s energy metabolism, may offer relief for conditions such as depression, bipolar disorder, and schizophrenia. The diet encourages the body to burn ketones as a primary energy source, which has been linked to improved mood stability and cognitive function.
- Mitochondrial Health and Mental Wellness
Mitochondria, the powerhouses of our cells, play a crucial role in energy production and are vital for brain health. The ketogenic diet has been shown to improve mitochondrial function, potentially addressing the mitochondrial dysfunction observed in many psychiatric disorders. Enhanced mitochondrial activity supports better brain health, offering a novel approach to treating mental illness.
Real-Life Impacts: Case Studies and Clinical Observations
Compelling case studies from healthcare professionals, including Dr. Chris Palmer, illustrate the diet’s profound impact on individuals with severe psychiatric disorders. Patients who had struggled with traditional treatments found significant improvements in symptoms and overall quality of life through dietary changes. These anecdotes underline the diet’s potential as a complementary treatment strategy, encouraging further research and clinical trials.
Practical Tips for Exploring the Ketogenic Diet for Mental Health
- Consult with a Professional: Before making any dietary changes, especially for mental health purposes, consulting with a healthcare provider is crucial.
- Start Slow: Gradually reduce carbohydrate intake while increasing fat intake to ease the transition into ketosis.
- Monitor Your Mental Health: Keep a journal to note any changes in mood, anxiety levels, or cognitive function.
- Nutritional Balance: Ensure the diet is nutritionally balanced, focusing on high-quality fats, moderate proteins, and low carbohydrates.
- Patience is Key: Metabolic changes take time, and the effects on mental health may not be immediate.
The Future of Mental Health Treatment
The exploration of the ketogenic diet in mental health treatment is still in its early stages, but the potential it holds is immense. As we continue to unravel the complex relationship between diet and brain function, the ketogenic diet stands as a beacon of hope for those seeking alternative treatments for mental illness.
This approach to mental health care not only highlights the importance of nutrition in our overall well-being but also encourages a more holistic view of treatment. With ongoing research and clinical studies, we are on the cusp of a paradigm shift in psychiatry, one where our plates might hold the key to our psychological health.
FAQs for “From Seizures to Sanity: Is Keto the Key to Mental Health?”
1. How does the ketogenic diet affect the brain?
The diet induces ketosis, a metabolic state where the body burns fat for energy instead of carbohydrates. This can increase the production of ketones, which provide an alternative energy source for the brain, potentially stabilizing mood and cognitive function.
2. Is the ketogenic diet safe for everyone?
While many people can safely adopt a ketogenic diet, it’s not suitable for everyone. Consulting with a healthcare provider before starting the diet, especially for those with pre-existing health conditions, is crucial.
3. How long does it take to see benefits on mental health from the ketogenic diet?
The time frame can vary significantly between individuals. Some may notice improvements in a few weeks, while others might take several months to experience noticeable changes.
4. Can I use the ketogenic diet to replace my current mental health treatment?
The ketogenic diet should not replace any current treatments or medications for mental health conditions without professional guidance. It can be used as a complementary approach under the supervision of healthcare providers.
5. What are the risks or side effects of the ketogenic diet?
Common side effects include the keto flu, characterized by headache, fatigue, and irritability during the initial adjustment period. Long-term risks may include nutritional deficiencies and other health issues.
6. Are there any specific foods I should eat or avoid on the ketogenic diet?
Yes, the diet emphasizes high-fat foods like avocados, cheese, nuts, and seeds, moderate protein intake, and minimal carbohydrates. Foods to avoid include grains, sugar, and high-carb fruits and vegetables.
7. How can I start the ketogenic diet?
Begin by consulting with a healthcare provider or a dietitian who can provide personalized advice and ensure your diet remains nutritionally balanced while you transition to ketosis.
8. Will I need to stay on the ketogenic diet forever to maintain mental health benefits?
The duration of the diet can vary based on individual goals and responses. Some may find benefits in a shorter term, while others might adopt it as a longer-term lifestyle change.
9. How can I ensure I’m getting enough nutrients on the ketogenic diet?
Consider working with a nutritionist to plan meals that meet all your dietary needs and consider taking supplements for nutrients that are harder to obtain on a ketogenic diet, such as certain vitamins and minerals.
Blog Tags for the Post
ketogenic diet, mental health, nutrition psychiatry, metabolic therapy, bipolar disorder, depression treatment, schizophrenia, brain health, diet and wellness, mental health care