Looking for a natural way to support your weight loss goals? If you’re tired of harsh diet pills and flavorless “health” foods, fennel might be the secret ingredient missing from your journey. Revered for centuries in Mediterranean kitchens and healing traditions, fennel is not only delicious—it’s earning real attention from modern science for its gentle, effective, and multi-faceted support in weight management.
What is Fennel?
Fennel (Foeniculum vulgare) is a highly aromatic herb with a subtle licorice flavor. It’s unique because every part—bulb, stalk, fronds, and seeds—is edible and bursting with nutrients. While you may have encountered fennel seeds in Indian cuisine or the bulb in Italian salads, the entire plant is a powerhouse for both flavor and wellness.
Why Consider Fennel for Weight Loss?
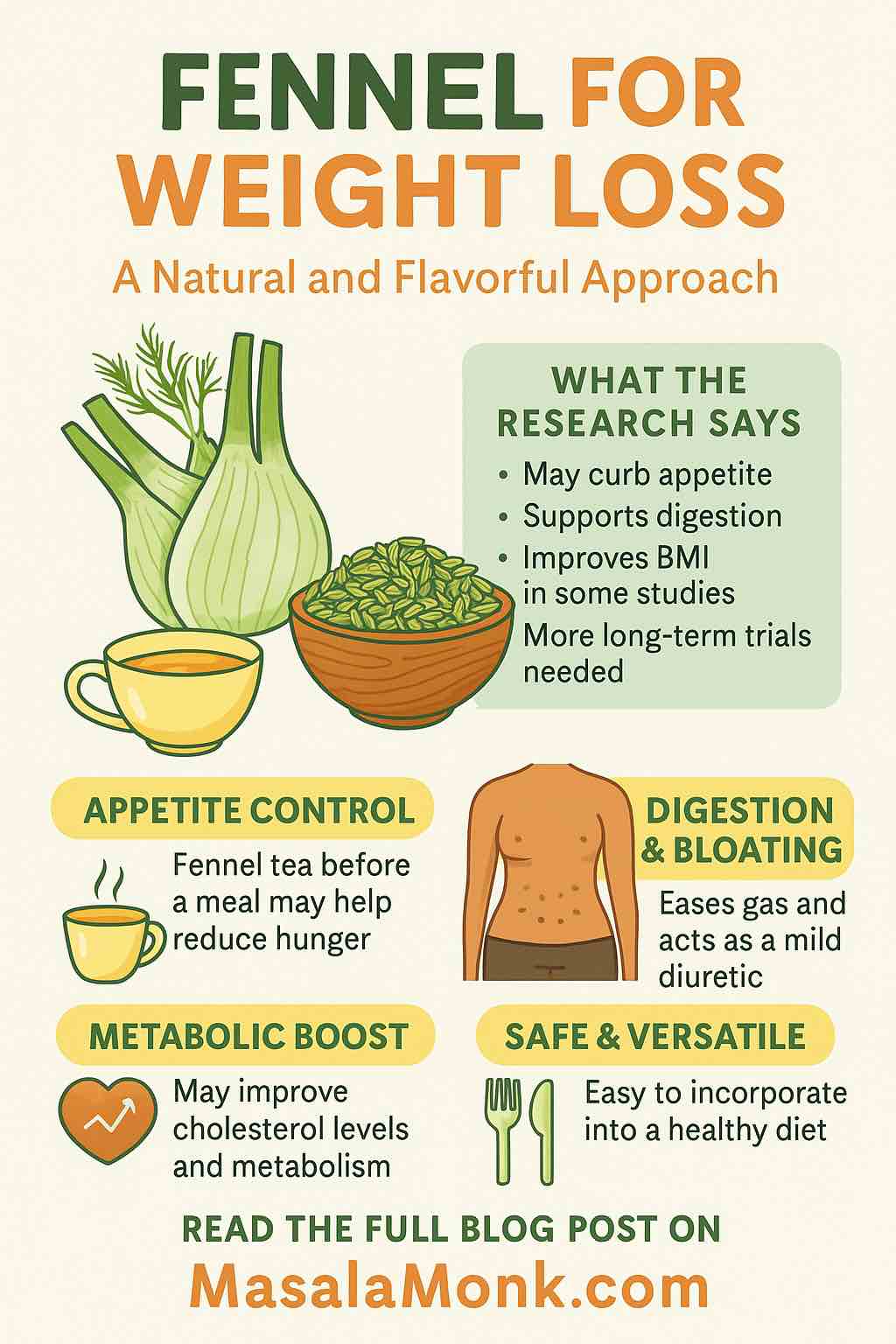
1. Appetite Control: Nature’s Little Secret
Struggling with cravings or overeating? Fennel seeds contain anethole, a compound shown to help regulate appetite hormones. Recent studies suggest that fennel tea, when consumed before meals, can reduce feelings of hunger and lead to lower calorie intake.
Pro tip: Brew fennel tea 15 minutes before lunch or dinner to help curb those extra servings!
2. Digestion & Bloating Relief: Feel Lighter, Not Just Slimmer
Bloating and sluggish digestion can make you feel heavy—even if the scale doesn’t move. Fennel is a traditional digestive, easing gas and discomfort. Modern research supports its use as a carminative (gas-reliever) and mild diuretic, which means less water retention and a flatter stomach.
Quick Fix: Chew a pinch of fennel seeds after your meal, just like they do in India!
3. Metabolic Boost & Lipid Control
Obesity is about more than just calories in versus calories out. It’s linked to inflammation, oxidative stress, and sluggish metabolism. Fennel seeds are rich in antioxidants and fiber, which not only help reduce inflammation but also improve blood lipid profiles.
Recent trials show that adding fennel seed or extract to snacks (think: crackers or yogurt) can improve BMI and cholesterol over just 8 weeks.
4. Safe, Accessible, and Delicious
Unlike many weight-loss “superfoods,” fennel is safe for most people, affordable, and versatile. It fits easily into almost any dietary pattern, from Mediterranean to vegetarian to low-carb.
Science Speaks: What Does the Research Say?
- 2025 Review: A major review in the Pakistan Biomedical Journal noted that fennel’s active ingredients support satiety, fat metabolism, blood sugar, and cholesterol control. While the results are promising, more large clinical trials are needed.
- Human Trials: People consuming snacks fortified with fennel extract saw real improvements in BMI and cholesterol after just two months. Another study found that women drinking fennel tea before meals ate fewer calories and felt fuller, compared to those drinking a placebo.
- Animal Studies: Rats and mice given fennel extract gained less weight and had healthier metabolic markers, thanks to reduced inflammation and oxidative stress.
- Caution: While these findings are encouraging, it’s clear that fennel works best as a supportive aid, not a magic bullet.
✅ Summary of Evidence
| Benefit | Human RCTs | Animal Studies | Mechanism | Level of Evidence |
|---|---|---|---|---|
| Appetite ↓ | Yes (small) | Yes | Anethole effects, ghrelin ↓ | Moderate |
| Body fat/BMI ↓ | Yes | Yes | Improved metabolism, satiety | Moderate |
| Lipid profile improvement | Yes | Yes | Fat metabolism, antioxidant → HDL ↑/LDL ↓ | Moderate |
| Digestive comfort (bloating) | Yes | — | Carminative effect | Strong for digestion |
| Direct body fat loss | Limited | Yes | Preliminary, mostly in animals | Weak in humans |
How to Use Fennel for Weight Loss
1. Fennel Tea
Ingredients:
- 1-2 teaspoons fennel seeds
- 1 cup boiling water
How to Make:
Crush the seeds lightly. Pour boiling water over them, cover, and steep for 10–15 minutes. Strain and sip, ideally before meals.
Why it works:
Studies indicate fennel tea helps control appetite and ease digestion.
2. Fennel Seed Snack Topper
Sprinkle roasted fennel seeds on yogurt, oatmeal, or salads. They add crunch, flavor, and fiber that keeps you fuller longer.
3. Roasted Fennel Bulb
How to Cook:
Slice fresh fennel bulbs. Drizzle with olive oil, salt, and pepper. Roast at 400°F (200°C) until golden and tender. Serve as a side dish or toss with leafy greens.
4. Chew After Meals
Simply chew ½ teaspoon of fennel seeds after eating—an easy, time-tested trick for digestion and fresh breath.
Practical Tips for Maximum Benefit
- Consistency is key: Incorporate fennel daily for best results, but remember, it’s most effective when combined with balanced eating and regular movement.
- Mind your dose: About 5 grams (a teaspoon) of seeds or extract per day is used in many trials.
- Mix with other healthy habits: Use fennel as part of a diet rich in veggies, lean proteins, and whole grains.
- Stay hydrated: Fennel’s mild diuretic effect is best balanced with plenty of water.
Are There Any Risks?
For most, fennel is very safe when used in food amounts. Avoid large supplemental doses if you have a history of hormone-sensitive conditions or are pregnant, due to its mild estrogenic activity. If in doubt, ask your doctor.
The Bottom Line: Can Fennel Help You Lose Weight?
Yes—with a catch. Fennel can curb appetite, reduce bloating, and support a healthier metabolism. But real, sustainable weight loss comes from the combination of smart food choices, physical activity, and habits you can stick with for life.
Fennel isn’t a miracle, but it’s a fantastic flavor-packed tool to help you enjoy the journey.
Want to Get Started?
Try swapping your afternoon snack with fennel tea, or add roasted fennel bulbs to your weekly menu. Small changes add up—and with fennel, they taste great, too.
References & Further Reading
- Therapeutic Effect of Fennel Seeds in the Management of Obesity (2025, PBJ)
- Fennel-Fortified Crackers Improve BMI and Lipid Profile (2023)
- 9 Spices That Can Help You Lose Weight, Verywell Health
- Fennel Benefits and Uses, Health.com
Ready to spice up your routine? Fennel might just be your new weight-loss ally—naturally, flavorfully, and scientifically.
Have you tried fennel for weight loss? Share your experiences or favorite recipes in the comments!
10 Frequently Asked Questions (FAQs) About Fennel for Weight Loss
1. Can fennel really help me lose weight?
Fennel may help with weight loss by reducing appetite, easing bloating, and supporting better digestion. Some small human studies show benefits, especially when combined with a healthy diet and exercise. However, fennel is not a “magic bullet”—it works best as a supportive tool.
2. How should I use fennel for weight loss?
The most common methods are drinking fennel tea before meals, chewing fennel seeds after eating, and adding roasted fennel bulb or seeds to recipes. Aim for about 1–2 teaspoons of seeds (or their equivalent) per day for best effect.
3. What does fennel taste like?
Fennel has a mild, sweet, and slightly licorice-like flavor. The bulb is crisp and refreshing, while the seeds are aromatic and a bit stronger.
4. Is it safe to use fennel every day?
For most people, yes! Fennel is safe when used in culinary amounts. Avoid large medicinal doses if you are pregnant, breastfeeding, or have hormone-sensitive conditions. When in doubt, check with your doctor.
5. Will fennel make me lose belly fat?
Fennel can help reduce bloating, making your stomach appear flatter. While it may support fat loss as part of a healthy lifestyle, no food (including fennel) specifically targets belly fat.
6. Does fennel have any side effects?
Side effects are rare when fennel is consumed as a food or tea. In large doses, it can cause allergic reactions or interact with certain medications. Stick to moderate, food-based amounts.
7. Can I use fennel with other weight loss herbs?
Yes! Fennel combines well with herbs like ginger, cumin, or black cumin (Nigella sativa) for enhanced digestive and metabolic effects. Always introduce new herbs gradually to monitor tolerance.
8. How soon can I expect to see results?
You might notice less bloating and better digestion within days. Weight loss or appetite changes usually take several weeks, and results are most noticeable when paired with other healthy habits.
9. Are fennel supplements as effective as seeds or tea?
Whole seeds and tea are the most researched and traditional forms. Some supplements may be effective, but quality varies—choose reputable brands and stick close to food-based options when possible.
10. Can children or older adults use fennel safely?
Fennel is generally safe for all ages in food amounts. For children, use smaller portions. For older adults, fennel can aid digestion and reduce bloating—just consult a healthcare provider if there are existing health conditions or medications.