Garlic, the pungent bulb revered for centuries in culinary traditions, is also a powerhouse of medicinal and cosmetic properties. Packed with sulfur compounds, antioxidants, and essential nutrients, garlic offers a treasure trove of benefits for both skin and hair. In this post, we’ll explore the latest insights into how this humble ingredient can transform your skincare and haircare routine.
Garlic for Skin: Nature’s Detox Agent
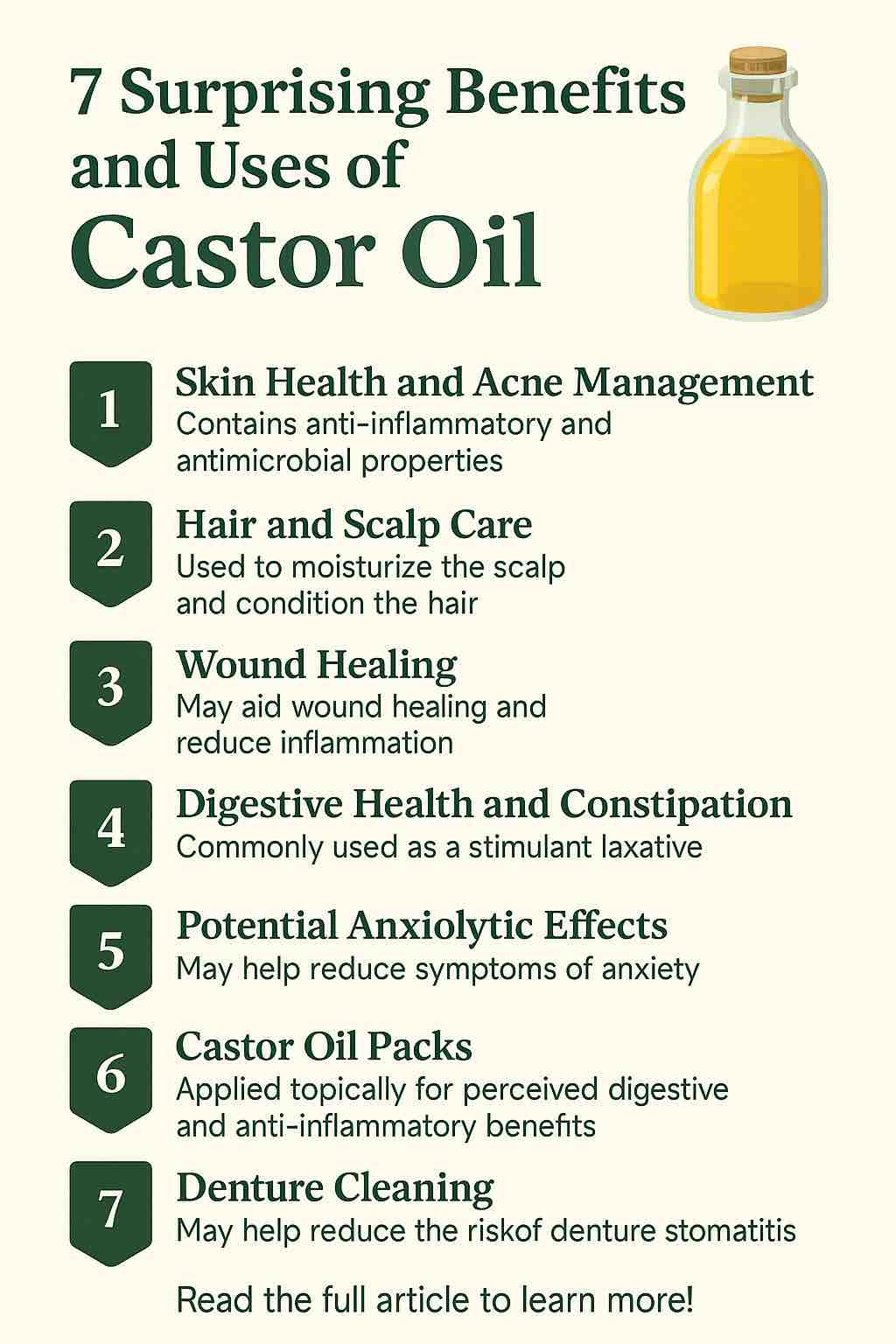
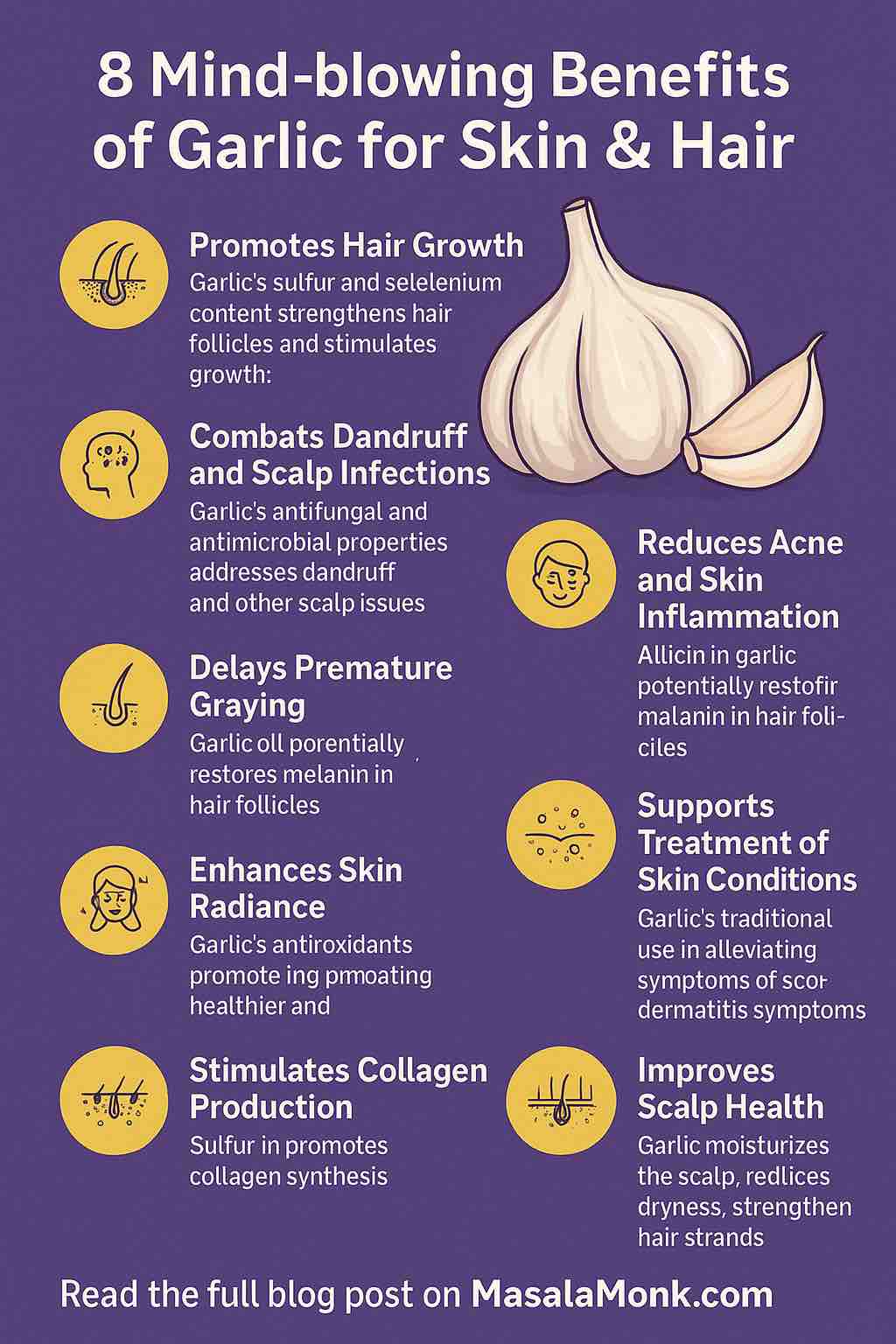
1. Fights Acne and Blemishes
Garlic contains a potent compound called allicin, known for its powerful antibacterial, antifungal, and antiviral properties. These qualities make garlic highly effective against acne-causing bacteria. It also reduces inflammation, helping to calm the redness and swelling associated with pimples. While direct application of raw garlic should be approached with caution due to its intensity, diluted garlic oil or garlic-infused topical products are gaining popularity for their acne-clearing effects.
DIY Tip: Mix crushed garlic with aloe vera gel and apply to affected areas. Leave on for 5–10 minutes and rinse thoroughly.
2. Anti-Aging and Collagen Production
Sulfur, a mineral present in garlic, plays a crucial role in the production of collagen—an essential protein that maintains skin elasticity and firmness. Antioxidants in garlic also combat free radicals, which accelerate the aging process. Regular topical use may help reduce fine lines and give your skin a more youthful glow.
3. Treats Skin Conditions (Psoriasis, Eczema, Dermatitis)
Garlic’s anti-inflammatory and immune-boosting properties make it a natural remedy for chronic skin conditions. It can help reduce flare-ups and soothe itching. While garlic is not a substitute for prescription treatments, incorporating it as a complementary remedy may enhance overall skin health.
Caution: Always do a patch test to avoid allergic reactions.
4. Enhances Skin Radiance
Garlic detoxifies the skin by purifying the blood and enhancing circulation. Improved blood flow delivers more nutrients to the skin, resulting in a healthier, more vibrant complexion. Consuming garlic regularly can amplify these effects from within.
Garlic for Hair: Strength from Root to Tip
5. Stimulates Hair Growth
Garlic boosts hair growth by increasing blood circulation to the scalp. Selenium and sulfur help fortify hair follicles, promoting healthier and faster growth. Some studies also suggest that garlic extract applied to the scalp can help treat alopecia areata (patchy hair loss).
DIY Tip: Blend garlic cloves with carrier oils like coconut or castor oil. Warm slightly and massage into the scalp. Leave for 30 minutes before washing off.
6. Combats Dandruff and Scalp Infections
Thanks to its antifungal properties, garlic is effective in treating dandruff and other scalp infections. It helps maintain a healthy scalp environment, which is essential for sustained hair growth.
7. Prevents Hair Thinning and Breakage
The nutrients in garlic—including Vitamin C, B6, and manganese—help strengthen hair strands, reducing breakage and thinning. This is particularly beneficial for people experiencing hair damage due to environmental stressors or heat styling.
8. Delays Premature Graying
Emerging research indicates that garlic may help delay the appearance of gray hair by increasing catalase levels, an enzyme that breaks down hydrogen peroxide buildup in the hair follicles. This can potentially restore natural pigment when used consistently.
Final Thoughts: A Word of Caution
While garlic offers numerous skin and hair benefits, it’s essential to use it correctly. Raw garlic can be extremely potent and may cause skin irritation or burns when applied directly. Always dilute it with carrier ingredients and conduct a patch test before regular use. If you have sensitive skin or an underlying skin condition, consult a dermatologist before integrating garlic into your beauty routine.
Whether consumed as part of your diet or used topically, garlic proves to be more than just a kitchen staple. With consistent use and proper care, it can be a powerful ally in your journey to healthier skin and stronger hair.
Ready to unlock the power of garlic? Start small, stay consistent, and let nature do the rest.
🔍 10 FAQs About Using Garlic for Skin and Hair
1. Can I apply raw garlic directly to my skin?
Raw garlic is very potent and can cause irritation or chemical burns. Always dilute it with aloe vera gel, honey, or carrier oils before topical use and do a patch test first.
2. How often should I use garlic on my skin or scalp?
For topical applications, 1–2 times per week is generally safe. More frequent use may lead to irritation, especially for sensitive skin or scalp.
3. Is garlic effective for treating acne scars?
While garlic helps reduce acne due to its antibacterial properties, it’s not proven to fade deep acne scars. It may, however, improve skin tone and reduce inflammation, which can help prevent new scars.
4. Can garlic help with hair regrowth in bald spots?
Some studies and anecdotal reports suggest that garlic may aid in treating conditions like alopecia areata. It works best when used consistently and in combination with a healthy scalp care routine.
5. What’s the best way to consume garlic for skin and hair benefits?
Eating 1–2 raw cloves of garlic daily (preferably crushed and left to sit for 10 minutes) may boost skin clarity and hair health. Cooking garlic reduces some of its active compounds.
6. Will garlic oil work the same as raw garlic?
Garlic oil (especially homemade or cold-infused) retains many of garlic’s benefits and is gentler on the skin and scalp. It’s a good alternative for those with sensitivity.
7. Are there any side effects of using garlic topically?
Yes. Common side effects include burning, redness, itching, or allergic reactions. Always test a small area of skin first and never leave it on overnight.
8. How long will it take to see results?
For both skin and hair, it can take 4–6 weeks of consistent use to notice visible changes. Natural remedies typically require patience and regular use.
9. Can garlic prevent or reverse gray hair?
While some early studies suggest garlic may help increase catalase activity (which breaks down hydrogen peroxide buildup in hair follicles), there’s no guarantee. It may slow the process, but reversing gray hair is unlikely.
10. Who should avoid using garlic on skin or hair?
People with very sensitive skin, eczema, or known garlic allergies should avoid topical use. Pregnant or breastfeeding women should consult a doctor before ingesting garlic in medicinal quantities.