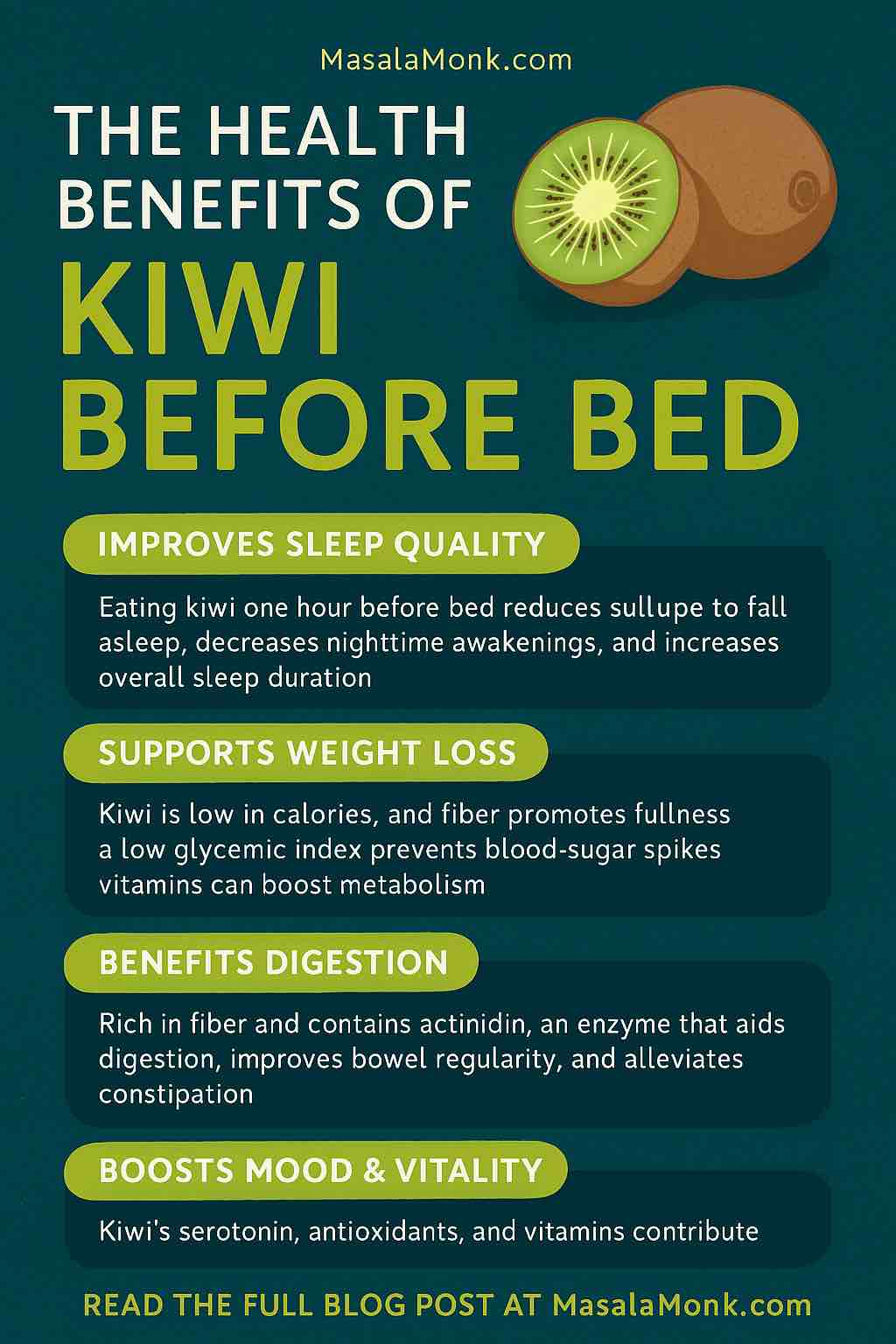
When it comes to improving health naturally, few foods check as many boxes as kiwi—especially when consumed at night. Though it may seem like just another tropical fruit, kiwi holds a special place in the world of nutrition thanks to its unique composition of bioactive compounds, micronutrients, and enzymes. In recent years, researchers have uncovered that eating kiwi before bedtime may not only improve sleep quality but also support weight management, digestion, cardiovascular health, and mood regulation.
In this comprehensive guide, we’ll explore the science, the benefits, the practical application, and the precautions of adding kiwi to your nightly routine.
🥝 What Makes Kiwi Special?
Before we dive into the health benefits, it’s worth understanding why kiwi is so nutritionally unique:
- High in serotonin and melatonin precursors: Rare among fruits.
- Rich in vitamin C (more than an orange): Essential for immunity and antioxidant protection.
- Source of vitamin E, folate, potassium, magnesium: Vital for nervous system and metabolic health.
- Powerful antioxidants (polyphenols, carotenoids, flavonoids): Reduce oxidative stress.
- Contains actinidin: A natural enzyme that aids protein digestion.
- Excellent fiber content (~3 grams per medium kiwi): Supports gut health and satiety.
This powerful nutritional profile is why kiwi has become the subject of increasing clinical interest, particularly for its role in sleep regulation and metabolic health.
💤 Kiwi and Sleep: The Science Behind the Hype
Sleep is a foundation of good health, yet many struggle to get enough restful sleep. Pharmaceutical sleep aids may come with side effects and dependency risks. That’s where kiwi offers a natural alternative.
📊 The Clinical Evidence
Taiwan Sleep Study (2011)
In one of the most cited studies, researchers from Taipei Medical University evaluated 24 adults with self-reported sleep disturbances. Participants consumed two green kiwis one hour before bedtime for 4 weeks. The results were remarkable:
- 35% reduction in time taken to fall asleep (sleep-onset latency)
- 13% increase in total sleep time
- 5% improvement in sleep efficiency
- 29% reduction in night awakenings
Elite Athlete Study (2023)
Athletes, who often experience sleep disruptions due to training stress, saw similar benefits after consuming kiwi nightly for 4 weeks:
- Improved sleep duration, efficiency, and subjective sleep quality.
- Enhanced recovery balance between training loads.
Acute Effect Study (2023)
A recent randomized controlled trial compared fresh and dried kiwi in men. Both forms increased serotonin metabolite levels (5-HIAA), improving morning alertness and mood, especially among poor sleepers.
🔬 Why Does Kiwi Improve Sleep?
Kiwi’s sleep-promoting effects come from multiple synergistic mechanisms:
| Component | Function |
|---|---|
| Serotonin | Regulates mood, sleep onset, converted into melatonin |
| Melatonin precursors | Supports circadian rhythm and sleep-wake cycles |
| Vitamin C and E | Antioxidants reduce oxidative stress, linked to poor sleep |
| Folate & Magnesium | Essential for neurotransmitter synthesis and relaxation |
| Fiber (gut-brain axis) | Supports gut microbiome, which influences sleep |
Unlike single-target supplements, kiwi works on several pathways simultaneously, which may explain its superior, natural results.
⚖️ Kiwi for Weight Management: A Supporting Role
Although kiwi isn’t a magic weight-loss pill, several of its properties make it a valuable tool in weight control, especially when eaten at night:
🏷 Low-Calorie Nutrient Density
- 1 medium kiwi: ~60–90 calories
- Nutrient dense, not calorie dense, allowing you to feel full with minimal caloric load.
🏷 High Fiber Content
- Soluble and insoluble fiber slow gastric emptying.
- Promotes satiety, curbing late-night cravings.
- Helps stabilize blood sugar levels overnight.
🏷 Blood Sugar Regulation
- Kiwi has a low glycemic index (GI ~50), leading to a slower rise in blood sugar.
- Prevents insulin spikes that can lead to fat storage or nighttime hunger.
🏷 Digestive Support via Actinidin
- Improves digestion, reducing bloating and promoting regularity.
- May alleviate mild constipation—a factor often linked to abdominal discomfort and water retention.
🏷 Metabolic and Cardiovascular Health
- Studies show that regular kiwi consumption may:
- Reduce blood pressure.
- Lower LDL cholesterol.
- Improve endothelial function (supporting cardiovascular health).
✅ These cardiovascular and metabolic benefits indirectly support healthier body weight regulation over time.
🧪 Gut-Brain Axis: The Underrated Kiwi Benefit
Emerging research on the gut-brain axis highlights how kiwi may influence both digestion and sleep through its impact on gut microbiota.
- Kiwi’s prebiotic fibers feed beneficial gut bacteria.
- A healthier microbiome can:
- Support balanced neurotransmitter production.
- Reduce systemic inflammation.
- Improve mental clarity and mood.
- Regulate hunger hormones (like ghrelin and leptin).
In essence, kiwi may help rebalance the entire gut-brain system, enhancing both sleep and metabolism simultaneously.
🍽️ How to Use Kiwi Practically at Night
Adding kiwi to your nightly routine is both simple and highly effective when done consistently.
🕰 Ideal Timing
- Consume 1–2 fresh kiwis about 1 hour before bedtime.
- Allows time for nutrient absorption to support melatonin production and relaxation.
🥣 How to Eat It
- Fresh and sliced (best absorption).
- Leave the skin on for maximum fiber (after washing thoroughly).
- Combine with light protein (Greek yogurt, cottage cheese) for additional satiety.
- Avoid heavy meals and high-GI snacks close to bedtime.
📝 Sample Bedtime Routine:
| Time | Activity |
|---|---|
| 8:30 PM | Light, balanced dinner |
| 9:30 PM | Consume 2 kiwis |
| 10:30 PM | Lights off, sleep prep |
🧉 Bonus Nighttime Kiwi Recipes:
1️⃣ Kiwi & Chamomile Smoothie
- 2 kiwis, ½ banana, ½ cup Greek yogurt, cooled chamomile tea, honey drizzle.
2️⃣ Kiwi Chia Pudding
- Blend kiwi puree into chia seed pudding made with almond milk.
3️⃣ Simple Kiwi Yogurt Bowl
- Diced kiwi, probiotic-rich yogurt, sprinkle of flaxseed.
⚠️ Precautions & Considerations
While generally safe for most people, a few precautions apply:
- Allergies: Kiwi is part of the latex-fruit syndrome group; those with latex allergies may react.
- Acidic Fruit: Excessive consumption may cause mild mouth or stomach irritation.
- Medication Interactions: High vitamin K content may affect blood thinners. Consult your doctor if on anticoagulants.
📊 Summary Table
| Benefit | Mechanism |
|---|---|
| Improved Sleep | Serotonin, melatonin precursors, antioxidants |
| Weight Management | Low calorie, high fiber, low GI, digestive enzymes |
| Cardiovascular Health | Blood pressure & cholesterol regulation |
| Digestive Support | Actinidin enzyme, fiber regularity |
| Gut-Brain Health | Prebiotic support of microbiome |
| Mood Elevation | Serotonin and reduced oxidative stress |
🧠 The Bottom Line
The simple habit of eating 1–2 kiwis at night offers an impressive range of health benefits. Backed by growing scientific evidence, kiwi supports better sleep quality, mood, digestion, and metabolic function — all while being delicious, natural, and easy to integrate into your daily life.
Whether you’re struggling with insomnia, aiming for better weight control, or just seeking an overall wellness boost, adding kiwi to your evening ritual may be one of the simplest and most effective changes you can make.
🌿 Sometimes, nature’s best medicine really does come in small, green packages.
📚 Frequently Asked Questions (FAQs)
1️⃣ How many kiwis should I eat at night to see benefits?
The majority of studies recommend consuming 1–2 kiwis about 1 hour before bedtime. This amount appears sufficient to support serotonin production, improve sleep onset, and promote longer sleep duration.
2️⃣ Can eating kiwi really help me lose weight?
Kiwi alone won’t cause weight loss, but it can support weight management. Its high fiber content, low calorie density, low glycemic index, and digestive benefits help reduce cravings, improve satiety, and regulate blood sugar, making it easier to maintain a calorie-controlled diet.
3️⃣ Does kiwi help with digestion too?
Yes. Kiwi contains actinidin, a natural enzyme that helps break down proteins and promotes efficient digestion. Its fiber also supports regular bowel movements and fosters a healthy gut microbiome.
4️⃣ Is it safe to eat kiwi every night?
For most people, yes. Daily consumption of 1–2 kiwis is generally safe and well-tolerated. However, those with kiwi allergies or latex-fruit syndrome should exercise caution and consult a healthcare provider.
5️⃣ What is the best time to eat kiwi for sleep benefits?
For maximum sleep support, eat kiwi about 60 minutes before your intended bedtime. This allows your body time to metabolize its serotonin precursors and antioxidants that aid relaxation.
6️⃣ Can I eat the kiwi skin?
Yes — the skin is edible, nutrient-rich, and packed with extra fiber and antioxidants. Wash it thoroughly before eating to remove any pesticides or surface residues.
7️⃣ Is there a difference between green and golden kiwi for sleep and weight loss?
Both varieties offer similar core benefits, though green kiwi is more extensively studied for sleep. Golden kiwi tends to be slightly sweeter, has less fiber, but still provides antioxidants, vitamin C, and serotonin precursors.
8️⃣ Can children or elderly people eat kiwi at night?
Yes, kiwi is safe for most age groups. Its nutrient profile may particularly help older adults with digestion and sleep. Always introduce it slowly to monitor tolerance, especially in children.
9️⃣ Can I eat dried kiwi instead of fresh?
Studies show that both fresh and dried kiwi can offer benefits, though dried kiwi may contain added sugars and more calories. Choose unsweetened dried kiwi if opting for this version, and control portions carefully.
🔟 Will eating kiwi interfere with my medications?
In most cases, kiwi does not interfere with common medications. However, those taking blood thinners (due to vitamin K content) or with certain gastrointestinal conditions should consult their doctor before adding large amounts of kiwi to their diet.