Pregnancy can feel like a rollercoaster—joy, anticipation, and a fair share of nerves. For millions of women each year, one extra challenge enters the scene: gestational diabetes mellitus (GDM). While the name sounds daunting, understanding GDM—its symptoms, impact, and the science behind it—empowers you to take control.
This guide brings together the latest global research, practical tools, and tables for clarity, with a focus on real-life strategies and what’s new in 2025.
What is Gestational Diabetes?
Gestational diabetes is high blood sugar (glucose) that develops during pregnancy in women who didn’t have diabetes before. It most often emerges between weeks 24 and 28—just when you’re starting to show and baby’s growth is ramping up.
Why does it happen?
Hormonal changes in pregnancy can make your body less sensitive to insulin. If your pancreas can’t compensate, glucose builds up in your bloodstream.
Who’s at risk?
- Over age 25
- Family history of type 2 diabetes
- Overweight or obese before pregnancy
- Previous gestational diabetes or a very large baby
- Certain ethnicities (South Asian, Black, Hispanic, Indigenous)
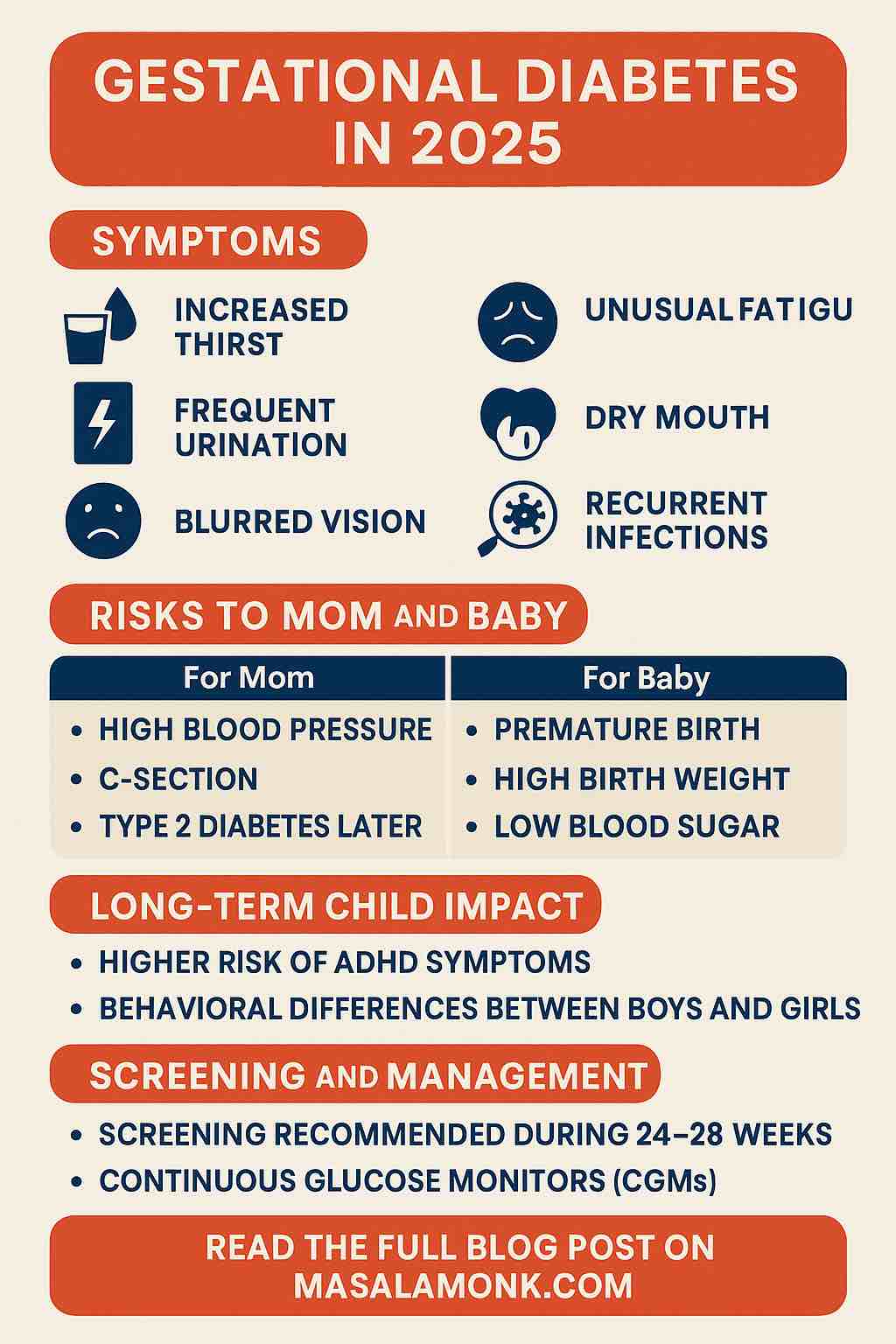
Silent Symptoms: What Should You Watch For?
Most women with gestational diabetes have no symptoms at all. It’s a silent condition, which is why screening is standard for all pregnancies.
But if symptoms do appear, they’re often mild and easy to mistake for normal pregnancy changes:
- Increased thirst
Are you suddenly parched, even after downing water? - Frequent urination
(Though, let’s be honest, every pregnant woman is peeing more.) - Unusual fatigue
Tired beyond the typical “pregnancy tired”? - Dry mouth
- Blurred vision
- Recurring infections
Such as UTIs or yeast infections. - Increased hunger or unexplained weight changes
Why symptoms are unreliable:
Most of these signs can be chalked up to pregnancy itself, making self-diagnosis nearly impossible. That’s why routine screening matters (more on that soon).
Table 1: Symptoms of Gestational Diabetes
| Symptom | Description | How Common in GDM? | Notes |
|---|---|---|---|
| None | No noticeable symptoms | Most common | Why screening is so important |
| Increased thirst | Persistent urge to drink water | Sometimes | Often overlooked |
| Frequent urination | Needing to pee more than normal | Sometimes | Also common in late pregnancy |
| Unusual fatigue | Tiredness beyond typical pregnancy fatigue | Sometimes | Nonspecific |
| Dry mouth | Feeling persistently parched | Occasionally | May occur with high blood sugar |
| Blurred vision | Vision changes (temporary) | Rare | Only with significant high glucose |
| Recurrent infections | UTIs or vaginal yeast infections | Occasionally | High sugar promotes infection |
| Increased hunger | Unusual, persistent hunger | Rare | |
| Unexplained weight change | Gaining or losing weight unexpectedly | Rare |
Important:
Symptoms alone are never enough to diagnose GDM—routine screening is essential!
The Latest Research: 2024–2025
Modern medicine is rapidly advancing our understanding of GDM. Here are the most recent and practical insights:
1. Long-Term Child Development Impact
- ADHD and Behavior:
A 2025 European/Australian study (200,000+ pairs) found that children of mothers with GDM showed higher rates of ADHD and externalizing behaviors at ages 4–10.
Read more - Sex-Specific Effects:
A Finnish cohort (N≈3,800) saw that GDM-exposed girls had more internalizing symptoms at 2 years, while boys showed more conduct issues and hyperactivity at age 5.
Read more
2. Screening Innovations
- AI and 3D Body Scanning:
3D optical body scans analyzed by AI can predict GDM risk during weeks 18–24 with 88% accuracy—outperforming BMI and traditional measures by 22%. This is a glimpse of near-future prenatal care!
Read more
3. Updated Clinical Guidelines (2025)
- ADA’s 2025 Recommendations:
The American Diabetes Association now recommends earlier screening for high-risk women, use of continuous glucose monitors (CGMs), and updated medication protocols for safety.
Read more
Screening: Why, When, and How
Screening usually happens between 24 and 28 weeks of pregnancy (sometimes sooner if you have risk factors like obesity, older maternal age, or a family history of diabetes).
How it works:
- You’ll be asked to drink a sugary drink and have your blood sugar checked (glucose challenge test).
- If that’s abnormal, a longer oral glucose tolerance test (OGTT) confirms the diagnosis.
Why so thorough?
Because undiagnosed GDM can cause complications like:
- Preterm birth
- High birth weight (which can lead to difficult deliveries)
- Low blood sugar in the newborn
- Increased risk of developing type 2 diabetes for both mom and child later in life
Table 2: Gestational Diabetes Screening Timeline
| Time in Pregnancy | What Happens | Why? |
|---|---|---|
| First prenatal visit | Risk assessment, early glucose test (if high risk) | Catch pre-existing diabetes early |
| 24–28 weeks | Glucose challenge test (GCT) | Most accurate time for GDM detection |
| If GCT abnormal | Oral Glucose Tolerance Test (OGTT) | Confirms diagnosis |
| Postpartum (6–12 weeks) | Re-test blood sugar | Screen for persistent diabetes |
The Oral Glucose Tolerance Test (OGTT): What to Expect
- Fasting overnight
- Blood sample taken (fasting glucose)
- Drink a sweet liquid (usually 75g glucose)
- Blood samples at 1 and 2 hours after drink
Table 3: OGTT Diagnostic Cutoffs
| Time Point | Normal Value (mg/dL) | GDM Diagnosis If |
|---|---|---|
| Fasting | < 92 | ≥ 92 |
| 1 hour after glucose | < 180 | ≥ 180 |
| 2 hours after | < 153 | ≥ 153 |
A diagnosis is made if any value meets or exceeds the threshold.
Complications: Why Timely Detection Matters
Table 4: Risks for Mom and Baby
| For Mom | For Baby |
|---|---|
| High blood pressure/preeclampsia | Large birth weight (macrosomia) |
| Higher C-section risk | Low blood sugar after birth |
| Increased risk of type 2 diabetes later | Premature birth |
| Recurrent GDM in future pregnancies | Breathing difficulties |
| Rare: Preterm delivery, stillbirth | Higher risk of obesity/type 2 diabetes later |
Early treatment and blood sugar control dramatically reduce these risks.
I Have GDM: Practical Management Steps
Gestational diabetes is manageable. Here’s how to take control and keep both you and baby healthy.
First—breathe. With the right care, most women with GDM go on to have healthy pregnancies and healthy babies.
Here’s what you can do:
- Monitor your blood sugar
- Your provider will teach you how to check at home (or, in some cases, you’ll use a continuous glucose monitor).
- Eat a balanced diet
- Focus on whole grains, lean protein, plenty of veggies, and limit simple sugars. Consider meeting with a registered dietitian for a personalized meal plan.
- Stay active
- Safe exercise like walking, swimming, or prenatal yoga can help manage blood sugar (check with your doctor first).
- Take medication if needed
- Some women need insulin or oral medications if lifestyle changes aren’t enough.
- Keep up with prenatal visits
- You’ll likely have more frequent monitoring to ensure both you and your baby stay healthy.
Table 5: Day-to-Day Management of GDM
| Action | Why It Matters | Practical Tips |
|---|---|---|
| Monitor blood sugar | Detect high/low readings | Use home monitor or CGM; keep a log |
| Eat a balanced diet | Prevent spikes in glucose | Focus on fiber, lean proteins, whole grains; limit processed sugar |
| Stay active | Improves insulin sensitivity | Walking, prenatal yoga, swimming |
| Medication if needed | Keeps blood sugar in target range | Insulin or metformin, as prescribed |
| Attend prenatal checks | Track growth, adjust care plan | More frequent visits if needed |
| Postpartum follow-up | Rule out persistent diabetes | Get retested 6–12 weeks after birth |
Sample Day: Gestational Diabetes Meal Plan
| Meal | Example | Reason |
|---|---|---|
| Breakfast | Whole grain toast, scrambled eggs, spinach | Balanced carbs/protein/fiber |
| Snack | Apple slices + peanut butter | Maintains steady energy |
| Lunch | Grilled chicken, quinoa, roasted veggies | Keeps glucose stable |
| Snack | Greek yogurt with berries | Probiotics, controlled carbs |
| Dinner | Baked salmon, sweet potato, green beans | Lean protein, low GI carbs |
| Snack | Handful of almonds or cottage cheese | Satisfying, stabilizes sugar |
The Science of Prevention: Can You Reduce Your Risk?
Table 6: Evidence-Based Prevention Tips
| Pre-Pregnancy/Between Pregnancies | During Pregnancy |
|---|---|
| Maintain healthy weight | Eat balanced meals |
| Regular exercise | Stay active (doctor approved) |
| Control portion sizes | Avoid sugary drinks |
| Manage blood pressure | Track blood sugar if high risk |
Note: Not all GDM is preventable, but lifestyle changes lower risk and improve outcomes.
Living With GDM: The Emotional Side
Gestational diabetes can bring worry—but remember, you’re not alone. Support groups, online communities, and honest conversations with your provider make a difference. Many women find the experience inspires them to keep healthier habits for years to come.
Key Takeaways
- Gestational diabetes is usually symptomless—don’t rely on “feeling fine.”
- Routine screening between 24–28 weeks is essential for all pregnancies.
- Most women with GDM have healthy pregnancies with proper management.
- Recent science is uncovering subtle, long-term child impacts—early care matters!
- The future includes AI, body scanning, and continuous glucose monitoring for even better outcomes.
Further Reading & Resources
- American Diabetes Association: Standards of Care 2025
- Mayo Clinic: Gestational Diabetes
- ScienceDaily: GDM & Child ADHD
- Nature: GDM and Child Behavior
- arXiv: AI/3D Body Scanning for GDM
FAQs: Gestational Diabetes
1. What exactly is gestational diabetes?
Gestational diabetes is a type of diabetes that develops during pregnancy. It means your blood sugar levels are higher than normal, but it usually goes away after you give birth. It’s different from having diabetes before pregnancy.
2. Why don’t I have any symptoms of gestational diabetes?
Most women with gestational diabetes experience no noticeable symptoms. That’s why screening is routine for all pregnancies, usually between 24–28 weeks.
3. How is gestational diabetes diagnosed?
It’s diagnosed using a two-step process: an initial glucose challenge test (GCT), followed by an oral glucose tolerance test (OGTT) if needed. Blood samples are measured after fasting and after drinking a glucose solution.
4. Will gestational diabetes harm my baby?
With early diagnosis and proper management, most women with gestational diabetes have healthy babies. Unmanaged GDM can increase risks of complications like large birth weight, premature birth, or low blood sugar in the newborn.
5. What foods should I avoid if I have gestational diabetes?
Limit simple sugars and refined carbs (like white bread, sweets, sugary drinks). Focus on whole grains, lean proteins, vegetables, and healthy fats for stable blood sugar.
6. Will I need insulin or medicine for gestational diabetes?
Many women can control GDM with diet and exercise. If those aren’t enough, your doctor may prescribe insulin or oral medications to keep your blood sugar in a healthy range.
7. How often should I check my blood sugar during pregnancy?
Your healthcare team will guide you, but most women check several times a day—before meals and sometimes after meals—using a home glucose monitor or a continuous glucose monitor (CGM).
8. Does gestational diabetes go away after delivery?
For most women, yes—it resolves after birth. However, you’ll need a follow-up test 6–12 weeks postpartum to confirm your blood sugar is back to normal.
9. Am I at higher risk for type 2 diabetes later if I had gestational diabetes?
Yes, about half of women who have GDM will develop type 2 diabetes in the future. Healthy habits and regular checkups can help reduce your long-term risk.
10. Can gestational diabetes be prevented?
Not always, but maintaining a healthy weight, staying active, and eating a balanced diet before and during pregnancy can lower your risk.