Are you a woman struggling with energy, mood, weight, or that persistent feeling something’s off—even when your bloodwork is “normal”? You’re not alone.
Thyroid issues affect millions of women worldwide. They often show up as vague, frustrating symptoms: fatigue, brain fog, unexplained weight gain, dry skin, hair loss, anxiety, or menstrual changes. It’s not just in your head, and it’s not just about your numbers—your thyroid is the master regulator of metabolism, hormones, and overall well-being.
But here’s what your doctor may not tell you: what you eat and how you live can dramatically influence how you feel, how well your medication works, and even your risk of future thyroid problems. This isn’t about magical “thyroid diets” or silver-bullet supplements. This is about understanding your body’s unique needs as a woman—and building the daily habits that help you thrive.
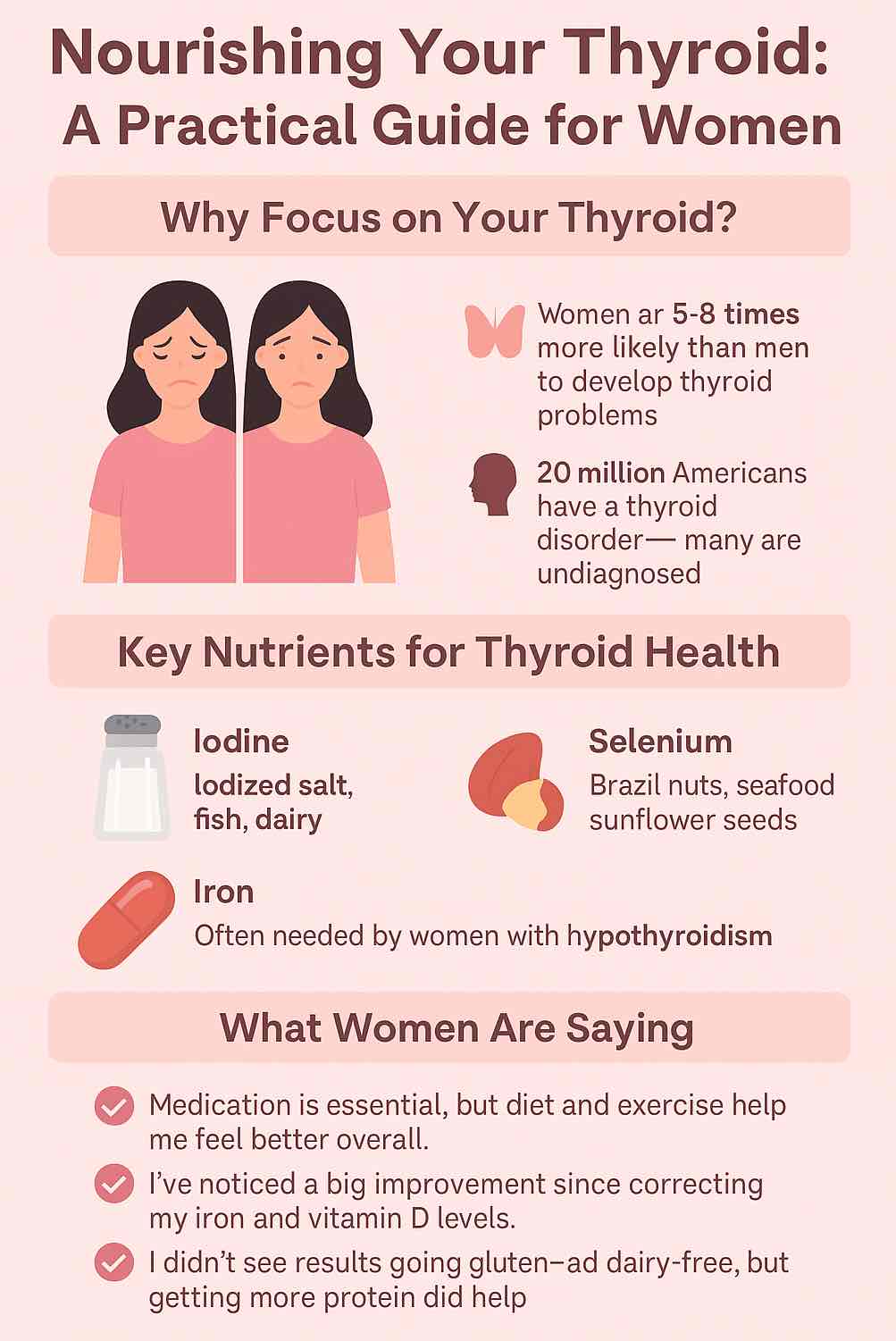
Understanding Your Thyroid: Why Women Need to Pay Special Attention
Your thyroid gland sits quietly at the base of your neck, but its impact is anything but quiet. It releases hormones (T4 and T3) that set the pace for every cell—regulating metabolism, temperature, brain function, heart health, and even how you process other hormones (like estrogen and progesterone).
Women are more vulnerable than men to thyroid disorders due to hormonal shifts (puberty, pregnancy, postpartum, perimenopause/menopause), higher rates of autoimmunity, and sometimes increased risk of nutrient deficiencies.
The two most common thyroid issues are:
- Hypothyroidism (underactive thyroid): Fatigue, weight gain, cold intolerance, constipation, hair loss, low mood.
- Hashimoto’s thyroiditis: An autoimmune disease causing hypothyroidism (the immune system attacks the thyroid).
Why Food and Lifestyle Matter More Than You Think
Here’s the truth:
- Medication is essential if your body isn’t producing enough thyroid hormone.
- Nutrition and lifestyle are powerful levers to optimize your health, help your medication work better, support your immune system, and restore your energy, metabolism, and mood.
The Research Is Clear:
- Diets rich in anti-inflammatory foods (think: lots of vegetables, fish, olive oil, nuts) can lower thyroid antibodies and support hormone balance.
- Gut health is intimately linked with thyroid health—your microbiome helps absorb nutrients and may even “talk” to your immune system to prevent or calm autoimmunity.
- Micronutrient sufficiency—getting enough iodine, selenium, iron, zinc, vitamin D, and more—makes a real difference in how you feel and how well your thyroid functions.
The Nutrients Your Thyroid Can’t Live Without (and How to Get Them)
1. Iodine
- Why it matters: You literally can’t make thyroid hormone without it.
- Best sources: Iodized salt (not sea salt or fancy salts), seaweed (in moderation), fish, eggs, dairy.
- Pro tip: Too much is as bad as too little, especially for women with Hashimoto’s. Stick to natural sources unless your doctor prescribes more.
2. Selenium
- Why it matters: Converts T4 (inactive) to T3 (active), shields the thyroid from inflammation.
- Best sources: Brazil nuts (just 1-2 daily is enough), sunflower seeds, seafood, eggs, turkey.
- Science hack: A 2025 meta-analysis found selenium supplementation (100–200 mcg/day) can lower antibodies in Hashimoto’s, but food is safest unless your doctor suggests otherwise.
3. Iron
- Why it matters: You need iron to make thyroid hormone and for oxygen delivery.
- Best sources: Red meat, poultry, beans, lentils, pumpkin seeds, leafy greens.
- What women say: “Fixing my iron deficiency changed everything. More energy, less hair loss, and finally losing weight!”
4. Zinc
- Why it matters: Key for making and activating thyroid hormone; supports immune health.
- Best sources: Oysters, beef, chicken, nuts, whole grains, chickpeas.
5. Vitamin D
- Why it matters: Low levels are linked to more autoimmunity and worse thyroid symptoms.
- Best sources: Sunlight (15–30 min on arms/legs daily), salmon, sardines, egg yolks, fortified foods.
- Tip: Nearly everyone with Hashimoto’s is low in D—ask for a blood test!
6. B12 and Folate
- Why they matter: Low B12 is common with hypothyroidism (especially if you’re vegetarian or have gut issues).
- Sources: Fish, dairy, eggs, meat, fortified cereals (for B12); greens, beans, citrus (for folate).
7. Tyrosine
- Why it matters: This amino acid is the backbone of your thyroid hormones.
- Sources: Chicken, turkey, dairy, avocados, almonds, pumpkin seeds.
8. Gut-Supporting Fiber and Probiotics
- Emerging research: A healthy microbiome helps absorb thyroid-critical nutrients, keeps inflammation down, and can even modestly improve thyroid hormone levels.
- Best sources: Yogurt, kefir, sauerkraut, kimchi, high-fiber veggies, beans, oats.
Real Women, Real Stories: What’s Actually Working?
Let’s get real—most women with thyroid conditions feel overwhelmed by conflicting advice. Here’s what women are sharing, in their own words:
- On medication & lifestyle:
“Levothyroxine alone got my labs in range, but I still felt tired and foggy. Focusing on protein and cutting processed foods gave me the energy I’d been missing for years.” - On weight loss:
“Losing weight with hypothyroidism is slower, but it’s possible. I stopped focusing on perfection, tracked my food, added walks, and the pounds finally started moving.” - On diet experiments:
“I tried going gluten- and dairy-free. It didn’t change my labs, but my digestion improved, so I stuck with it. My friend, with the same diagnosis, didn’t notice any difference. You have to experiment.” - On deficiencies:
“I was eating healthy but still felt awful. Blood tests showed low iron and vitamin D. Once I fixed those, it was like a light switch for my mood and energy.” - On small wins:
“Just prepping lunch ahead—hard-boiled eggs, veggies, and nuts—keeps me from grabbing junk. Small habits really add up.”
Building Your Thyroid-Friendly Plate: Practical, Day-to-Day Strategies
1. Prioritize Protein at Every Meal
- Why: Helps stabilize energy, curbs cravings, preserves lean muscle (which keeps metabolism higher).
- How: Eggs for breakfast, Greek yogurt or cottage cheese as snacks, chicken/fish at lunch, beans or tofu at dinner.
2. Double Down on Veggies
- Why: Rich in fiber, vitamins, antioxidants, and support gut health.
- How: Aim for at least two cups of non-starchy veggies at lunch and dinner. Mix cooked and raw (but if you have iodine issues, lightly cook cruciferous veggies).
3. Don’t Fear (Healthy) Fats
- Why: Fats like olive oil, avocado, and nuts are anti-inflammatory and keep you full.
- How: Drizzle olive oil on salads, add avocado to toast or smoothies, snack on nuts or seeds.
4. Go for Slow Carbs, Not No Carbs
- Why: Slow-digesting carbs (oats, brown rice, sweet potatoes, quinoa) support steady energy and prevent blood sugar crashes.
- How: Choose one slow carb per meal, limit white bread, pastries, and sugary cereals.
5. Optimize Your Micronutrients
- Why: Deficiencies can stall progress, worsen symptoms, or prevent you from feeling your best.
- How:
- Iodine: Use iodized salt, not sea salt.
- Selenium: Eat a Brazil nut most days.
- Vitamin D: Get outside; ask your doctor about a supplement if you’re low.
- Iron/B12: Include animal protein or fortified foods, especially if you’re vegetarian.
6. Hydrate Wisely
- Why: Even mild dehydration affects energy and metabolism.
- How: Keep a water bottle handy. Try herbal teas, or flavor water with citrus/mint.
7. Space Out Your Thyroid Medication
- Pro tip: Take thyroid meds first thing in the morning with water, wait at least 30–60 minutes before coffee or breakfast to ensure proper absorption. Avoid calcium, iron, or magnesium supplements close to medication time.
Weekly Meal Plan Sample: Food for Real Life
Here’s a sample plan you can tweak to your tastes, budget, and schedule:
Monday
- Breakfast: Omelet with spinach, mushrooms, and feta
- Snack: Greek yogurt + sliced almonds
- Lunch: Grilled salmon over leafy greens with olive oil dressing, roasted sweet potatoes
- Snack: Brazil nut + apple slices
- Dinner: Chicken stir-fry with broccoli (cooked), peppers, carrots, served over brown rice
Tuesday
- Breakfast: Overnight oats with chia seeds, berries, and pumpkin seeds
- Snack: Cottage cheese + sliced cucumber
- Lunch: Lentil and vegetable soup, side of quinoa salad
- Snack: Hard-boiled egg + cherry tomatoes
- Dinner: Turkey chili with black beans, corn, and avocado
Wednesday
- Breakfast: Smoothie (protein powder, banana, spinach, nut butter, almond milk)
- Snack: Kefir or unsweetened yogurt + walnuts
- Lunch: Tuna salad (with beans, celery, olive oil) on mixed greens
- Snack: Carrot sticks + hummus
- Dinner: Baked cod, roasted Brussels sprouts (cooked), brown rice
(Repeat, mix, and match for the rest of the week!)
The Emotional Side: Mindset, Motivation, and What to Do When You Hit a Wall
Thyroid health isn’t just about biology. It’s about mindset and self-compassion. Many women describe years of feeling dismissed, frustrated, or misunderstood.
Practical Mindset Shifts:
- Focus on progress, not perfection: Small, consistent changes beat all-or-nothing thinking every time.
- Track how you feel, not just your weight: Celebrate better energy, mood, and less brain fog as big wins.
- Advocate for yourself: Push for complete lab work, including ferritin, B12, vitamin D, and thyroid antibodies.
- Experiment, don’t obsess: Try different eating patterns (Mediterranean, plant-forward, gluten-free) and see what actually helps you.
- Lean on community: Find others online (r/Hypothyroidism, support groups) or locally to swap stories and motivation.
What to Do When Progress Slows:
- Revisit your nutrition—are you getting enough protein, iron, selenium, and vitamin D?
- Are you sleeping enough and managing stress?
- Are your medications optimized? Has your dose changed since weight loss or a new life stage?
- If you’re stuck, bring data (food/mood/symptom logs) to your doctor or a registered dietitian.
Advanced Tips: Going Beyond the Basics
1. Gut Health: Your Hidden Ally
- Recent studies show that probiotic and synbiotic supplements (for 4–8 weeks) can reduce TSH and boost active T3/T4—especially helpful if you’ve had digestive issues, antibiotics, or lots of processed food.
- Try to eat something fermented daily (yogurt, kefir, sauerkraut, kimchi, miso).
2. Inflammation Busters
- Colorful berries, leafy greens, turmeric, ginger, nuts, seeds, and fatty fish (salmon, sardines, mackerel) are all proven anti-inflammatory foods.
- Swap out vegetable oils and processed snacks for olive oil, avocado, and whole nuts.
3. Body Composition Matters
- New research shows where you carry weight (waist/hips) affects how your thyroid hormones behave.
- Resistance training helps retain muscle, improves metabolism, and balances blood sugar.
4. Hormone Fluctuations
- Pregnancy, perimenopause, and menopause all impact thyroid needs.
- Ask your doctor for thyroid labs during life transitions—doses often need tweaking.
Your Next Steps: Building Your Personal Thyroid Blueprint
- Get a thorough checkup: Insist on full thyroid panel (TSH, Free T4, Free T3, antibodies), ferritin, B12, vitamin D, and iron.
- Start a food/mood/energy journal: You’ll quickly spot what foods, habits, and routines make you feel best.
- Experiment with one small change at a time: Whether it’s adding a Brazil nut, 10 minutes of morning sunlight, or a daily walk.
- Find your tribe: Support is out there—don’t go it alone.
- Celebrate your wins: Whether it’s better sleep, less hair loss, or finishing the week with more energy—you deserve it.
The Bottom Line
Thyroid health is a marathon, not a sprint. Medication is often necessary, but food and lifestyle create the foundation for energy, resilience, and joy. There’s no one-size-fits-all formula—so get curious, stay compassionate with yourself, and take it step by step.
You are not broken, you are not alone, and you are more powerful than you realize. Nourish your body, honor your journey, and trust that small changes truly do add up.
Ready to feel better? Start today with one simple, nourishing meal. Your thyroid—and your whole body—will thank you.
10 FAQs for Women Supporting Thyroid Health
1. Can I manage hypothyroidism with diet alone, or do I need medication?
No, diet cannot replace thyroid hormone if your thyroid is underactive. Medication (like levothyroxine) is essential for most with hypothyroidism. However, a healthy diet supports your energy, immune function, and may improve how you feel and how well your medication works.
2. What foods are best for supporting thyroid function?
Focus on iodine-rich foods (iodized salt, fish, dairy, eggs), selenium sources (Brazil nuts, seafood, sunflower seeds), iron (lean meats, legumes, spinach), zinc (beef, pumpkin seeds), and plenty of colorful vegetables, whole grains, nuts, and seeds. Include probiotic-rich foods for gut health.
3. Should I avoid gluten or dairy if I have Hashimoto’s or hypothyroidism?
There’s no universal need to avoid gluten or dairy unless you have celiac disease, diagnosed intolerance, or personal symptom improvement when eliminating these foods. Many women do not see thyroid benefits from removing them, but some with autoimmune thyroiditis may feel better without gluten.
4. How do I take my thyroid medication for best results?
Take your medication first thing in the morning with water, on an empty stomach. Wait 30–60 minutes before eating, drinking coffee, or taking supplements (especially calcium, iron, magnesium) to ensure proper absorption.
5. Why am I still tired and gaining weight even though my labs are “normal”?
You may have other factors affecting your energy, such as low iron, vitamin D, or B12; poor sleep; unmanaged stress; or your medication dose may need adjustment. Talk to your healthcare provider and ask for a full nutrient panel.
6. Are raw cruciferous vegetables (like broccoli or kale) bad for my thyroid?
In normal portions and if you get enough iodine, cooked or raw cruciferous veggies are generally safe. If you have severe iodine deficiency, it’s better to cook these vegetables and enjoy them in moderation.
7. Can I lose weight with hypothyroidism?
Yes, but it may be slower. Prioritize lean proteins, non-starchy veggies, and whole foods. Monitor your calorie intake, stay active, and correct any nutrient deficiencies. Consistency is more important than rapid progress.
8. Is it safe to take thyroid support supplements from the store?
Be cautious. Many “thyroid support” supplements contain unregulated doses of iodine, selenium, or even unlisted thyroid hormones. Always consult your doctor before starting any new supplement.
9. How does gut health relate to thyroid function?
A healthy gut helps absorb key nutrients (like selenium and zinc) and can influence immune balance. Recent research shows that probiotics and fiber-rich diets may modestly improve thyroid hormone levels and reduce inflammation.
10. What blood tests should I ask for if I have thyroid symptoms?
Request a full thyroid panel (TSH, Free T4, Free T3, thyroid antibodies), plus iron studies (ferritin), vitamin D, vitamin B12, and sometimes folate and zinc, especially if symptoms persist despite treatment.