Is intermittent fasting (IF) a smart daily discipline—or can it tip into harmful territory? If you’ve ever scrolled through fitness forums or Reddit threads, you’ll know opinions (and experiences) run the gamut. This post breaks down the science, real-world stories, and practical wisdom so you can make IF work for you, not against you.
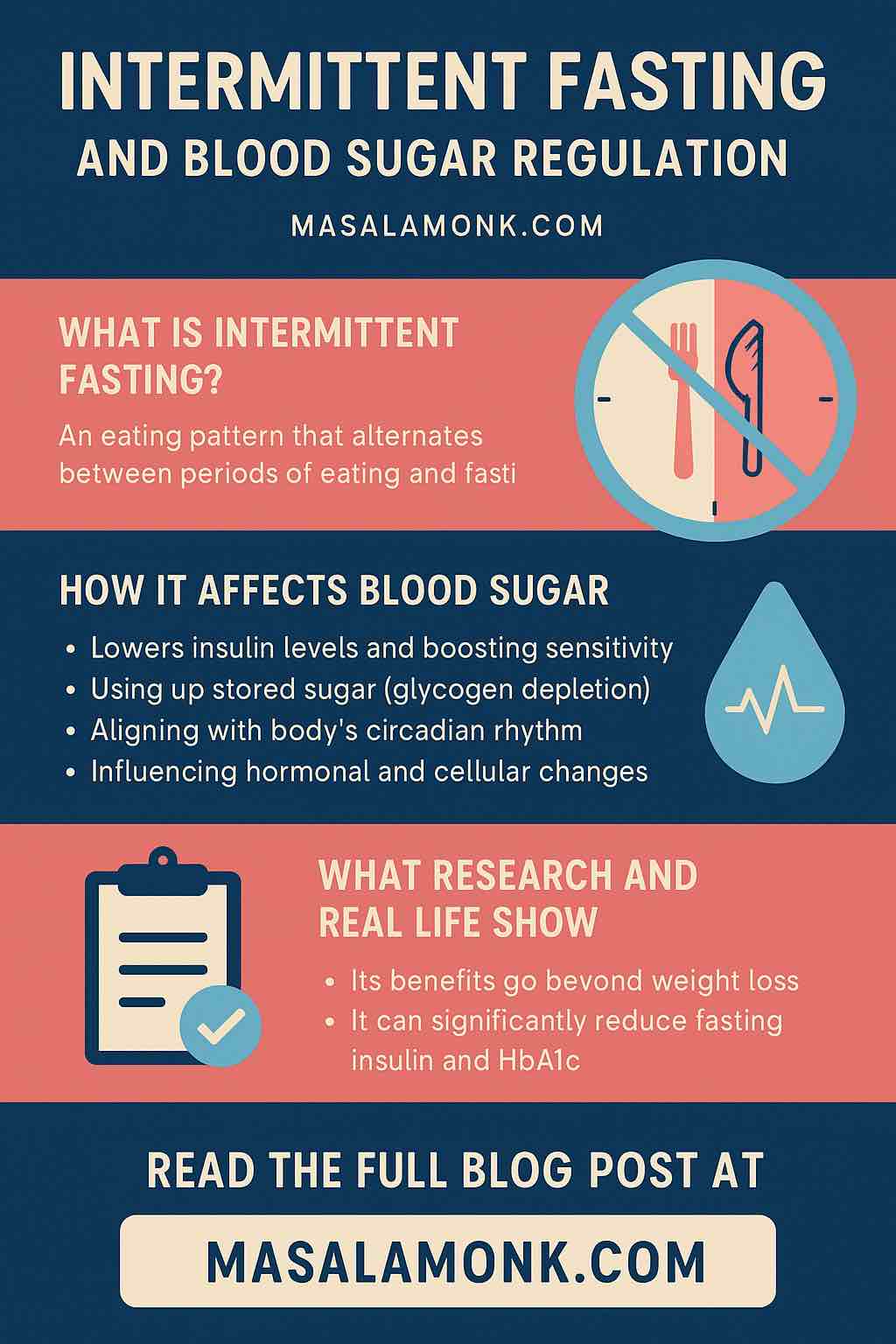
What Is Intermittent Fasting—Really?
At its core, intermittent fasting is not a diet. It’s a pattern for when you eat (and don’t eat). The most popular routines:
- 16:8: Fast for 16 hours, eat within an 8-hour window (ex: noon–8pm).
- 18:6, 20:4, or OMAD (One Meal a Day): Increasingly narrow windows.
- 5:2: Eat normally 5 days, restrict calories 2 days each week.
- Alternate-Day Fasting: Fast every other day.
People love IF for its simplicity—you don’t count calories, you just watch the clock.
The Benefits: More Than Hype?
Science and stories both suggest real advantages.
A massive 2024 analysis in the BMJ found that IF leads to weight loss and improved markers like blood pressure, cholesterol, and blood sugar—often as much as traditional calorie counting. Some protocols (like alternate-day fasting) may even provide a slight edge in waist-trimming and lowering inflammation.
Real Users, Real Results
“I lost about 15 lbs in 3 months … As long as you’re keeping a complete and balanced diet it’s totally healthy.”
—Reddit user, r/intermittentfasting
“I did it for almost 2 years … Lost about 60 lbs and leaned out like crazy. Now, I can maintain my weight with much less effort.”
—Reddit user, r/nutrition
Beyond the scale, many share improvements in focus, appetite control (“hunger has controlled me for years … now I rarely even think about food”), and an easier time resisting mindless snacking.
When Discipline Becomes Overdoing It
But IF isn’t a magic bullet—and it’s definitely possible to overdo it.
Signs You’re Taking It Too Far
- Constant fatigue or brain fog
- Obsession with meal timing or food
- Digestive discomfort on long fasts
- Mood swings, irritability, or poor sleep
- Women: changes in menstrual cycles or hair loss
“Intermittent fasting was what pushed me over the edge from just dieting to straight-up horrible disordered eating. I felt out of control, then obsessed with food, then guilty if I ate outside my ‘window.’”
—Reddit user, cautioning against extremes
People who try OMAD or multiple 24–72 hour fasts sometimes report rapid early weight loss, but just as often hit a wall—binge eating, anxiety, or even regaining more weight when they stop.
Why the Experience Varies So Much
Your body, background, and mindset matter.
- Athletes or those with high energy needs might struggle with performance dips or insufficient recovery.
- Women’s hormones are particularly sensitive to fasting stress—many female users have reported cycle changes with long fasts.
- History of disordered eating? IF can be triggering, even if the intent is health, not restriction.
How to Use IF as a Healthy Discipline (Not a Trap)
1. Start Slow—No Heroics Needed
Begin with a gentle 12–14 hour overnight fast (ex: 8pm–10am), and see how you feel. Most people naturally “skip” breakfast anyway.
2. Choose a Window That Suits Your Life
If 16:8 feels good, great. If not, 14:10 or even a consistent overnight fast can still yield benefits.
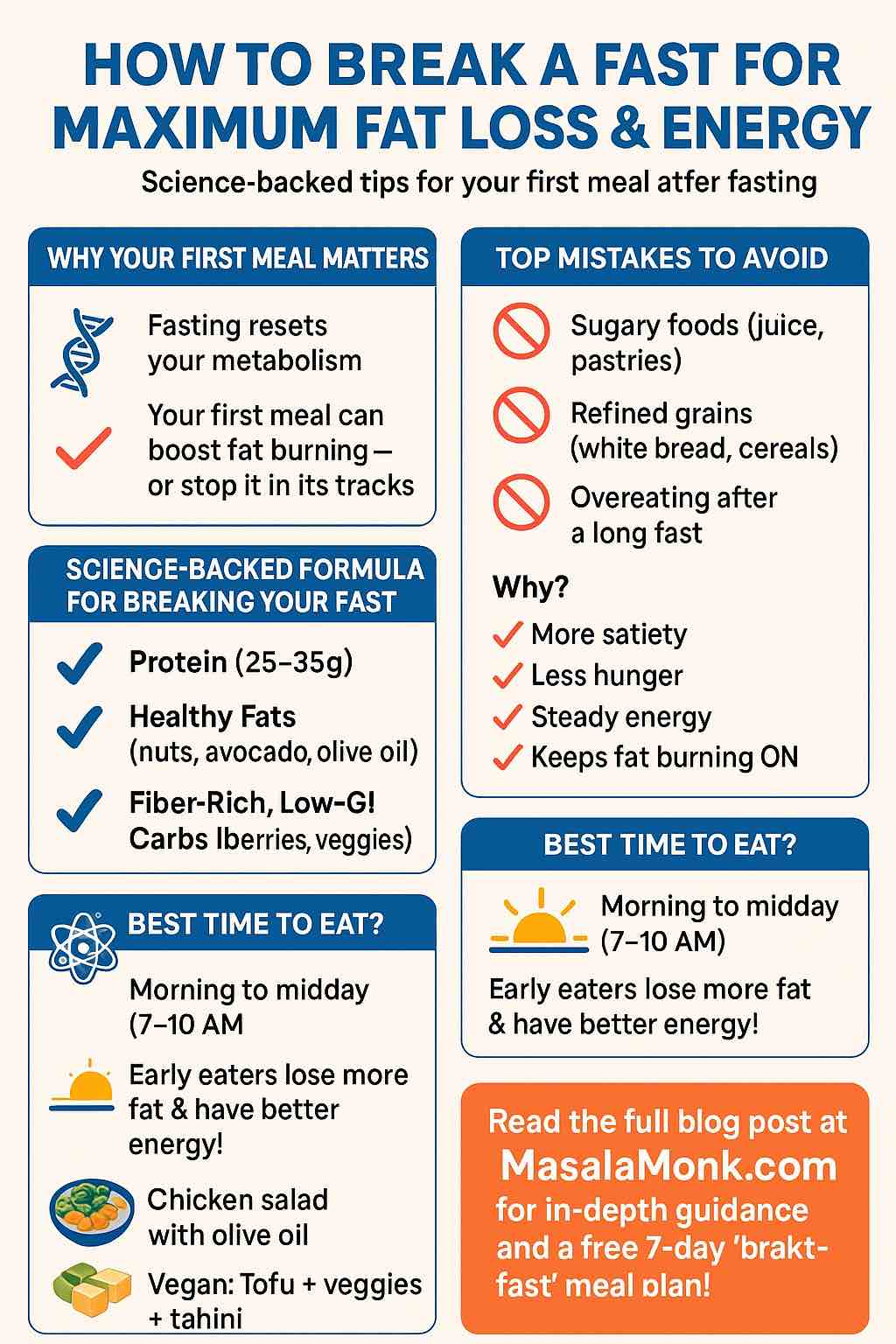
3. Eat Well During Your Window
Fasting is not an excuse to load up on junk food. Real users who see lasting results emphasize:
- High-protein meals for satiety and muscle
- Plenty of fiber (veggies, legumes)
- Healthy fats
- Hydration!
4. Stay Flexible
Life happens. Social meals, holidays, stressful days—it’s OK to break your routine. Long-term success comes from consistency, not perfection.
5. Track More Than Weight
Notice your energy, mood, sleep, and—for women—cycle regularity. These are as important as the scale.
6. Watch for Red Flags
If fasting makes you anxious, preoccupied with food, fatigued, or socially withdrawn, it’s time to reassess.
7. Get Support If Needed
If you have a history of eating disorders, chronic illness, or hormonal issues, check with a healthcare professional before starting or adjusting your IF routine.
What About the Extreme Fasts?
Some users experiment with 24–72 hour (or longer) fasts for “autophagy” or metabolic resets. A few report powerful mental clarity and rapid weight drops. But these are not for most people—and carry real risks: muscle loss, electrolyte imbalances, and even binge cycles when refeeding. Extended fasting should only ever be done with medical supervision.
User Stories: The Spectrum
| Approach | Positive Outcomes | Negative Experiences |
|---|---|---|
| 16:8/18:6 daily discipline | Steady weight loss, better focus | Occasional hunger, boredom |
| OMAD or 24h+ fasts | Rapid fat loss, food freedom | Fatigue, food obsession, burnout |
| Flexible/“sometimes IF” | Improved appetite, easy to sustain | Slower results, less structure |
The Bottom Line
Intermittent fasting can be a powerful tool—when approached with flexibility, awareness, and self-compassion.
For most, moderate routines like 16:8 or 14:10 are enough to see benefits without stress. Remember: more extreme doesn’t always mean better. Your health and happiness come first.
Ready to Try IF?
- Start small, track your progress, and focus on whole foods.
- Ignore the “hardcore” stories if they don’t suit your lifestyle or mental health.
- Be open to adjusting—or even stopping—if it stops serving you.
Your body, your rules.
Questions or want to share your own IF experience? Drop a comment below! Let’s learn together.
Intermittent Fasting FAQs
1. How quickly will I see results with intermittent fasting?
Answer:
Some people notice initial weight loss (mostly water weight) in the first week. Meaningful, sustainable results—like fat loss and improved energy—usually show up after 3–6 weeks, depending on your diet, activity, and consistency.
2. Can I drink coffee, tea, or water during the fasting window?
Answer:
Yes! Black coffee, plain tea, and water are all allowed (and encouraged) while fasting. Just avoid sugar, milk, or cream, as these break the fast.
3. What should I eat when my fasting window ends?
Answer:
Focus on nutrient-dense meals: lean proteins, vegetables, whole grains, healthy fats, and fiber. Avoid breaking your fast with heavy, processed, or sugary foods, which can cause energy crashes.
4. Can I exercise while fasting?
Answer:
Many people successfully exercise during fasting. Light-to-moderate workouts (walking, yoga, weights) are usually fine. Listen to your body, and if you feel weak or dizzy, adjust your eating window or have a small pre-workout snack.
5. Will intermittent fasting slow my metabolism?
Answer:
Short-term fasting does not slow your metabolism. In fact, some research shows a slight boost. Chronic, extreme calorie restriction or long-term aggressive fasting, however, can lead to metabolic slowdown.
6. Is intermittent fasting safe for everyone?
Answer:
No. IF is not recommended for children, pregnant/breastfeeding women, people with a history of eating disorders, or those with certain medical conditions (like uncontrolled diabetes). Always consult your doctor if you have health concerns.
7. What if I feel very hungry or get a headache while fasting?
Answer:
Mild hunger and headaches are common when starting IF. These usually subside after a week or two. Stay hydrated, add a pinch of salt to your water if needed, and make sure your meals are balanced and filling.
8. Do I have to fast every day?
Answer:
No. Many people practice IF on weekdays and relax on weekends, or simply when it fits their lifestyle. Flexibility increases long-term success and sustainability.
9. Can intermittent fasting cause muscle loss?
Answer:
Not if you eat enough protein and maintain resistance exercise. Most people preserve or even build muscle with moderate fasting, as long as they eat well during their eating window.
10. How do I avoid binge eating after breaking my fast?
Answer:
Plan your first meal, eat slowly, and include protein and fiber to stay satisfied. If you notice urges to binge, your fasting window might be too long—shorten it and focus on nourishing foods.