Uric acid might sound like a minor health metric, but if you’ve ever suffered a gout flare—or worried about kidney stones—you know it’s no joke. High uric acid (hyperuricemia) can lead to joint pain, inflammation, and more. Medication can help, but what about natural options? Is it really possible to bring your uric acid down without drugs? Let’s look at the science, real-world experiences, and practical steps anyone can try.
Understanding Uric Acid: The Basics
Uric acid is a natural waste product from breaking down purines, which are found in your body and many foods. Normally, uric acid dissolves in blood, passes through the kidneys, and exits in urine. If your body makes too much or your kidneys can’t remove enough, levels rise—sometimes forming sharp crystals in joints or kidneys.
Symptoms of High Uric Acid (Hyperuricemia):
- Joint pain, swelling, redness (often the big toe—classic gout sign)
- Fatigue
- Kidney stones
- Skin bumps (tophi) in severe cases
But not everyone with high uric acid gets symptoms. That’s why regular monitoring is important, especially if you have risk factors (family history, obesity, metabolic syndrome, high meat/alcohol intake).
How Much Can You Lower Uric Acid Naturally?
Let’s be real:
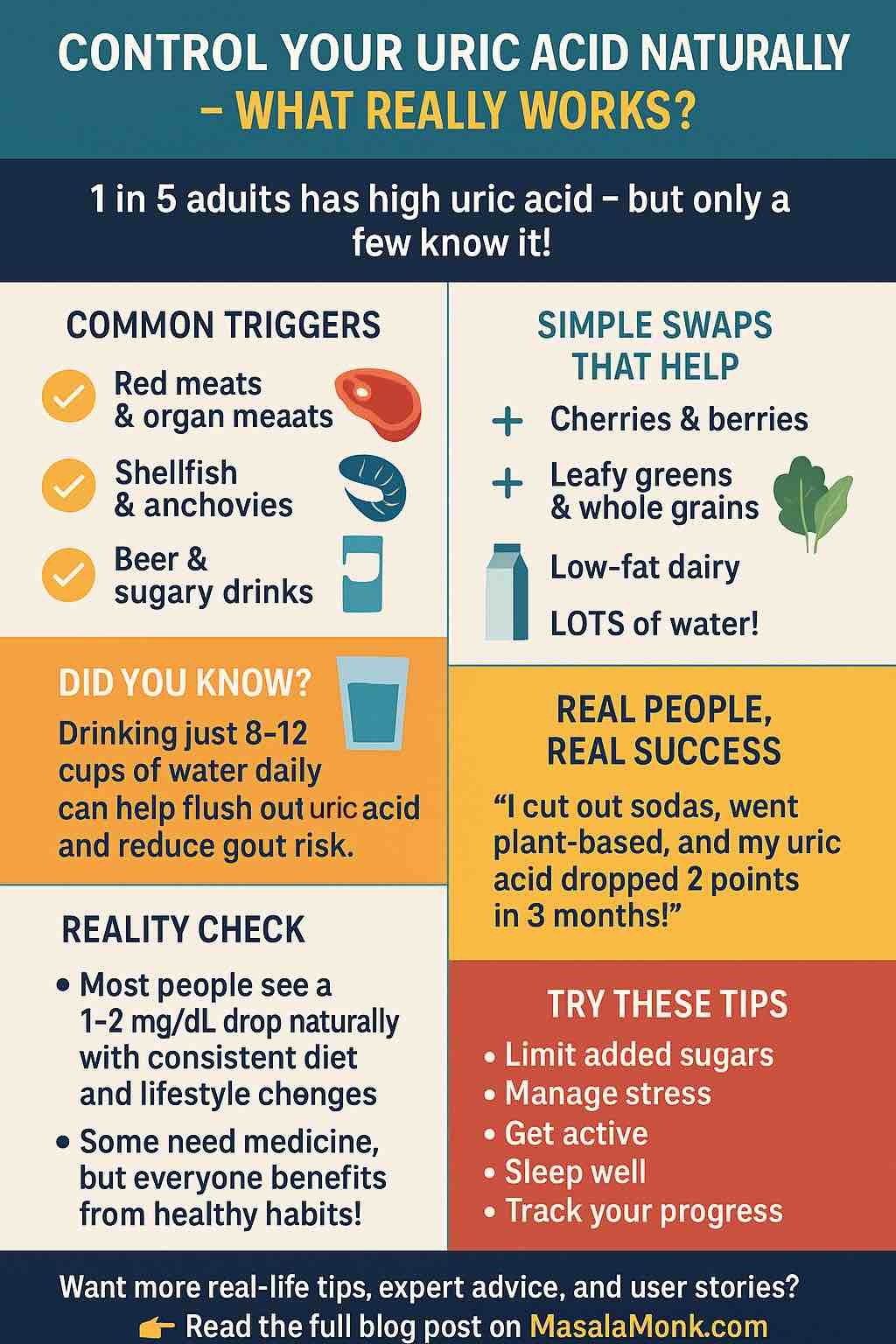
- Small to moderate improvements are possible for most people with diet, hydration, and lifestyle tweaks—often about 1–2 mg/dL (or 60–120 μmol/L).
- Some see bigger changes, especially if their starting diet was very high in purines, sugar, or alcohol.
- Complete control or “cure” without medicine is rare, especially if you’ve already had gout attacks or have chronic kidney disease.
But everyone can benefit from natural strategies, and some people have achieved real success. Here’s how.
Science-Backed Ways to Lower Uric Acid Naturally
1. Overhaul Your Diet: Go Plant-Strong, Limit Purines
- Plant-based and Mediterranean-style diets (think: lots of veggies, whole grains, nuts, olive oil, some fish, low-fat dairy) consistently reduce uric acid in research and real life.
- A big review in 2024 found that plant-based eaters had a 17% lower risk of high uric acid compared to heavy meat and sugar eaters.
- What to cut: Red meats, organ meats, shellfish, anchovies, sugary drinks, beer.
- What to eat: Leafy greens, berries, cherries, citrus, whole grains, lentils, beans, nuts, low-fat yogurt/milk.
User quote:
“I went mostly plant-based, cut out sodas and beer, and my UA dropped from 8.7 to 6.3 in four months. Fewer flare-ups too.” (Reddit user)
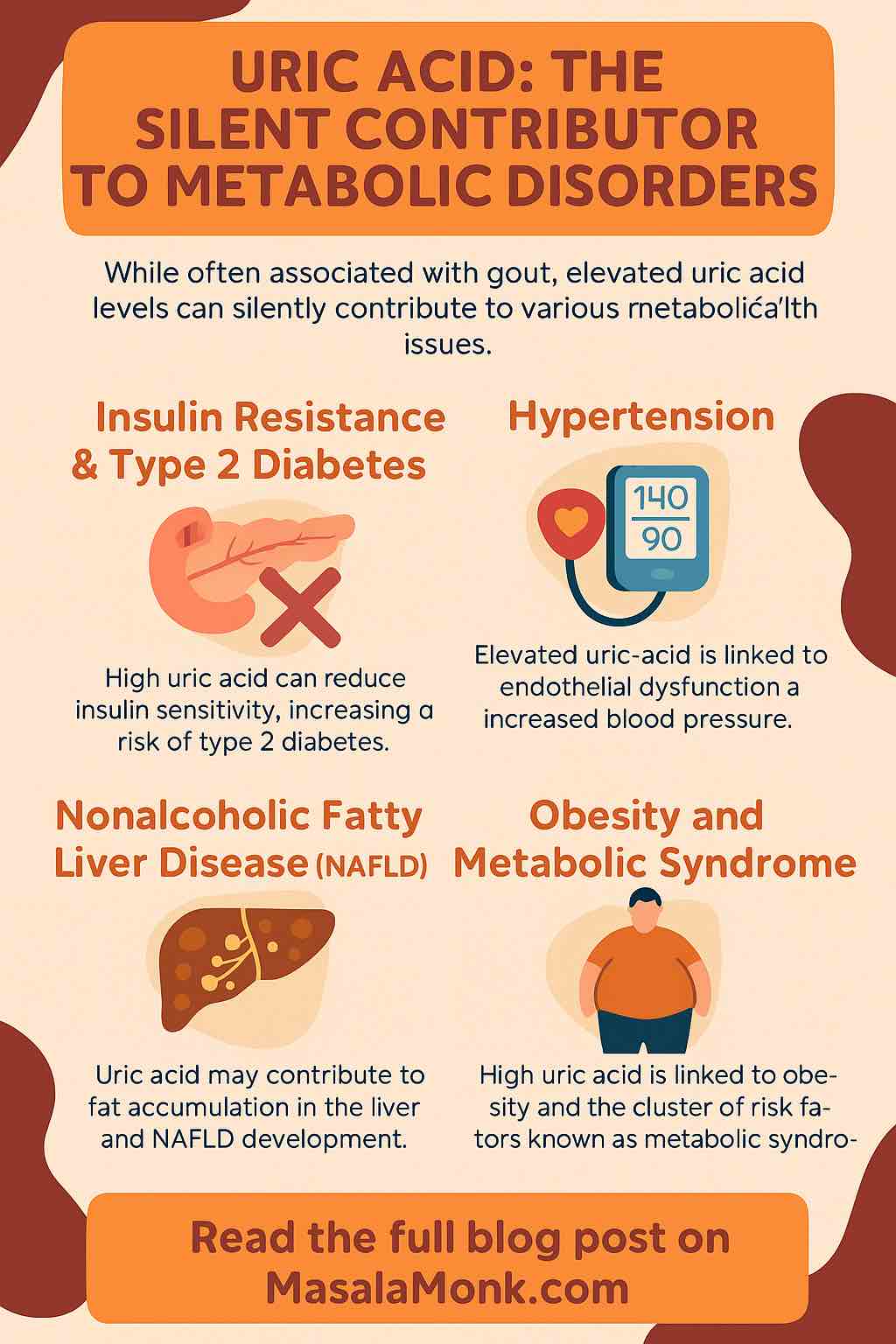
Read More: What is Uric Acid? The Silent Contributor to Metabolic Disorders
2. Stay Hydrated—Water Is Your Friend
- Aim for at least 2–3 liters of water a day (8–12 cups). Water helps flush uric acid out via urine.
- Herbal teas and lemon water are good extras; avoid sodas and juices.
User tip:
“I drink lots of water with lemon every day—definitely notice less joint pain and fewer kidney stone issues.” (Reddit)
3. Cut Sugar, Especially Fructose
- Fructose (found in sodas, sweets, fruit juices, processed foods) is a major uric acid trigger.
- Reducing added sugars and sweet drinks is one of the quickest wins for most people.
4. Moderate Your Alcohol (Especially Beer and Spirits)
- Alcohol, particularly beer, is notorious for raising uric acid.
- Wine is less risky, but moderation is key—try alcohol-free weeks if possible.
5. Try Short-Term Low-Purine Diets
- Studies show a strict low-purine diet can lower uric acid by 10–12% in just two weeks.
- Not always sustainable long-term, but a great jump-start—then shift to a balanced Mediterranean-style approach for maintenance.
6. Supplements With Research Support
- Vitamin C: 500 mg daily can lower uric acid slightly (~20 μmol/L), but talk to your doctor if you have kidney issues.
- Quercetin Phytosome™ (e.g., Quevir®): 2025 studies show up to 15% UA reduction in 3 months—promising, but discuss with your doctor first.
- Folic acid and probiotics: Recent meta-analyses show good effect (up to 40–60 μmol/L reductions), but clinical use should be individualized.
7. Eat More of These “Natural Helpers”
- Cherries: Several studies show cherries and tart cherry juice can lower uric acid and reduce gout flare risk.
- Coffee (black or with low-fat milk): Moderate consumption may lower gout risk.
- Low-fat dairy: Yogurt and skim milk support uric acid excretion.
Read more: Cherries and Arthritis: Are Cherries Good for Arthritis?
8. Get Active and Lose Extra Weight
- Even modest, steady weight loss lowers uric acid.
- Regular activity improves metabolism and reduces inflammation.
9. Manage Stress & Sleep
- Stress can trigger flares and metabolic issues.
- Prioritize good sleep and use stress-busting routines: exercise, meditation, social time, or hobbies.
User insight:
“Biggest gout trigger? Stress. Once I got serious about work-life balance, my flares dropped way off—even more than with diet alone.” (Reddit)
What Real People Say: Honest Experiences
Success Stories
- “Strict diet, hydration, and lots of lemon water—dropped my UA from 9.1 to 5.9 in three months.”
- “Plant-based eating cleared my flares for 2+ years after nothing else worked.”
- “Cutting sugar made a bigger difference than anything else. I wish I’d known sooner.”
Realistic Warnings
- “I did everything right, but still couldn’t get below 7 without meds. Diet helps, but sometimes it’s just genetics.”
- “My doctor said not to expect more than 1–2 mg/dL drop from food alone—he was right.”
- “Apple cider vinegar and celery seed did nothing for me. Everyone’s different.”
Potential Pitfalls and What to Watch Out For
- Natural approaches work best for mild cases or prevention; if you’ve already had flares, you may need meds.
- Results vary by person: genetics, kidney function, and severity all play a role.
- Be careful with supplements: some (e.g., high-dose vitamin C, herbal remedies) can interact with medications or cause kidney stones.
- Too strict, unsustainable diets can cause rebound flares or nutrient deficiencies—balance matters!
Step-by-Step Plan: Lowering Uric Acid Naturally
1. Get a Baseline:
- Know your uric acid number—ask your doctor for a blood test.
2. Make Diet Swaps:
- Replace red meats with beans, lentils, tofu, or fish.
- Ditch sodas and juice for water, lemon water, or herbal tea.
- Load up on veggies, whole grains, cherries, and low-fat dairy.
3. Hydrate, Hydrate, Hydrate:
- Set water reminders on your phone.
4. Move More:
- Even 20–30 min of walking daily helps.
5. Limit Alcohol and Added Sugars:
- Try “Dry January” or “Sober October” for a reset.
6. Sleep and De-stress:
- Prioritize sleep; try mindfulness apps or yoga.
7. Track Progress:
- Retest uric acid in 8–12 weeks. Adjust as needed.
8. Be Patient & Realistic:
- Small changes add up; some progress is better than none.
When to See a Doctor
- If you have frequent or severe flares.
- If uric acid stays above target despite your best efforts.
- If you have kidney stones, tophi, or other complications.
Natural methods are great—but not a substitute for expert medical care. Always check before starting new supplements or drastically changing your diet.
Final Thoughts: Your Journey, Your Results
Managing uric acid is a marathon, not a sprint. The research and real-life stories agree:
- Natural strategies work, especially when done consistently and combined.
- You may see impressive drops—or just modest improvements.
Either way, you’ll likely feel better, reduce your risk of flare-ups, and improve your overall health.
Ready to try? Start small, stay curious, and celebrate your wins—no matter how minor. If you want support, online communities (like r/gout) are full of people sharing their own journeys, challenges, and victories.
Have you tried to lower your uric acid naturally? What’s worked (or not worked) for you? Share your experience below or reach out for support!
References:
- Reddit r/gout
- Latest clinical trials & systematic reviews, 2024–2025
- Verywell Health: Gout Diet
- Times of India: Uric Acid Diet
- Recent medical reviews 2025
10 Frequently Asked Questions (FAQs) About Natural Uric Acid Control
1. What causes high uric acid levels?
High uric acid can be caused by genetics, eating too many purine-rich foods (like red meat and shellfish), obesity, drinking too much alcohol or sugary drinks, kidney problems, certain medications, or rapid weight loss.
2. Can you lower uric acid levels naturally without medication?
Yes, many people can lower uric acid by improving their diet (more vegetables, less meat and sugar), increasing hydration, losing excess weight, and limiting alcohol. However, severe cases or those with gout flares often need medication.
3. What foods should I avoid if I have high uric acid?
Avoid or limit red meats, organ meats, shellfish, anchovies, sardines, beer, sugary drinks, and high-fructose foods. These are highest in purines or increase uric acid production.
4. What foods help lower uric acid naturally?
Fruits (especially cherries), low-fat dairy, whole grains, vegetables, nuts, seeds, and legumes. Coffee (in moderation) and vitamin C–rich foods can also help.
5. How much water should I drink to help lower uric acid?
Aim for 2–3 liters (8–12 cups) of water per day. Staying hydrated helps your kidneys flush out excess uric acid.
6. Can supplements like vitamin C or quercetin really help?
Research shows that 500 mg of vitamin C daily or quercetin phytosome may modestly lower uric acid. Effects are usually mild and should be discussed with your doctor, especially if you have kidney issues.
7. How fast can I expect results from natural uric acid control?
Some people see improvement in 2–4 weeks, especially with strict diet and hydration. For others, it may take several months. Medication may be needed if natural changes aren’t enough.
8. Are there any risks to natural uric acid remedies?
Strict or unbalanced diets can lead to nutrient deficiencies. Some supplements may interact with medications or worsen kidney stones. Always consult your healthcare provider before major changes.
9. Can stress and lack of sleep affect uric acid levels?
Yes, both stress and poor sleep can raise inflammation and may trigger gout flares or worsen metabolic health, making it harder to control uric acid.
10. When should I see a doctor about high uric acid?
If you have frequent gout attacks, persistent joint pain, kidney stones, tophi, or uric acid stays high despite lifestyle changes, see your doctor for assessment and possible medication.