Scrotal eczema is one of those conditions that people don’t talk about openly, but it affects thousands of men worldwide. It’s uncomfortable, persistent, and can significantly impact quality of life. If you’re reading this, chances are you’re seeking clarity, solutions, or maybe just reassurance that you’re not alone. This guide breaks everything down—from what causes scrotal eczema to how you can manage and treat it effectively.
What Is Scrotal Eczema?
Scrotal eczema (also known as genital eczema or scrotal dermatitis) is a type of skin inflammation that occurs on or around the scrotum. It causes itching, redness, dryness, scaling, and sometimes even painful cracking or oozing. It’s often misdiagnosed as a fungal infection, especially in early stages.
Common Symptoms
- Persistent itching or burning sensation
- Red or darkened skin
- Dry, flaky, or leathery patches
- Raw, weeping, or cracked skin in severe cases
- Thickened skin (lichenification) from chronic scratching
Causes and Triggers
1. Irritants and Allergens
- Soaps, detergents, fabric softeners
- Fragranced lotions or wipes
- Latex condoms, spermicides, or lubricants
2. Friction and Moisture
- Tight or synthetic underwear
- Excessive sweating
- Long periods of sitting or activity in warm environments
3. Underlying Health Factors
- Stress and anxiety (can worsen symptoms)
- Nutritional deficiencies (especially riboflavin and zinc)
- A history of other skin conditions (like atopic dermatitis)
Diagnosis: Ruling Out the Imitators
Scrotal eczema often mimics other conditions like:
- Jock itch (fungal infection)
- Psoriasis
- Bacterial infections
- Sexually transmitted infections (STIs)
If over-the-counter antifungals or antibiotics haven’t helped, it’s time to see a dermatologist. Patch testing, skin biopsies, or fungal cultures might be used for accurate diagnosis.
Treatment Options
1. Topical Treatments
Corticosteroids
- Low- to mid-potency topical steroids like hydrocortisone or triamcinolone are first-line treatments.
- Use only short-term and under medical guidance due to the risk of skin thinning.
Calcineurin Inhibitors (Non-steroidal)
- Tacrolimus or pimecrolimus offer inflammation relief without thinning the skin.
- May cause mild burning at first but often resolves with continued use.
Crisaborole
- A non-steroidal PDE-4 inhibitor approved for sensitive areas.
- Useful for long-term management of mild to moderate eczema.
2. Moisturization (Emollients)
- Apply fragrance-free ointments or creams multiple times a day.
- Always apply after bathing and before bed.
- Let moisturizers and medications absorb separately (wait 20-30 minutes between).
3. Hygiene & Lifestyle Adjustments
- Wash with warm water and fragrance-free, non-soap cleansers.
- Wear loose-fitting, breathable cotton underwear.
- Avoid over-washing or scrubbing.
- Stay cool and dry: talc-free powders can help in humid climates.
4. Advanced Therapies
- Phototherapy (UVB): Effective for chronic, stubborn cases.
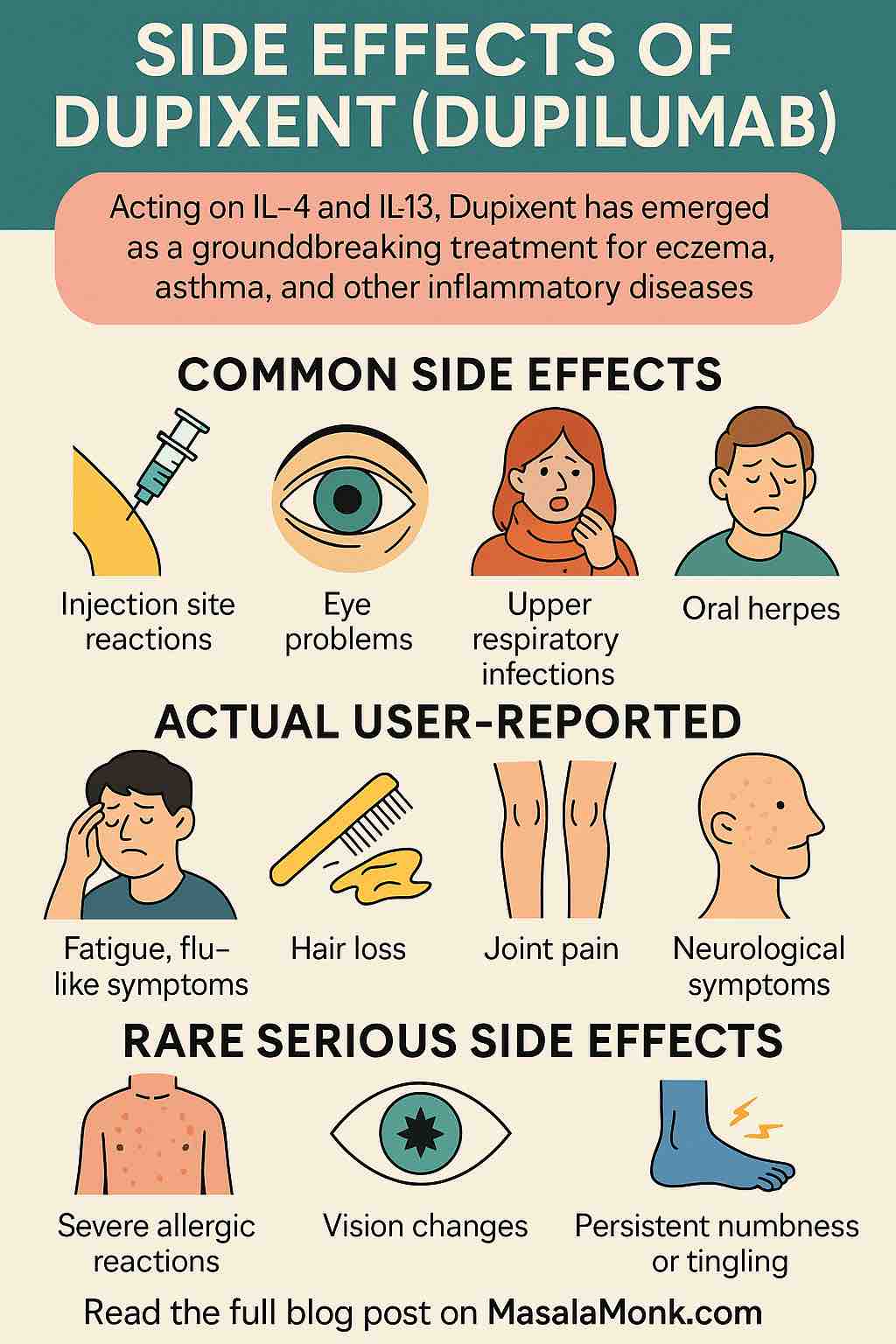
- Systemic Treatments: Reserved for severe flare-ups, including oral steroids, cyclosporine, or newer biologics like dupilumab.
Managing Chronic Scrotal Eczema
When eczema becomes chronic, the skin thickens and darkens due to repeated scratching (a condition called lichen simplex chronicus). In such cases, treatment may include:
- Short bursts of potent corticosteroids
- Barrier creams
- Night-time antihistamines to reduce nocturnal itching
- Addressing psychological triggers like stress or compulsive scratching
Prevention and Maintenance
Preventing flare-ups requires diligence:
- Stick to your skincare routine even when symptoms improve.
- Know your personal triggers and avoid them.
- Keep a diary to track flare-up patterns.
- Regularly moisturize and wear breathable clothing.
When to See a Doctor
- If symptoms persist beyond a few weeks
- If you notice signs of infection: pus, increased redness, warmth, or pain
- If over-the-counter remedies don’t help
- If you’re unsure whether it’s eczema or something else
Final Thoughts
Scrotal eczema is treatable, manageable, and more common than you might think. The key lies in identifying your triggers, sticking to a treatment routine, and not being afraid to seek professional help. With the right approach, you can break the itch-scratch cycle, heal your skin, and take back control of your comfort and confidence.
If you’ve been struggling with scrotal eczema and feel like you’re getting nowhere, you’re not alone—and you’re not out of options. Relief is possible. And now, you’ve got a plan.
❓ FAQs: Scrotal Eczema
- What’s the difference between scrotal eczema and jock itch?
Scrotal eczema is an inflammatory skin condition, not caused by infection. Jock itch (tinea cruris) is a fungal infection. Eczema tends to affect both sides evenly and doesn’t respond to antifungals, while jock itch often has a raised red border and improves with antifungal treatment. - Can scrotal eczema be cured permanently?
There’s no permanent cure, but it can be effectively managed and controlled. With consistent skincare, trigger avoidance, and proper treatment, many people experience long-term relief. - Is scrotal eczema contagious?
No. Eczema is not infectious or contagious. It cannot be spread through sexual contact, skin-to-skin contact, or shared items. - Can stress really cause flare-ups?
Yes. Psychological stress is a known trigger for eczema. Managing stress through techniques like meditation, sleep hygiene, and therapy can reduce flare-ups. - Are over-the-counter treatments enough?
Mild cases may improve with OTC moisturizers and low-strength hydrocortisone. Persistent or severe cases usually require prescription treatments and dermatologist guidance. - Is it safe to use steroid creams on the scrotum?
Yes, but only low- to mid-potency steroids and only under medical advice. The skin in this area is sensitive, and overuse can cause thinning or damage. - What are the best types of underwear for someone with scrotal eczema?
Loose-fitting, 100% cotton underwear is best. Avoid tight, synthetic fabrics that trap heat and moisture. - Can diet affect scrotal eczema?
There’s limited direct evidence, but deficiencies in zinc or riboflavin may play a role. An anti-inflammatory diet and staying hydrated can support overall skin health. - What if eczema doesn’t respond to treatment?
If standard therapies fail, you may need advanced options like tacrolimus, crisaborole, or phototherapy. A dermatologist can also reassess the diagnosis or check for overlapping conditions like psoriasis. - Can scrotal eczema affect sexual activity?
It may cause discomfort or self-consciousness, but it doesn’t affect sexual function. Communicating with your partner and avoiding irritants (like latex or scented products) can help.