1. Introduction
Eczema, a prevalent skin condition, is often a source of discomfort and distress. When coupled with sweating, managing eczema can become an even more challenging task. Sweating, a natural body process, can unfortunately exacerbate eczema symptoms, leading to increased irritation and discomfort. In this guide, we will explore the intricate relationship between eczema and sweating, delving into aspects such as night sweats, sweat-induced eczema, and the impact of hyperhidrosis on this skin condition.
2. Eczema Night Sweats: A Restless Battle
Night sweats can be a common occurrence for individuals battling eczema, turning restful nights into restless discomfort. The combination of the body’s natural nighttime temperature regulation and the irritation caused by sweat can lead to disrupted sleep and heightened discomfort.
- Understanding the Link: Eczema flares can often lead to an increase in body temperature, and when combined with the body’s propensity to sweat more at night, this can result in a cycle of night sweats and irritation.
- Managing Night Sweats: Ensuring a cool and comfortable sleeping environment, choosing breathable fabrics for bedding and nightwear, and maintaining a consistent bedtime routine can be beneficial in managing night sweats related to eczema.
3. Sweat Eczema: The Uncomfortable Reality
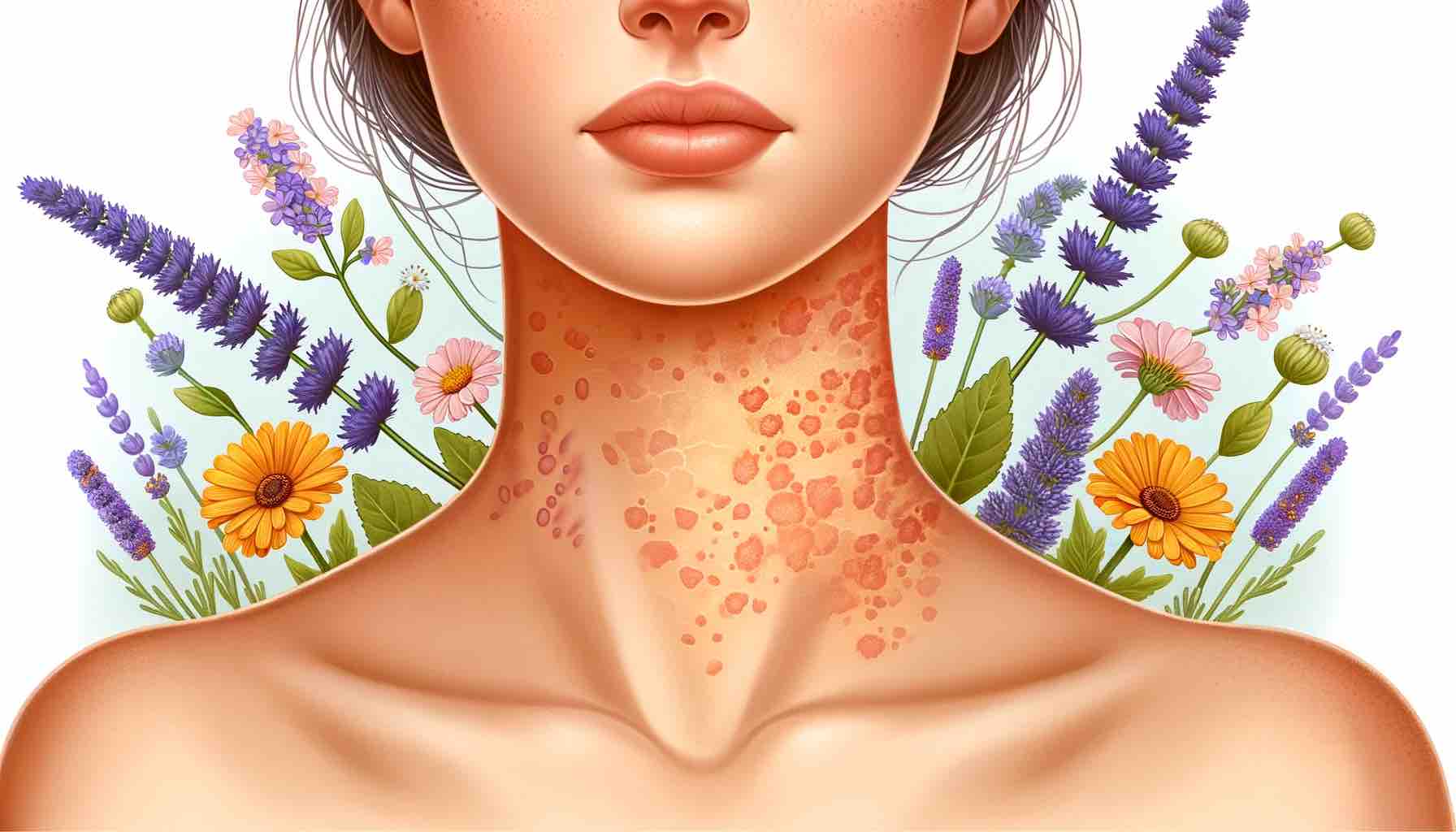
Sweat, while a natural body response, can be a trigger for eczema flares. Areas prone to sweating, such as the folds of the elbows, knees, and neck, can become hotspots for eczema irritation.
- Recognizing Sweat-Induced Eczema: Identifying the correlation between sweating and increased eczema irritation is crucial. Awareness allows for the implementation of strategies to manage and mitigate symptoms effectively.
- Practical Management Strategies: Regularly changing out of sweaty clothes, rinsing the skin gently after sweating, and ensuring the skin is dry but moisturized can help in managing sweat-induced eczema.
4. Hyperhidrosis: Excessive Sweating and Eczema
Hyperhidrosis, or excessive sweating, can be particularly challenging when dealing with eczema. The increased sweat production can lead to heightened skin irritation and exacerbate eczema symptoms.
- Understanding Hyperhidrosis: Recognizing whether excessive sweating is a consistent issue is essential, as it allows for targeted strategies and treatments to be applied.
- Navigating Eczema with Hyperhidrosis: Managing eczema with hyperhidrosis involves a careful balance of managing sweat production while ensuring that the skin is not overly dried or irritated.
5. Heat Rash: A Common Culprit
Heat rash, while distinct from eczema, can often co-occur, leading to increased skin irritation and discomfort. Understanding the differences, similarities, and management strategies for both conditions is essential for effective care.
- Differentiating Between Eczema and Heat Rash: While both conditions can lead to irritated and inflamed skin, recognizing the distinct characteristics of each can guide effective management strategies.
- Co-Management Strategies: When dealing with both conditions, strategies such as staying cool, wearing breathable fabrics, and avoiding irritants become crucial.
In each section, practical insights, expert guidance, and actionable strategies are provided to navigate the challenges of managing eczema in the presence of sweating and related conditions. For a deeper understanding and more specific guidance, you might find the following articles helpful:
- Eczema and Dermatitis Causes and Coping Mechanisms
- Soothing the Itch: Guide to Eczema Relief
- Oatmeal Baths: Remedy for Eczema and Dermatitis
6. Allergic to Sweat: Eczema’s Unfriendly Companion
Believe it or not, some people find that their sweat exacerbates their eczema symptoms. This condition, where one seems to be allergic to their sweat, adds another layer of complexity to managing eczema.
- Understanding the Reaction: Knowing that sweat can be an irritant helps in formulating a strategy to manage eczema better. It’s essential to recognize the signs and understand how sweat might be affecting your skin.
- Strategies for Management: Quick showers post-exercise, wearing breathable fabrics, and using gentle skincare products can be part of a strategy to minimize the impact of sweat on eczema.
7. Eczema in Sweaty Areas: Targeted Care
Certain areas of the body tend to sweat more, and when these areas are also affected by eczema, targeted care is necessary.
- Identifying Problem Areas: Common areas include the folds of the elbows and knees, the neck, and the feet. Identifying these areas can help in applying targeted care.
- Customized Care Strategies: Using absorbent powders, choosing appropriate clothing, and applying specialized skincare products can help manage eczema in these sweat-prone areas.
8. Sweat-Induced Dermatitis: A Close Relative
Sweat-induced dermatitis is closely related to eczema, where sweat irritates the skin, leading to a rash or irritation.
- Recognizing the Signs: Understanding the signs of sweat-induced dermatitis, such as redness, itching, and inflammation, is crucial for effective management.
- Management Techniques: Keeping the skin clean and dry, avoiding occlusive clothing, and using hypoallergenic skincare products are essential management techniques.
9. Practical Tips and Remedies
Managing eczema with the added challenge of sweating requires a toolbox of practical tips and remedies. Here are some strategies that might help:
- Stay Cool: Try to keep your body temperature regulated to avoid excessive sweating.
- Choose Fabrics Wisely: Opt for breathable, natural fabrics that wick away moisture.
- Hygiene: Maintain a routine of gentle cleansing to avoid the accumulation of sweat and irritants on the skin.
10. Related Articles and Resources
For more in-depth information and strategies to manage eczema and sweating, consider exploring the following articles:
- Ear Eczema and Dermatitis: Unveiling the Mystery
- Foods to Embrace and Avoid for Eczema Relief
- Exploring Eucrisa: An Eczema Solution
This guide aims to provide a comprehensive overview, practical strategies, and resources to manage eczema in the presence of sweating and related challenges. Remember, a personalized approach, often guided by a healthcare professional, is usually the most effective in managing eczema.
FAQs
- What is the connection between sweat and eczema flare-ups? Sweat contains salt and other irritants that can exacerbate eczema symptoms. When sweat dries on the skin, it can lead to irritation, itching, and flare-ups.
- How can I manage eczema in areas prone to sweating? Focus on keeping the areas clean and dry. Consider using absorbent powders and wearing breathable fabrics to reduce moisture accumulation.
- Can certain fabrics help in managing sweat-related eczema flare-ups? Yes, choosing natural, breathable fabrics like cotton can help in managing sweat and reducing the irritation caused by it.
- Is it possible to be allergic to one’s own sweat? While not technically an allergy, some people find that their sweat seems to exacerbate their eczema symptoms, acting as an irritant.
- What kind of hygiene practices are helpful in managing sweat-induced eczema flare-ups? Regular showers, using mild cleansers, and keeping the skin dry are essential hygiene practices to manage sweat-induced eczema.
- Are there specific treatments available for sweat-induced eczema? Treatments like topical steroids, emollients, and antifungal creams can be beneficial, but it’s best to consult a dermatologist for a personalized approach.
- How does heat and humidity affect eczema? Heat and humidity can increase sweating, which may act as an irritant, triggering eczema flare-ups in susceptible individuals.
- Can lifestyle modifications help in managing eczema aggravated by sweat? Lifestyle modifications such as staying in cool environments, wearing appropriate clothing, and managing stress can play a role in managing such eczema.
- What role do skincare products play in managing eczema related to sweating? Skincare products like moisturizers and barrier creams can help protect the skin, while the choice of cleansers can help prevent irritation.
- How can I prevent sweat from worsening my eczema during workouts? Try to workout in cool environments, wear breathable fabrics, and ensure that you shower immediately after exercising to remove sweat.
Blog Tags
eczema, sweating, dermatitis, skin care, eczema management, sweat-induced eczema, eczema flare-ups, eczema remedies, eczema treatment, skin irritation