If you’ve ever been jolted awake at night by that burning sensation creeping up your chest, you know heartburn is more than just a minor nuisance. For many, it’s a daily struggle—ruining dinners, spoiling sleep, and making simple pleasures feel risky. The good news? You don’t have to reach for harsh meds every time. There’s a whole toolkit of natural, practical, and fast-acting remedies—many hiding right in your kitchen!
In this post, we’ll cut through the noise. No snake oil, no vague advice. Just what actually works, how fast, and what real people say. Let’s dig in.
What Is Heartburn, Really?
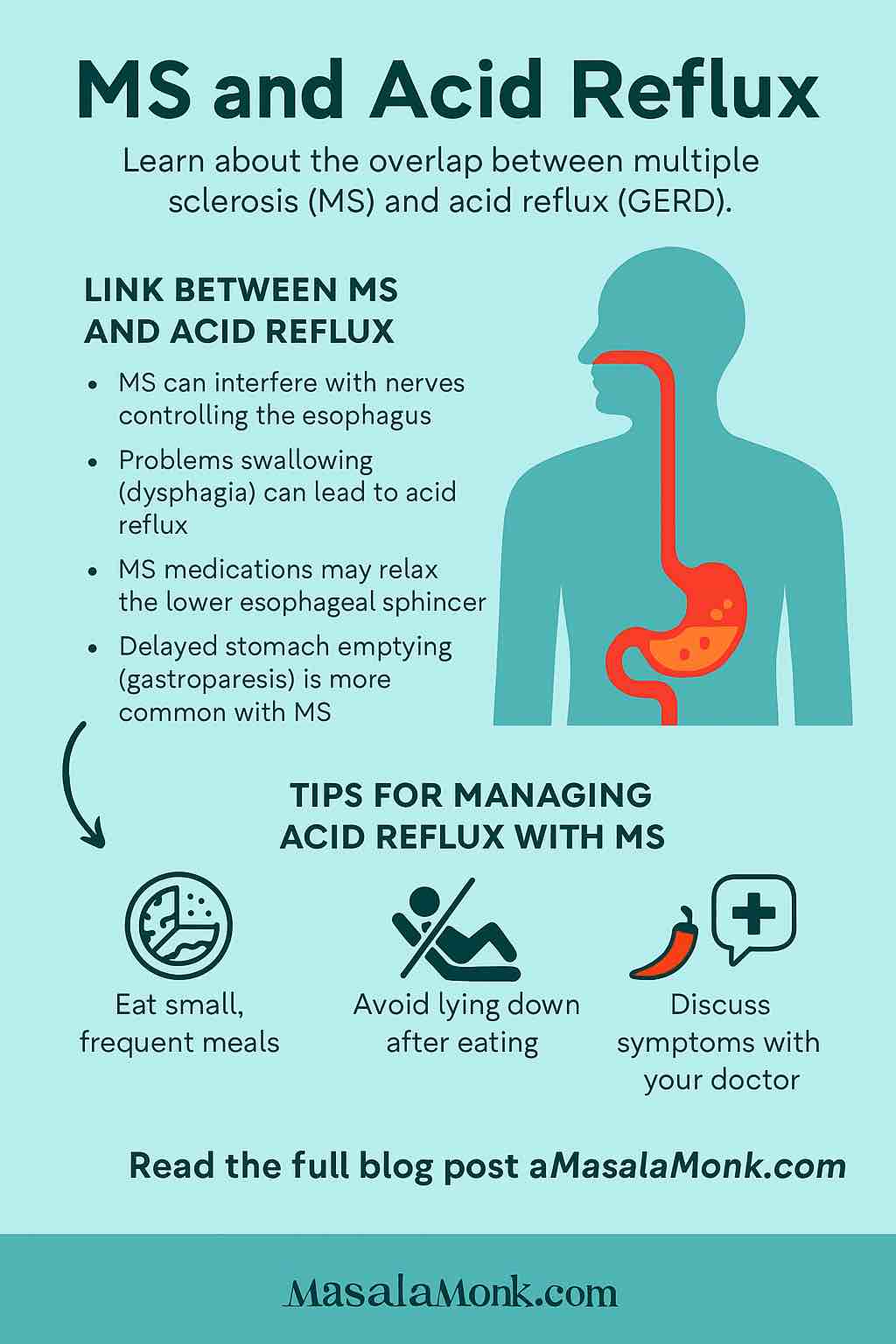
Before you fix it, it helps to know the basics. Heartburn happens when stomach acid backs up into your esophagus, causing that familiar burn. Common culprits? Spicy foods, large meals, alcohol, stress, and sometimes just lying down after eating.
Quick fact: Heartburn and acid reflux are closely related, but not identical. GERD (gastroesophageal reflux disease) is the chronic, more severe version.
Natural Heartburn Remedies That Actually Work
Here are the top tried-and-tested remedies—from clinical research and Redditors alike—ranked by how fast and reliable they are.
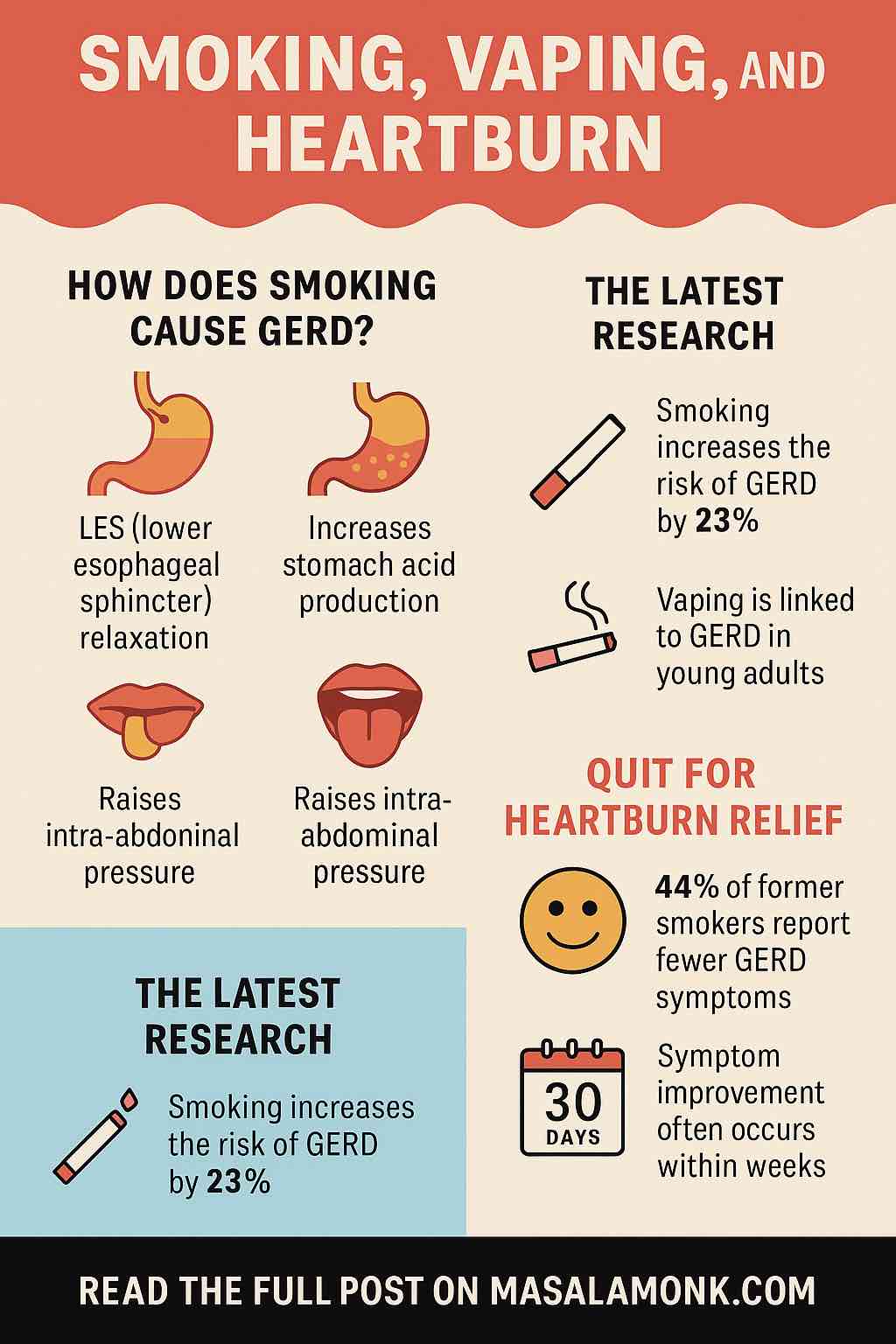
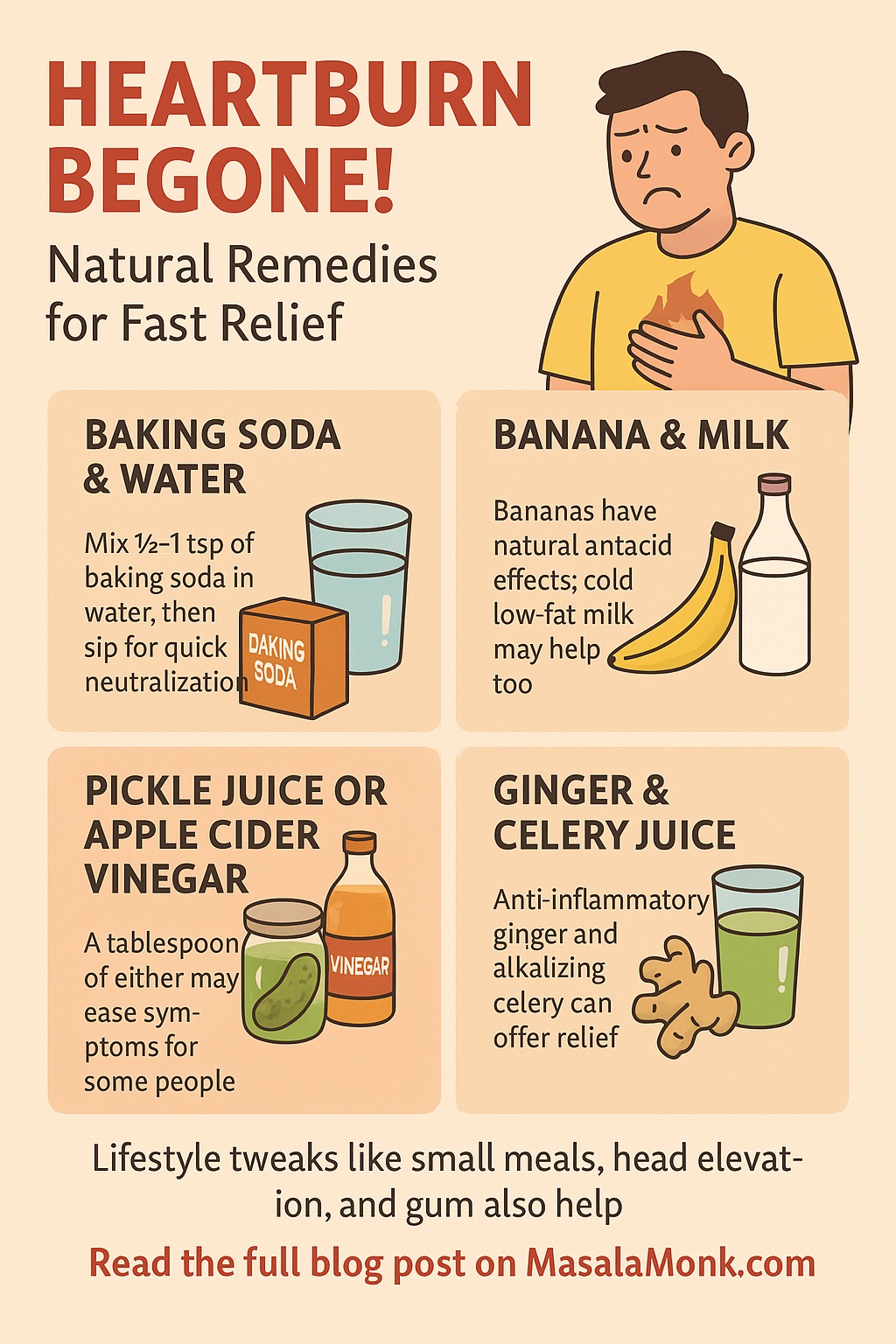
1. Baking Soda & Water: The “Fire Extinguisher”
- How it works: Baking soda (sodium bicarbonate) neutralizes stomach acid in minutes.
- How to use: Mix ½ to 1 teaspoon in a glass of cold water, stir, and sip slowly.
- What real people say: “One or two teaspoons, then stay upright—massive burp, burning is gone.” (Reddit)
- Cautions: High in sodium; don’t use more than once every few days.
Pro tip: Don’t chug it! Sipping slowly works better and is easier on your stomach.
2. Banana, Milk, and Soothing Foods
- Banana: The gentle fruit. Its natural antacid effect soothes the esophagus.
- “If my acid reflux is acting up, I eat a banana. Works wonders for me!” (Reddit)
- Milk (or oat/almond milk): Sips of cold, low-fat milk can ease the burn for some.
- Heads up: For others, especially with full-fat milk, it can sometimes make things worse later.
- Honey lozenges: Sucking on honey-based lozenges stimulates saliva, which helps wash acid down.
3. Pickle Juice or Apple Cider Vinegar (ACV): The Contrarian Fix
- How it works: A tablespoon of vinegar (especially ACV) or pickle juice can trigger your stomach to regulate acid production.
- What real people say:
- “A tablespoon of apple cider vinegar in water—heartburn gone.”
- “Pickle juice, just a sip, sounds weird but instant relief.”
- Why it works (sometimes): Some people’s heartburn is from too little acid, not too much. This trick “resets” stomach acidity.
- Cautions: Try in small amounts, and stop if it makes things worse.
4. Ginger & Celery Juice (for the Naturalists)
- How it works: Ginger is a classic anti-nausea, anti-inflammatory root. Celery is highly alkaline.
- How to use: Juice fresh ginger (just a sliver!) and celery (a few stalks) and sip on an empty stomach.
- What people say:
- “Ginger tea or celery juice in the morning—I’m off meds!”
- Downsides: Some find prep a hassle, but it’s a great long-term solution.
5. Chewing Gum, Lozenges & Water
- Why it works: Chewing gum or sucking lozenges increases saliva, which helps neutralize acid and push it back down.
- What works best: Sugar-free gum, especially after meals.
- “Chewing gum after dinner is my secret weapon.” (Reddit)
- Don’t forget: A big glass of water can help rinse acid down, especially in mild cases.
6. Mechanical Tricks: The “Burp Bubble”
- How it works: Swallow air (like you’re about to burp) and “hold it in” to create a pressure bubble above your stomach, which some people swear blocks reflux for a few minutes.
- “Swallow air, hold it, stay upright—instant blockade!”
- Is it weird? Yes. But if you’re desperate and upright, worth a try.
7. Ayurvedic and Indian Pantry Staples
For readers in India (or with a good spice cabinet!), these “desi” remedies are gaining scientific respect:
- Curd (plain yogurt): Soothes the stomach, provides probiotics.
- Coconut water: Mildly alkaline and hydrating.
- Jeera (cumin) water: Boil cumin seeds, cool, sip.
- Fennel seeds (saunf): Chew after meals to aid digestion.
“Curd, coconut water, and saunf are my go-to for any acidity. I hardly need meds now.” (Times of India, user stories)
8. Alkaline Water: The Latest Science
- What’s new: Water with a pH >8 can neutralize pepsin (an enzyme that damages the esophagus), offering fast relief.
- How to use: Look for bottled “alkaline water” or add a pinch of baking soda to regular water.
- Bonus: Staying hydrated always helps flush acid down.
| Remedy | Speed | Evidence | Benefits | Risks/Cautions |
|---|---|---|---|---|
| Baking soda | Immediate | Moderate–High | Fast neutralization | Overuse → alkalosis, high sodium |
| Aloe vera juice | 10–30 min | Moderate | Soothes, mucosal healing | Use decolorized only; possible interactions |
| Ginger tea | 10–30 min | Moderate | Reduces inflammation/nausea | Too much → may worsen symptoms |
| Banana, papaya | 15–30 min | Low–Moderate | Alkaline, digestive enzymes | Minimal — but vary by individual |
| Chewing gum | 20–30 min | Low–Moderate | Increases clearance | Sugar-free only; limited studies |
| Cold milk/curd | Immediate | Traditional | Buffering acid, probiotics | Full-fat may worsen reflux |
Lifestyle Tweaks for Long-Term Relief
Quick fixes are great, but sustained change wins. Here’s what actually works, according to thousands of forum users:
- Don’t lie down after eating: Wait at least 2–3 hours.
- Raise your head: Elevate your bed by 6–8 inches if you get night heartburn.
- Eat small, frequent meals: Big meals = big reflux.
- Lose a bit of weight (if you need to): Even a few kg can make a difference.
- Track your triggers: Spicy food, caffeine, chocolate, tomatoes, and alcohol are classic offenders.
What NOT to Do
- Don’t chug full-fat milk every time—for some, it’s a quick fix; for others, a rebound trigger.
- Don’t rely on baking soda daily—it’s for emergencies, not routine.
- Be cautious with peppermint tea—it relaxes the valve that keeps acid down, making heartburn worse for many.
Real Stories: What Worked for Others
- Jatin (Delhi): “Heartburn hit every night. Curd and coconut water after dinner changed my life. I only use antacids when traveling now.”
- Emily (US): “I keep a banana at my bedside and a pack of sugar-free gum. If I wake up burning, one or both get me back to sleep.”
- Rakesh (Reddit): “First time in years I fixed it naturally—pickle juice shot, then a walk, then celery juice. Magic.”
| Remedy | Real Mentioned? | How It’s Described | Notes |
|---|---|---|---|
| Baking soda | ✅ | 1–2 tsp in water, fast “fire put-out” | High sodium, not for frequent use |
| Apple cider vinegar / pickle juice | ✅ | 1 tbsp ACV, or pickle juice swallowed for relief | Counterintuitive, popular and swift |
| Banana / Milk / Lozenges | ✅ | Eat soothing banana or lozenges to aid saliva | Gentle relief, low acidity benefit |
| Swallowing air “burp bubble” | ✅ | Instant blockade of reflux | Mechanical trick, may work for some |
| Carrot / celery / ginger juices | ✅ | Sipping veggie/ginger mix for quick calm | Natural, anti-inflammatory properties |
| Lifestyle adjustments & breathing | ✅ | Bed angle, meal timing, high-pH water, breathing | Key for long-term success |
Your Action Plan for Next Time Heartburn Strikes
- Immediate: Try a glass of water, or ½ tsp baking soda in water. If you’re adventurous, a tablespoon of pickle juice or diluted ACV.
- Soothing: Eat a banana, suck a lozenge, drink a bit of cold milk or oatmilk.
- Longer-acting: Try celery or ginger juice, chew fennel seeds, or sip on cumin water.
- Lifestyle: Don’t lie down! Walk around, prop yourself up, and note what triggered it.
- Prevent: Adopt small meals, stay upright after eating, and keep your spice triggers in check.
When To See a Doctor
If you’re getting heartburn more than twice a week, have trouble swallowing, vomit blood, or have unexplained weight loss—see a doctor ASAP. Chronic heartburn can mean something more serious.
Final Word: Experiment & Listen to Your Body
Everyone’s digestive system is different. The trick is to experiment (one remedy at a time), take notes, and see what works for you. With this toolkit of real-life, natural fixes—and a few small habits—you can keep heartburn in check and get back to enjoying life (and food!) again.
Got your own remedy or story? Share it in the comments—let’s help each other beat the burn, naturally!
References: Healthline, Medical News Today, Reddit, Times of India, UCLA Health, VeryWell Health, EatingWell, Patient.Info community, and real user stories. All advice is for informational purposes—when in doubt, talk to your doctor.
10 Frequently Asked Questions (FAQs) About Natural Heartburn Relief
1. What is the fastest natural remedy for heartburn?
The quickest natural remedy is usually drinking a glass of water or a baking soda solution (½–1 tsp in a glass of water). Both can neutralize acid within minutes. Use baking soda sparingly due to sodium content.
2. Can banana or milk really help with heartburn?
Yes, many people find bananas soothing due to their low acidity and natural antacid effect. Low-fat milk or plant-based alternatives like oat milk can also help, though some people experience rebound acidity with dairy.
3. Is it safe to use baking soda for heartburn often?
No. Baking soda is safe for occasional, emergency use, but frequent use can cause high sodium intake and disrupt your body’s pH balance. Consult your doctor for recurring symptoms.
4. Are there any natural remedies I should avoid?
Avoid peppermint (can worsen reflux), full-fat dairy (may trigger more acid), and excessive vinegar if it worsens symptoms. Always listen to your body and stop any remedy that causes discomfort.
5. How long should I wait before lying down after a meal if I have heartburn?
Wait at least 2–3 hours before lying down. Staying upright helps prevent acid from flowing back into your esophagus.
6. Does apple cider vinegar work for everyone?
No, ACV helps some people (especially if low stomach acid is the cause), but can worsen symptoms for others. Always start with a small, diluted amount to test your tolerance.
7. What are some Indian/ayurvedic remedies for quick relief?
Curd (plain yogurt), coconut water, jeera (cumin) water, fennel seeds (saunf), and bananas are traditional remedies proven helpful by many in India.
8. What lifestyle changes can prevent heartburn naturally?
Eat smaller meals, avoid late-night eating, maintain a healthy weight, avoid trigger foods, elevate your head while sleeping, and reduce stress. Consistency matters more than perfection.
9. When should I see a doctor for heartburn?
If you have heartburn more than twice a week, trouble swallowing, vomiting blood, black stools, or unexplained weight loss, see a doctor immediately. Chronic or severe heartburn needs medical evaluation.
10. Can natural remedies be used with medications?
Generally, yes, but always check with your doctor—especially if using remedies like baking soda, aloe vera, or vinegar. Some can interact with medications or underlying conditions.