1. Introduction
Eyelid dermatitis is a multifaceted skin condition marked by inflammation, redness, and itchiness around the eyes. This prevalent issue can significantly impact daily comfort and appearance, necessitating a comprehensive understanding and a multifaceted approach to management.
2. Unveiling the Types of Eyelid Dermatitis
Understanding the specific type of eyelid dermatitis you are dealing with is crucial for effective management. The condition manifests primarily in three forms:
- Allergic Dermatitis: Caused by an allergic reaction to substances like makeup, pollen, or skincare products. Symptoms include redness, swelling, and itching.
- Atopic Dermatitis (Eczema): A chronic condition often linked to a genetic predisposition. It is characterized by dry, itchy, and inflamed skin.
- Contact Dermatitis: Results from direct skin contact with irritants, leading to symptoms like redness, burning, and itching.
For a more nuanced understanding, refer to: Eczema and Dermatitis: Causes and Coping Mechanisms.
3. Medical Treatments: A Closer Look
Various medical interventions can be employed to manage eyelid dermatitis effectively:
- Topical Creams and Ointments: Products like steroids or calcineurin inhibitors that reduce inflammation and ease symptoms.
- Prescribed Medications: Oral medications or eye drops that a doctor might prescribe in more severe cases.
Explore detailed treatment options here: Exploring Eucrisa: An Eczema Solution.
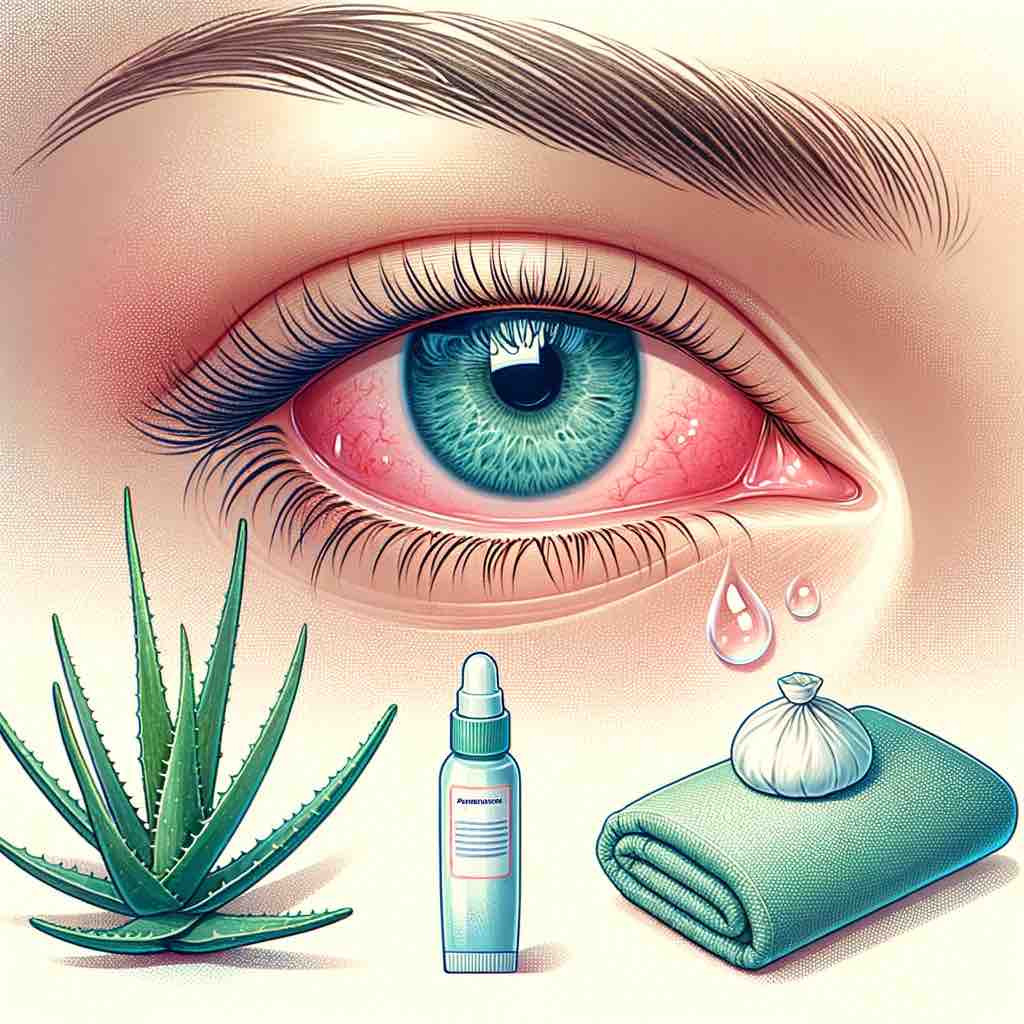
4. Home Remedies and Natural Solutions: Gentle Approaches
Home remedies offer a softer, more natural approach to managing eyelid dermatitis:
- Cold Compresses: To reduce swelling and soothe irritation.
- Aloe Vera: Known for its soothing and anti-inflammatory properties.
- Oatmeal Baths: A gentle way to soothe and moisturize the skin. Learn more: Oatmeal Baths: Remedy for Eczema and Dermatitis.
5. Skincare and Cosmetic Products: Making the Right Choices
Choosing the right skincare and cosmetic products is essential in managing eyelid dermatitis without exacerbating the condition. Here are some considerations:
- Select Hypoallergenic Products: Opt for products specifically formulated for sensitive skin to minimize the risk of irritation.
- Avoid Harsh Chemicals: Steer clear of products containing irritants like alcohol, fragrances, or dyes.
- Moisturize Regularly: Keep the skin hydrated by using gentle, moisturizing creams or ointments.
6. Preventative Strategies and Lifestyle Adjustments
Adopting certain preventative measures and lifestyle changes can help in managing the condition better:
- Identify and Avoid Triggers: Recognize substances or factors that worsen the condition and try to avoid them.
- Maintain a Skin-Friendly Diet: Consume foods that promote skin health and avoid those that may trigger flare-ups. For dietary guidance, refer to: Foods to Embrace and Avoid for Eczema Relief.
- Practice Good Eyelid Hygiene: Keep the eyelid clean and free from irritants as much as possible.
7. Conclusion: Crafting Your Path to Relief
Navigating through eyelid dermatitis involves a journey of exploration and adaptation. Armed with knowledge and a variety of strategies, you can tailor an approach that suits your needs, offering relief and improvement in the condition.
8. Additional Resources for In-depth Exploration
For further insights and a more comprehensive understanding, consider exploring the following resources:
- Healing Eczema Naturally
- Natural Remedies for Eczema Around the Eyes
- Exploring Different Eczema Treatments
FAQs
- What are the common symptoms of eyelid dermatitis? Eyelid dermatitis typically presents with symptoms such as redness, swelling, itching, and flaking of the skin around the eyes. The severity and combination of symptoms can vary based on the individual and the type of dermatitis present.
- Which types of eyelid dermatitis are most prevalent? The most common types of eyelid dermatitis include allergic, atopic, and contact dermatitis. Each type has unique triggers and manifestations, requiring different approaches to management and treatment.
- How can medical treatments benefit eyelid dermatitis? Medical treatments, such as topical creams and ointments, play a crucial role in managing the symptoms of eyelid dermatitis by reducing inflammation, easing discomfort, and promoting healing.
- Are there effective home remedies for managing eyelid dermatitis? Yes, home remedies like cold compresses, aloe vera, and oatmeal baths can offer soothing relief, complementing medical treatments and aiding in the skin’s recovery process.
- What should be considered when choosing skincare and cosmetic products for eyelid dermatitis? It’s essential to select hypoallergenic products, avoid harsh chemicals, and ensure that the products are suitable for sensitive skin to prevent further irritation.
- How can lifestyle adjustments contribute to the management of eyelid dermatitis? Lifestyle adjustments such as identifying and avoiding triggers, maintaining a skin-friendly diet, and practicing good eyelid hygiene can significantly impact the management of eyelid dermatitis.
- What role does diet play in managing eyelid dermatitis? A well-balanced diet that supports skin health can be beneficial. Identifying and avoiding foods that may trigger or worsen the condition is also crucial.
- Is it possible to prevent eyelid dermatitis flare-ups? While it may not be entirely preventable, recognizing and avoiding triggers, along with consistent skincare practices, can help reduce the frequency and severity of flare-ups.
- Where can I find more detailed information and guidance on eyelid dermatitis? Various resources offer in-depth insights, practical tips, and expert advice on managing eyelid dermatitis, such as specialized articles, blogs, and medical websites.
- What are some recommended resources for further reading on eyelid dermatitis? Consider exploring articles that delve into different aspects of eyelid dermatitis, such as causes, treatments, home remedies, and preventative strategies, for a comprehensive understanding.
Blog Tags
eyelid dermatitis, eczema, skincare, home remedies, medical treatments, allergic dermatitis, atopic dermatitis, contact dermatitis, eyelid care, natural remedies













