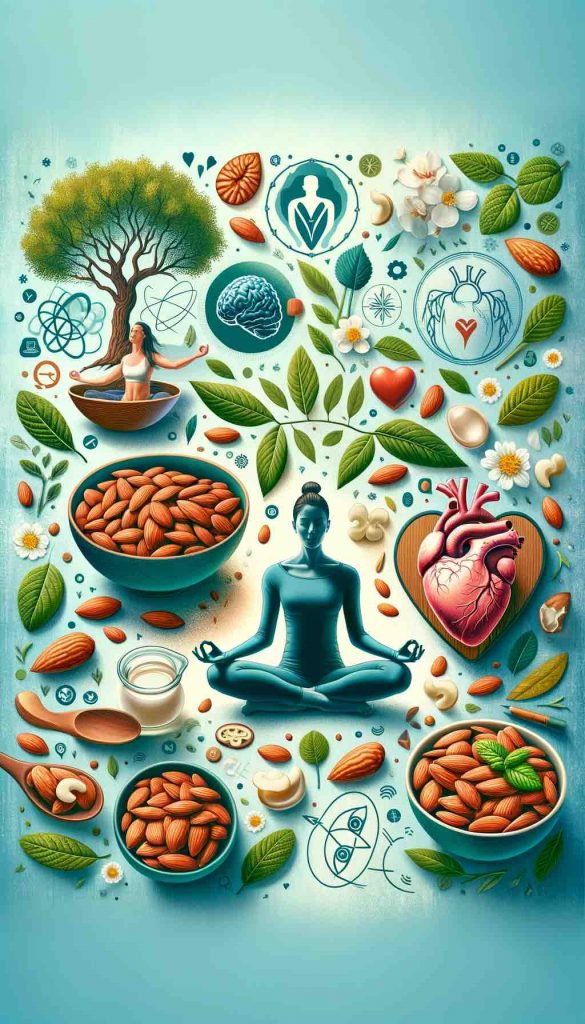
Almonds are more than just a snack—they’re a daily health booster when prepared the right way. One of the oldest wellness traditions, especially in Ayurveda, is soaking almonds overnight and consuming them first thing in the morning. But why go through the trouble of soaking them? Turns out, the benefits are well worth the effort. Here’s a deep dive into the top ten benefits of eating soaked almonds daily, and why this simple habit can make a big difference.
1. Enhanced Digestion and Nutrient Absorption Soaking almonds removes their brown skin, which contains tannins that inhibit nutrient absorption. The soaking process also reduces phytic acid, a compound that binds minerals and prevents the body from absorbing them efficiently. The result? Your body gets more out of every almond—especially key nutrients like magnesium, iron, and calcium.
2. Activated Enzymes for Metabolism Support When almonds are soaked, they begin to sprout slightly, initiating the activation of beneficial enzymes. These enzymes, such as lipase, aid in the breakdown of fats and improve metabolic function. This means your body can better process what you eat throughout the day, keeping you energized and balanced.
3. Heart Health and Cholesterol Control Soaked almonds are rich in monounsaturated fats and antioxidants, particularly vitamin E. These nutrients are essential for cardiovascular health, helping to lower LDL (bad cholesterol) and increase HDL (good cholesterol). Magnesium in almonds also helps regulate blood pressure, further protecting your heart.
4. Natural Energy Booster Forget sugary energy drinks. Soaked almonds offer a natural boost thanks to their balanced mix of protein, fiber, healthy fats, and B vitamins like riboflavin. This combination stabilizes blood sugar and provides sustained energy without the crash.
5. Aiding in Weight Management Despite being calorie-dense, almonds can actually help with weight management. Their fiber and protein content increase satiety, reducing the urge to snack unnecessarily. Soaked almonds are also easier to digest, reducing bloating and helping you feel lighter throughout the day.
6. Brain Health and Cognitive Function Almonds are often called “brain food” for good reason. They contain nutrients like riboflavin and L-carnitine that are linked to neurological function. Regular consumption supports better memory, sharper focus, and may even reduce the risk of age-related cognitive decline.
7. Glowing Skin from Within The vitamin E and antioxidants in soaked almonds help combat oxidative stress, one of the main contributors to aging skin. These nutrients also support hydration and skin elasticity, giving you a healthy glow naturally.
8. Stronger, Healthier Hair Biotin (vitamin B7), magnesium, and proteins in almonds nourish hair follicles, promote growth, and reduce hair thinning. Soaked almonds are also easier to digest, which means these nutrients are absorbed more efficiently, translating to shinier, stronger hair over time.
9. Better Blood Sugar Regulation Almonds have a low glycemic index and are rich in fiber, healthy fats, and magnesium—all of which play a role in stabilizing blood sugar levels. Eating soaked almonds regularly can help prevent sugar spikes and improve insulin sensitivity, making them particularly beneficial for people with or at risk of type 2 diabetes.
10. Bone Strength and Immune Support Calcium, magnesium, phosphorus, and zinc in almonds are vital for maintaining strong bones and a resilient immune system. Regular intake of soaked almonds can help you meet your daily mineral requirements and reduce your risk of deficiencies.
How to Soak Almonds Properly It’s simple: Take 5-10 raw almonds and soak them in a glass of water overnight (8-12 hours). In the morning, peel off the skin and eat them on an empty stomach. This enhances their digestibility and nutritional value.
Final Thoughts Soaked almonds pack a nutritional punch in a small, digestible form. By soaking and peeling them, you unlock their full potential and give your body access to a wider range of benefits—from heart health to better digestion to glowing skin. It’s a habit that takes less than a minute to start but pays dividends for a lifetime.
If you’re looking to make one small change that has a big impact, start soaking your almonds tonight. Your body will thank you in the morning.
Quick Recap – Health Gains at a Glance
| Benefit | Key Impact |
|---|---|
| Digestion | Enzyme activation, less bloating |
| Heart health | Cholesterol ↓, blood pressure ↓ |
| Energy | Sustained fuel, low crash |
| Weight | Appetite control |
| Brain | Memory, focus |
| Skin & Hair | Hydration, protection |
| Metabolism | Blood sugar control |
| Bones & Immunity | Minerals support |
FAQs
1. Why should I soak almonds instead of eating them raw?
Soaking removes enzyme inhibitors like tannins and phytic acid, making the almonds easier to digest and increasing nutrient absorption.
2. How long should I soak almonds?
Ideally, soak them for 8 to 12 hours overnight in clean water.
3. Should I peel soaked almonds before eating?
Yes. Peeling removes the skin that contains tannins, which can interfere with nutrient absorption.
4. How many soaked almonds should I eat per day?
5 to 10 soaked almonds per day is a healthy amount for most adults.
5. Can I soak almonds in hot water to speed up the process?
Yes, soaking in hot water for about an hour works in a pinch, but overnight soaking in room-temperature water is best for full enzyme activation.
6. Is there a best time to eat soaked almonds?
Yes, the best time is first thing in the morning on an empty stomach to maximize absorption and energy benefits.
7. Can soaked almonds help with weight loss?
Yes. They’re rich in fiber and protein, which promote satiety and help control cravings.
8. Are soaked almonds safe for diabetics?
Absolutely. They help regulate blood sugar levels and improve insulin sensitivity.
9. Can children eat soaked almonds?
Yes, but give them in moderation and ensure they’re peeled and soft to avoid choking.
10. Do soaked almonds lose any nutrients compared to raw ones?
No—they become easier to digest and absorb, actually enhancing the nutritional benefit.