Pregnancy is a beautiful journey—but let’s be honest, it can also leave you feeling exhausted, especially if your iron levels take a dip. Iron is the mineral that keeps your blood oxygenated and your energy steady, and during pregnancy your body needs almost 50% more of it—jumping from 18 mg/day to a whopping 27 mg/day.
If you’re following a plant-based lifestyle, you might already know that your iron comes in the “non-heme” form, which isn’t absorbed quite as efficiently as the “heme” iron from animal products. But don’t worry—research in 2025 has shown that with smart food pairings, preparation methods, and a little creativity in the kitchen, plant-based diets can fully support a healthy pregnancy.
And here’s where two humble heroes—lentils and spinach—come into play.
Why Iron Matters So Much During Pregnancy
During pregnancy, your blood volume increases by about 50%, which means your body is working double-time to carry oxygen to both you and your growing baby. That requires more hemoglobin—and hemoglobin is built from iron.
Daily iron needs:
- Before pregnancy: ~18 mg/day
- During pregnancy: ~27 mg/day
Low iron can lead to anemia, which may cause fatigue, dizziness, shortness of breath, and even affect your baby’s growth. Research from 2025 confirms that well-planned plant-based diets can meet these increased needs—especially when you pay attention to iron absorption.
Why Lentils + Spinach Are a Perfect Pair
- Lentils: ~6–7 mg of iron per cooked cup, plus high folate content for fetal brain and spine development, fiber for digestion, and plant protein.
- Spinach: ~6.4 mg of iron per cooked cup, along with vitamins A, K, and a touch of vitamin C.
- Vitamin C synergy: Combining these with vitamin C-rich foods (bell peppers, lemon juice, tomatoes) can dramatically improve iron absorption.
💡 Pro tip: Cooking in a cast-iron pan can naturally increase the iron content of your meals—a method validated by recent UC Davis nutrition research.
The Science of Absorption (Made Simple)
Iron from plants (non-heme iron) isn’t absorbed as efficiently as iron from meat (heme iron). But there are easy ways to change that:
✅ Do
- Pair with vitamin C sources to boost absorption.
- Soak, sprout, or ferment lentils to reduce phytates (iron blockers).
- Cook in cast-iron cookware.
❌ Don’t
- Drink tea or coffee with iron-rich meals (tannins can block absorption by up to 60%).
- Rely solely on spinach without pairing with other absorption-friendly foods.
5 Delicious Lentil + Spinach Snacks for Pregnancy
Pregnancy snacks don’t have to be bland or repetitive. With lentils and spinach as the foundation, you can create snacks that are not only rich in iron, folate, and fiber, but also bursting with flavor and texture. Here’s a detailed look at five tried-and-true recipes, with extra tips for enhancing absorption, making them in bulk, and adding variety.
1. Spinach & Lentil Patties
Why they work:
These patties deliver iron, protein, and folate in a compact, freezer-friendly form. They’re satisfying enough for a midday hunger pang and versatile enough to double as a burger patty for dinner.
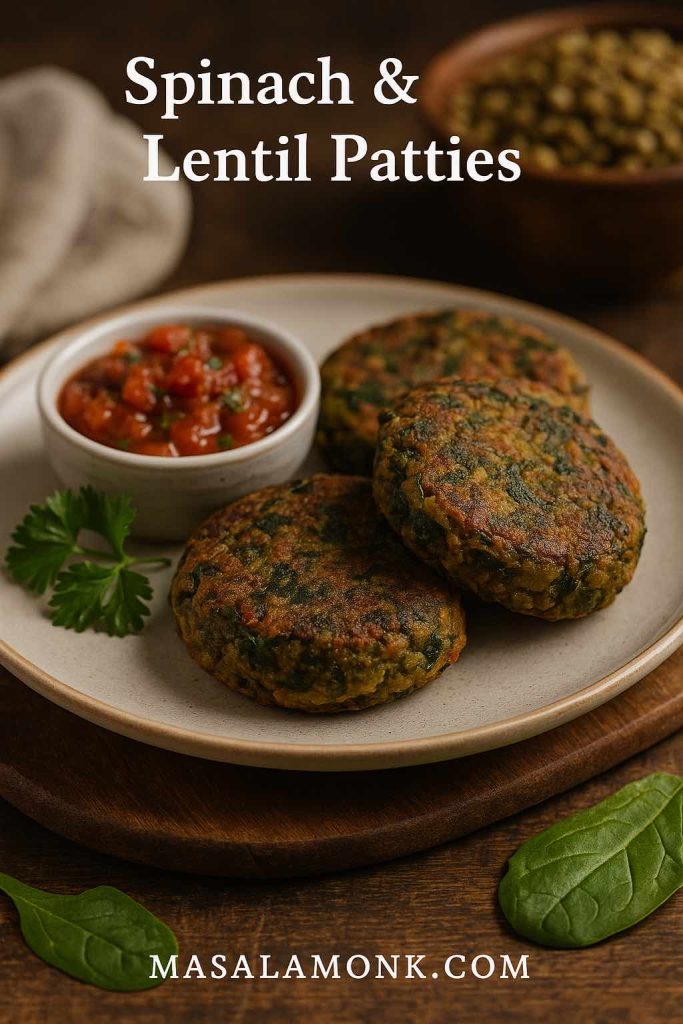
Ingredients:
- 1 cup cooked brown or green lentils (soaked overnight for better digestion)
- 2 cups fresh spinach leaves, finely chopped
- ½ cup breadcrumbs or oat flour
- 1 small onion, finely diced
- 2 cloves garlic, minced
- 1 tsp ground cumin
- Juice of ½ lemon (vitamin C boost)
- Salt & pepper to taste
- 2 tbsp olive oil for pan-searing
Method:
- Prep the lentils: Boil soaked lentils until tender but not mushy. Drain well to prevent soggy patties.
- Cook the spinach: Sauté with onion and garlic until just wilted.
- Mix: Combine lentils, spinach mixture, breadcrumbs, spices, and lemon juice. Mash lightly, leaving some lentil texture.
- Shape: Form into small patties.
- Cook: Pan-sear in a cast-iron skillet until golden on each side.
💡 Related: Boosting Folate in Pregnancy: Top 5 Lentil and Bean Dishes
Pregnancy Tip: Pair with fresh tomato salsa or bell pepper chutney to increase non-heme iron absorption.
Make-Ahead: Freeze uncooked patties between parchment sheets. Cook straight from frozen, adding 2–3 extra minutes per side.
2. Lentil & Spinach Hummus
Why they work:
A smooth, creamy dip that sneaks in greens without compromising flavor. Perfect for an afternoon snack that also helps you meet your protein quota.
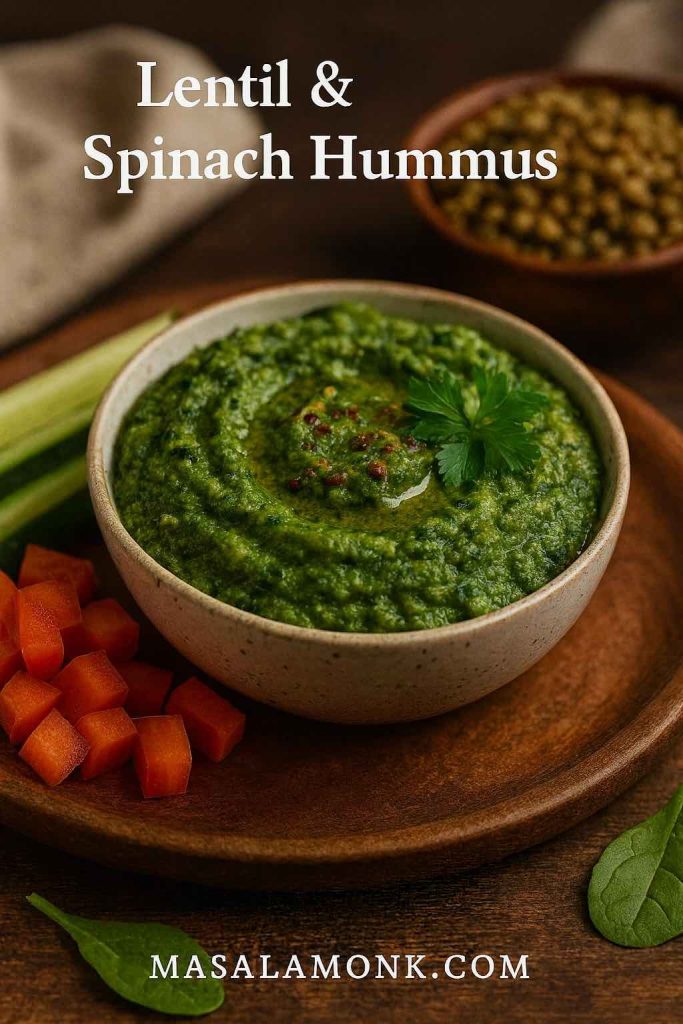
Ingredients:
- 1 cup red lentils, boiled until soft
- 1 cup spinach, blanched for 30 seconds
- 2 tbsp tahini (calcium + healthy fats)
- 2 tbsp lemon juice (vitamin C)
- 1 garlic clove, roasted or raw
- 1 tbsp olive oil
- Salt & cumin to taste
Method:
- Cook lentils: Boil until soft, drain well.
- Blanch spinach: Drop into boiling water for 30 seconds, then shock in ice water to keep it green.
- Blend: Add lentils, spinach, tahini, lemon juice, garlic, olive oil, salt, and cumin to a food processor. Blend until creamy.
Serving Tip: Serve with carrot sticks, cucumber rounds, or bell pepper strips.
💡 Related: 5 Sugarless Snacks Rich in Iron for Pregnant Nights
Pregnancy Tip: Red lentils cook quickly and are easy to digest—ideal for pregnancy when digestion can slow down.
Flavor Variations: Add roasted red peppers or sun-dried tomatoes for a smoky twist.
3. Mini Spinach-Lentil Soup Shots
Why they work:
These are perfect when you want something warm and nourishing without committing to a full bowl. Great as a mid-morning boost or evening wind-down.

Ingredients:
- ½ cup red or yellow lentils
- 2 cups vegetable broth (low sodium)
- 1 cup chopped spinach
- 1 medium tomato, diced (vitamin C)
- ½ onion, chopped
- 1 garlic clove, minced
- ½ tsp turmeric
- Salt & pepper to taste
- Lemon wedges to serve
Method:
- Cook lentils: Simmer in vegetable broth with onion, garlic, tomato, and turmeric until soft.
- Add spinach: Stir in chopped spinach just before blending.
- Blend: Puree until silky smooth.
- Serve: Pour into small mugs or shot glasses, garnish with lemon.
💡 Related: 5 Folate-Focused Recipes for a Nourishing Pregnancy
Pregnancy Tip: Turmeric adds anti-inflammatory benefits, but keep portions moderate (¼–½ tsp) during pregnancy.
Make-Ahead: Freeze in small glass jars; thaw overnight for a ready-to-go warm snack.
4. Lentil & Spinach Falafel Wraps
Why they work:
These wraps are a complete mini-meal in one — protein-packed falafels made with lentils and spinach, wrapped with crisp vegetables and a creamy dressing. Perfect for a quick lunch or a portable pregnancy-friendly snack.
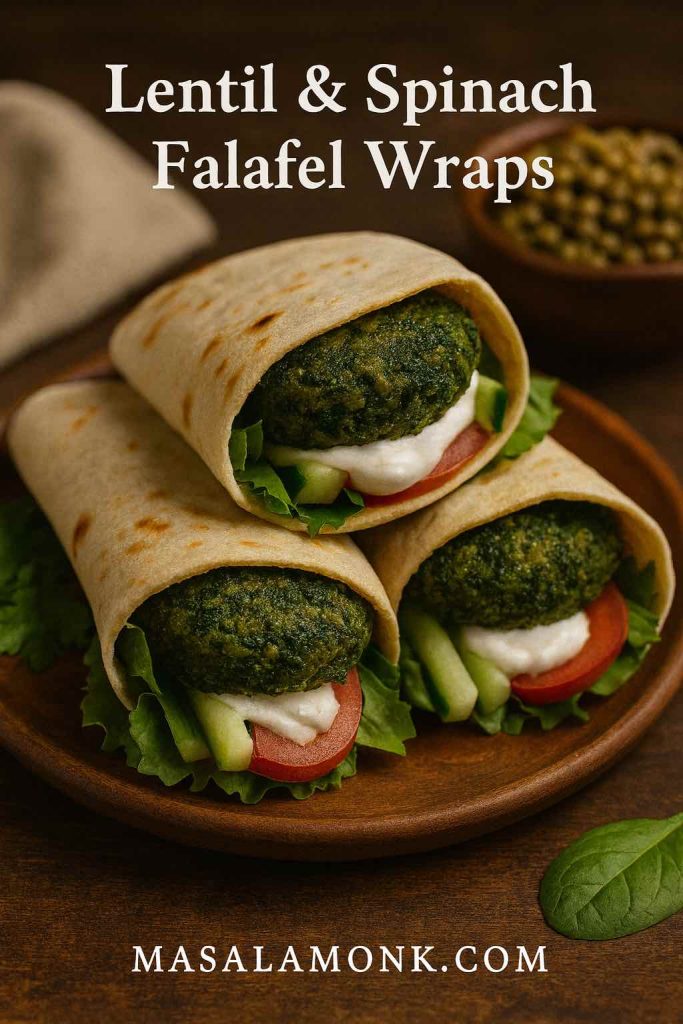
Ingredients:
- 1 cup green lentils, cooked and drained
- 1½ cups spinach, finely chopped
- ¼ cup chickpea flour (binds and boosts protein)
- 2 cloves garlic, minced
- 1 tsp cumin powder
- ½ tsp coriander powder
- Salt & pepper to taste
- 4 whole wheat pitas or wraps
- Salad fillings: lettuce, tomato slices, cucumber sticks
- Tahini or yogurt dressing
- Lemon wedges
Method:
- Mix: In a food processor, blend lentils, spinach, garlic, chickpea flour, and spices into a coarse mixture.
- Shape: Form into small patties or balls.
- Cook: Bake at 200°C (390°F) for 20 minutes or pan-fry with minimal oil until golden.
- Assemble: Place falafels in pitas with salad fillings and drizzle generously with tahini or yogurt dressing. Squeeze lemon juice over before serving.
💡 Related: 10 Exotic Superfoods for a Healthy Pregnancy
Pregnancy Tip: Add sliced avocado for healthy fats and extra creaminess.
Batch Tip: Prepare falafel mixture in advance and refrigerate for up to 2 days, or freeze shaped falafels to cook later.
5. Spinach-Lentil Energy Wraps
Why they work:
Fresh, crunchy, and portable—these wraps require minimal prep and can be customized for different cravings.

Ingredients:
- Large spinach leaves or whole-grain tortillas
- 1 cup cooked brown lentils
- ½ cup shredded carrots
- ½ cup thinly sliced bell peppers (vitamin C)
- ¼ avocado, sliced (healthy fats)
- 2 tbsp tahini-lemon dressing
Method:
- Prep filling: Mix lentils with carrots, bell peppers, and avocado.
- Assemble: Lay spinach leaves or tortillas flat, fill with lentil mixture.
- Dress: Drizzle with tahini-lemon dressing.
- Wrap & secure: Roll tightly and secure with a toothpick if needed.
💡 Related: 5 Omega-3 Rich Vegan Snack Ideas for Pregnant Women
Pregnancy Tip: These wraps are rich in fiber and healthy fats, helping to maintain steady blood sugar levels.
Make-Ahead: Pack in parchment for a quick grab-and-go snack; store in the fridge for up to 24 hours.
🥗 Final Pro Tips for All 5 Recipes
- Enhance absorption: Always pair with a vitamin C source.
- Diversify your greens: Swap spinach with kale or amaranth leaves for variety.
- Play with spices: Pregnancy-safe spices like cumin, coriander, and fennel add flavor and aid digestion.
- Mind your portions: Multiple smaller snacks can be easier on digestion than one large portion during pregnancy.
Pregnancy Nutrition Tip
Even with the best snack lineup, iron deficiency can still sneak up during pregnancy. Pay attention to symptoms like unusual fatigue, dizziness, or shortness of breath—and don’t skip your prenatal checkups. If your doctor recommends a supplement, it’s not a failure—it’s just an extra tool in your pregnancy wellness kit.
Final Thoughts
Pregnancy nutrition can feel overwhelming, but it doesn’t have to be complicated. By combining the humble lentil with vibrant spinach—and pairing them with vitamin C—you can create snacks that are as delicious as they are nourishing.
Think of these recipes as a starting point. Once you get the hang of the flavor combos, you’ll find endless variations. And by linking your snacks to other nutrient-packed recipes—like Folate-Focused Recipes or Omega-3 Rich Vegan Snack Ideas—you can build a pregnancy-friendly menu that keeps you energized and your baby thriving.
So go ahead—grab those lentils and spinach. Your body (and your baby) will thank you.
FAQs – Lentil & Spinach Pregnancy Snacks
1. Why are lentils and spinach recommended during pregnancy?
Lentils and spinach are both rich in iron, folate, and fiber—three nutrients vital for pregnancy. Iron supports healthy blood oxygen levels, folate aids fetal brain and spinal development, and fiber helps prevent constipation, which is common during pregnancy.
2. How much iron do I need daily while pregnant?
Most pregnant women need about 27 mg of iron per day, compared to 18 mg before pregnancy. Since plant-based iron (non-heme iron) is absorbed less efficiently, it’s important to pair it with vitamin C-rich foods like bell peppers, tomatoes, or lemon juice.
3. Can I meet my iron needs on a plant-based diet during pregnancy?
Yes. Research in 2025 confirms that with smart food pairings, soaking or sprouting legumes, and cooking methods like using cast-iron pans, plant-based diets can fully support healthy pregnancy iron levels.
4. Why should I pair lentils and spinach with vitamin C?
Vitamin C helps convert plant-based iron into a form your body can absorb more easily. Adding lemon juice, fresh tomatoes, or bell peppers to your lentil and spinach dishes can significantly boost iron uptake.
5. Can I freeze these snacks for later?
Absolutely. Most of these recipes—especially patties, cutlets, and falafel—can be frozen uncooked between parchment sheets or cooked and cooled before freezing. This makes healthy snacking quick and convenient.
6. Are these recipes safe for gestational diabetes?
Yes, with some adjustments. These snacks are high in fiber and protein, which help stabilize blood sugar. If needed, reduce or avoid added refined carbs (like breadcrumbs) and use oat or chickpea flour instead.
7. Can I substitute spinach with other greens?
Yes. Kale, Swiss chard, and amaranth leaves are excellent alternatives, offering similar nutrient profiles and slightly different flavors. Just adjust cooking times, as tougher greens may need a bit longer to soften.
8. Do lentils need to be soaked before cooking?
Soaking lentils isn’t strictly necessary, but it can reduce cooking time and help lower phytates—natural compounds that can reduce iron absorption. For better digestion during pregnancy, soaking is recommended.
9. Can I make these snacks gluten-free?
Yes. Replace breadcrumbs with oat flour, chickpea flour, or ground flaxseeds. All five recipes can be adapted to be 100% gluten-free without losing flavor or texture.
10. Are there any foods I should avoid pairing with these snacks?
Avoid consuming tea, coffee, or high-calcium dairy products at the same time as iron-rich meals, as tannins and calcium can block iron absorption. Instead, enjoy those beverages between meals.