When you think of a healthy snack, apples often come to mind. With their juicy, crisp texture, apples have long been a favorite fruit worldwide, not just for their taste but also for their health benefits. But if you are someone managing diabetes, you might find yourself wondering, “Can I still enjoy this crunchy fruit?” The good news is that apples can absolutely be part of a diabetes-friendly diet, provided you understand their nutritional impact and how to include them mindfully in your meals.
This blog post dives deep into answering five key questions about apples and diabetes, followed by five delicious and creative ways you can enjoy apples while keeping your blood sugar levels in check. Let’s start with the essentials!
5 Important Questions About Apples and Diabetes
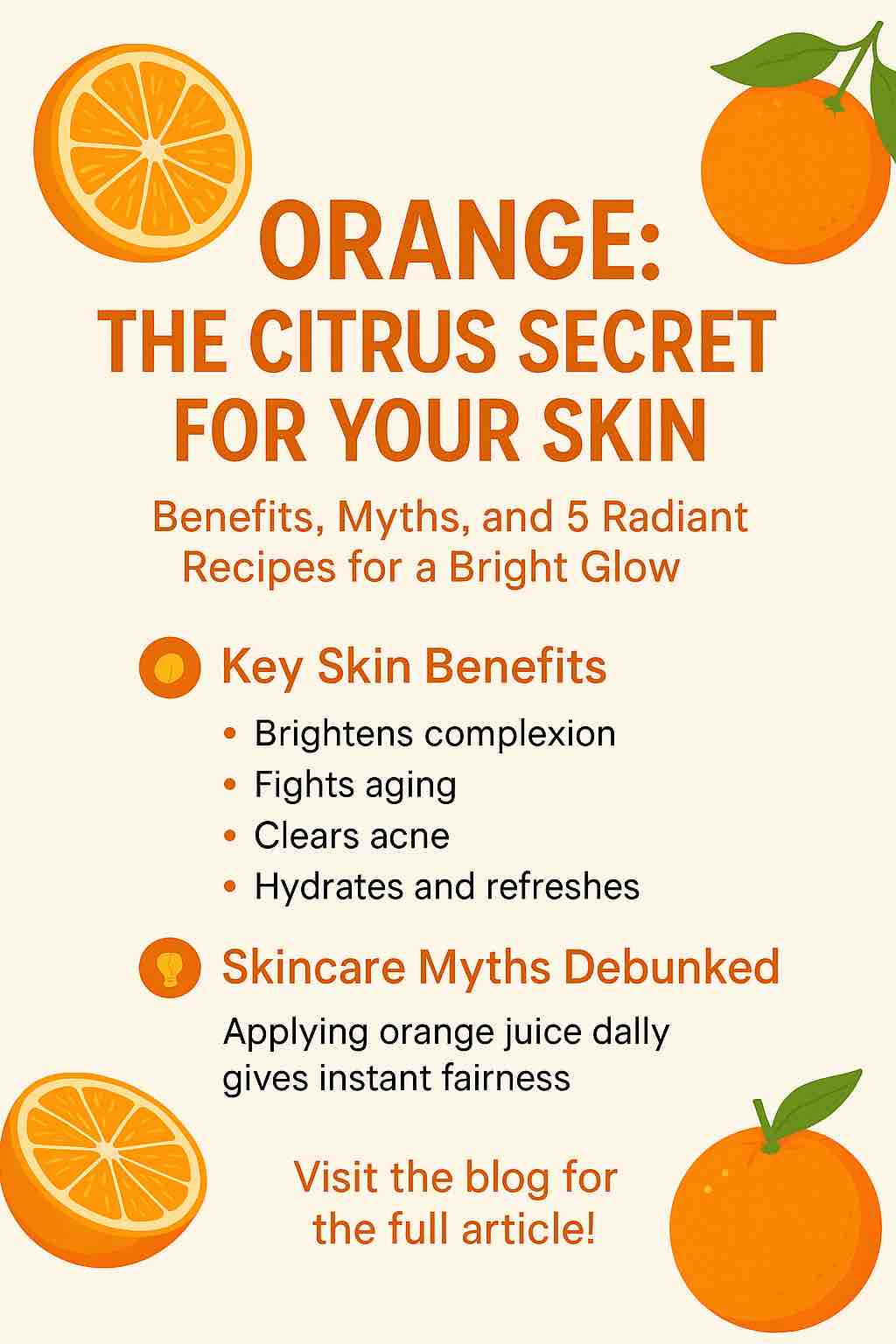
1. Are Apples Safe for Diabetics?
Apples are not only safe but also beneficial for individuals with diabetes, when consumed in moderation. One medium-sized apple contains approximately 20-25 grams of carbohydrates, primarily from natural sugars. However, this doesn’t mean that apples should be avoided; in fact, they are a great option for diabetics because they come with a wealth of health benefits.
First and foremost, apples are rich in fiber, particularly soluble fiber, such as pectin. This fiber plays an essential role in regulating blood sugar levels by slowing down the digestion and absorption of sugar into the bloodstream. This slow release helps prevent blood sugar spikes after meals, which is crucial for diabetics trying to manage their condition.
Additionally, apples contain antioxidants, particularly flavonoids and polyphenols, which have been shown to reduce oxidative stress in the body. Oxidative stress is a key factor in the development of diabetic complications such as nerve damage, heart disease, and kidney issues. Therefore, consuming apples regularly can help promote overall health.
2. Do Apples Raise Blood Sugar Levels?
The glycemic index (GI) of a food measures how quickly it raises blood sugar after consumption. Foods with a high GI value can cause a rapid spike in blood sugar levels, while foods with a low GI value release glucose more gradually. Apples have a relatively low glycemic index of about 38, meaning they have a minimal effect on blood sugar levels.
However, while apples are low in GI, portion control is essential. A large apple, for instance, may contain more carbohydrates than a smaller one. Consuming an entire large apple might lead to a higher blood sugar rise than a small apple. The key to including apples in a diabetic diet is moderation, as well as balancing the apple with other foods that stabilize blood sugar.
3. What is the Best Type of Apple for Diabetics?
Not all apples are created equal when it comes to blood sugar control. Some apple varieties are sweeter than others, and those with a higher sugar content can cause a faster spike in blood glucose levels. If you’re looking for the best apple for diabetes, green apples, particularly Granny Smith apples, are an excellent choice.
Granny Smith apples are not only tart and low in sugar but are also packed with fiber, which helps in blood sugar regulation. They also contain fewer carbohydrates compared to sweeter varieties like Fuji or Red Delicious. While sweeter apples can still be consumed in moderation, opting for a green apple may offer more control over blood sugar levels.
4. How Many Apples Can a Diabetic Eat Per Day?
As with all fruits, portion control is essential. The general guideline for diabetics is to consume a small-to-medium-sized apple (about 150 grams) per day. This amount typically provides 20-25 grams of carbohydrates, which can fit within the daily carb limit for most people with diabetes.
It’s important to consider your overall carbohydrate intake, so if you’re consuming an apple as part of a meal or snack, balance it with protein, healthy fats, and fiber-rich vegetables to prevent a blood sugar spike. For example, pairing an apple with a handful of nuts or a slice of cheese can provide a more balanced snack.
5. Are There Any Benefits to Apples for Diabetics?
Yes! Apples offer numerous health benefits that make them an excellent choice for diabetics. They are rich in antioxidants, particularly flavonoids, which are known for their anti-inflammatory and anti-oxidative properties. These antioxidants help protect the body from damage caused by free radicals, a major factor in the development of diabetes-related complications, such as heart disease and kidney failure.
Additionally, apples are high in soluble fiber, which not only helps regulate blood sugar but also promotes digestive health. The fiber in apples helps slow digestion and prevents rapid spikes in blood glucose after meals. Apples are also linked to better weight management, which is especially important for diabetics, as maintaining a healthy weight can improve insulin sensitivity.
5 Scrumptious Ways to Include Apples in Your Diabetic Diet
Incorporating apples into your diabetic-friendly diet doesn’t have to be boring or bland. Here are five creative and scrumptious ways to enjoy apples while keeping your blood sugar levels under control:
1. Apple and Nut Salad
This crisp, refreshing salad combines the tartness of apples with the crunchy texture of nuts, offering a perfect balance of flavors and textures. Slice a green apple (like Granny Smith) and toss it with mixed greens, such as spinach or arugula. Add a handful of walnuts, almonds, or pistachios for a dose of healthy fats and protein.
Top it off with a light dressing made from olive oil, lemon juice, and a pinch of salt. The nuts provide protein and healthy fats, which help slow the absorption of sugars from the apples, making this salad an excellent choice for a balanced meal.
2. Baked Cinnamon Apples
Baked apples are a warming and comforting treat, especially when the weather turns chilly. Slice up a green apple and sprinkle with cinnamon—a spice that has been shown to improve insulin sensitivity. Cinnamon adds flavor without adding sugar, making it a perfect complement to the natural sweetness of apples.
For a diabetes-friendly twist, bake the apples with a drizzle of stevia or monk fruit sweetener instead of sugar. You can also top them with a dollop of Greek yogurt or a sprinkle of chopped nuts for added protein and healthy fats.
3. Apple and Cheese Snack
If you’re looking for a quick, satisfying snack, try pairing apple slices with a small portion of cheese. The natural sweetness of the apple and the creamy, salty cheese create a delicious contrast. Choose a low-fat cheese like mozzarella, cheddar, or goat cheese to keep the snack healthier.
The combination of apple and cheese provides a good balance of carbohydrates, fiber, protein, and fat, which can help prevent blood sugar spikes and keep you feeling full for longer.
4. Apple Smoothie
A refreshing and nutrient-packed smoothie is a great way to incorporate apples into your diet. For a diabetic-friendly apple smoothie, blend up one small apple with a handful of spinach, a tablespoon of chia seeds, and unsweetened almond milk.
You can also add a scoop of protein powder for an extra boost. This smoothie is packed with fiber, healthy fats, and protein, which will help keep your blood sugar stable throughout the day. Plus, it’s a great way to get in some extra vegetables and antioxidants.
5. Apple Chia Pudding
For a fun, nutritious dessert, try making apple chia pudding. Mix chia seeds with unsweetened almond milk and let them sit overnight to form a thick, pudding-like consistency. In the morning, top the chia pudding with diced apple slices, a sprinkle of cinnamon, and some chopped nuts for added texture.
Chia seeds are a great source of fiber, protein, and omega-3 fatty acids, making them a perfect complement to the apples. This dessert is satisfying, filling, and perfectly suited for a diabetes-friendly diet.
Conclusion
Apples are a delightful and nutritious fruit that can easily fit into a diabetic diet when enjoyed in moderation. By choosing the right variety, controlling portion sizes, and pairing them with other healthy foods, you can savor apples without worrying about blood sugar spikes.
The 5 creative recipes outlined above offer delicious ways to include apples in your daily meals, allowing you to enjoy the many benefits this crunchy fruit has to offer. So go ahead, take a bite into that crisp apple—your taste buds and your body will thank you!
FAQs About Apples and Diabetes
1. Can diabetics eat apples daily?
Yes, diabetics can enjoy an apple a day in moderation. A medium-sized apple typically contains around 20-25 grams of carbohydrates, so it’s important to factor it into your daily carbohydrate intake. Pairing it with protein or healthy fats helps balance blood sugar levels.
2. Are apples high in sugar?
Apples contain natural sugars, but they also have a low glycemic index (GI), which means they do not cause a rapid increase in blood sugar levels. Their fiber content, particularly soluble fiber, helps slow the absorption of sugar, making them a good choice for diabetics.
3. What is the glycemic index of apples?
Apples have a glycemic index of around 38, which is considered low. Foods with a low GI are absorbed slowly, preventing spikes in blood sugar. This makes apples a safe option for individuals with diabetes when consumed in appropriate portions.
4. Is it better to eat apples with or without the skin for diabetics?
It’s better to eat apples with the skin on. The skin is rich in fiber, which helps regulate blood sugar and improve digestion. It also contains antioxidants that can reduce the risk of diabetes-related complications.
5. Can apples be part of a low-carb diet for diabetics?
Apples contain carbohydrates, so they should be consumed in moderation on a low-carb diet. A small apple is usually considered acceptable, but it’s essential to keep track of your overall carbohydrate intake and adjust accordingly.
6. Are green apples better for diabetics than red apples?
Green apples, such as Granny Smith, are often a better choice for diabetics due to their lower sugar content and higher fiber. However, red apples like Fuji and Gala can still be enjoyed in moderation. Opting for tart varieties helps minimize blood sugar spikes.
7. How do apples help control blood sugar levels?
Apples contain soluble fiber, which slows down digestion and the absorption of sugar into the bloodstream. This helps prevent sharp increases in blood sugar levels. Additionally, the antioxidants in apples may improve insulin sensitivity.
8. Can apple juice be consumed by diabetics?
While fresh apple juice may seem like a healthy option, it is not recommended for diabetics because it lacks fiber and can cause a rapid rise in blood sugar. Whole apples, with their skin and fiber, are a much better choice.
9. Are apples a good source of vitamins for diabetics?
Yes, apples are a good source of vitamins, particularly vitamin C, which supports immune function and overall health. They also contain small amounts of other essential vitamins and minerals that contribute to overall well-being.
10. Can apples help with weight management for diabetics?
Yes, apples are a great option for weight management. Their high fiber content promotes satiety, helping you feel fuller for longer. They are also low in calories, making them a great snack for diabetics who are trying to manage their weight.