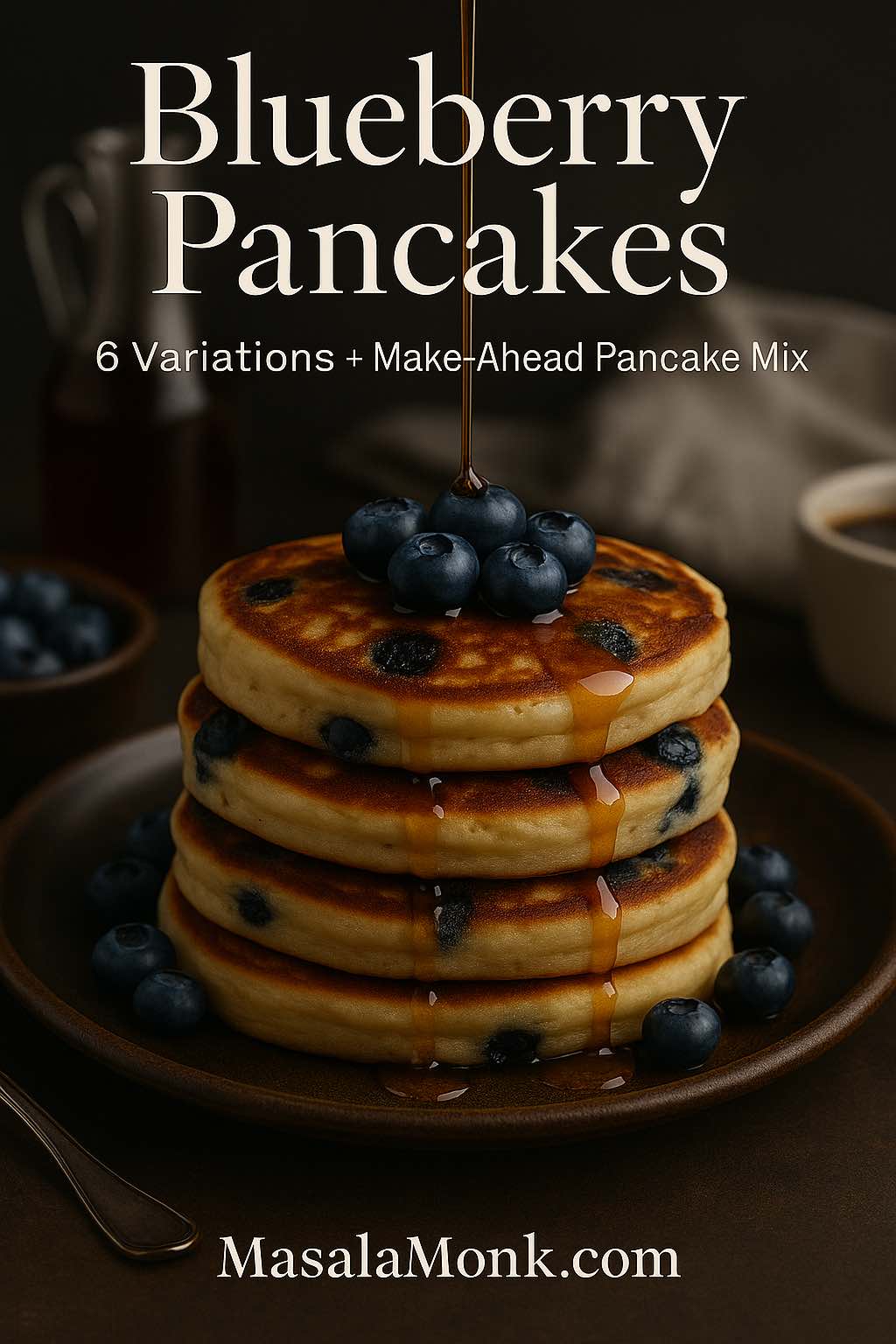
Some mornings call for something simple. Others practically demand a warm stack, a pat of butter sliding into the edges, and that first bite where the blueberries burst and the pancake stays airy instead of heavy. That’s the promise here: blueberry pancakes that taste like blueberries, not like flour with a few berries sprinkled in out of obligation.
To get there, we’ll start with a dependable classic—your “best blueberry pancake” base—then move through the variations people actually look for: blueberry hotcakes, banana and blueberry pancakes, blueberry lemon pancake, blueberry ricotta hotcakes, blueberry oat pancakes (and blueberry oatmeal pancake), plus high protein blueberry pancakes that still taste like breakfast. Along the way, you’ll get a practical approach for frozen blueberries for pancakes, a homemade blueberry pancake mix you can stash for fast mornings, and an easy way to make blueberry pancakes with pancake mix taste like you made them from scratch.
If you’re the type who loves building a whole breakfast scene, there are plenty of natural pairings too: crisp bacon, cozy hot chocolate, café-style coffee, or even a bright smoothie. We’ll get to those at the end—without turning breakfast into a project.
Blueberry Pancakes That Stay Fluffy: A Simple Recipe That Works Every Time
Blueberry pancakes become reliably fluffy for a handful of reasons, and once you understand them, you can switch flavours, add protein, go gluten-free, or use frozen berries—without losing the texture you came for.
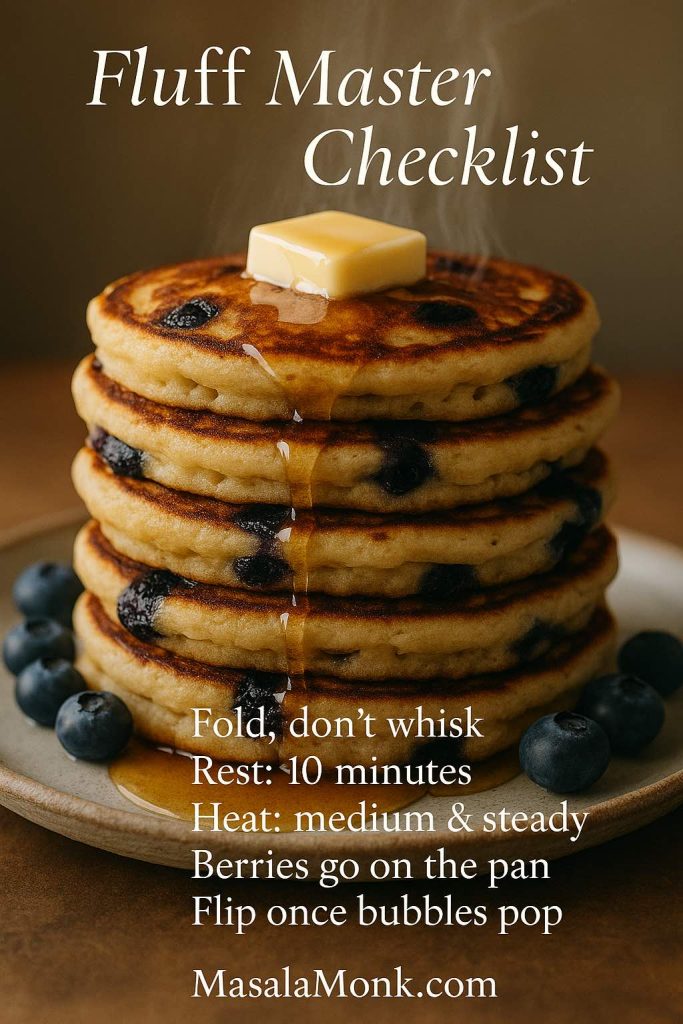
First, keep the batter gentle
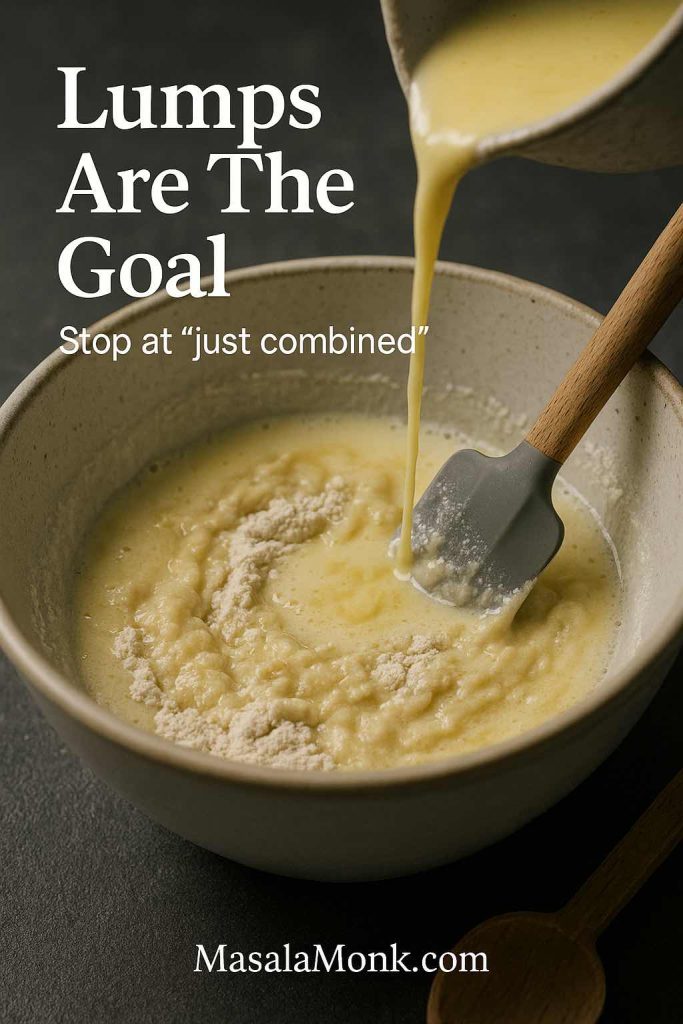
Pancakes want a light touch. As soon as flour meets liquid, gluten starts developing. Stir vigorously and the batter tightens; cook that batter and you’ll get dense pancakes that feel more like bread. Instead, fold until the dry flour disappears and stop. Even if you see a few lumps, leave them alone. They relax as the batter rests.
If you like seeing the logic behind the “don’t overmix” rule, King Arthur’s pancake guidance is consistently practical and clear: Simply Perfect Pancakes. Epicurious also explains why mixing matters in a way that’s easy to remember: why overmixing matters in baking.
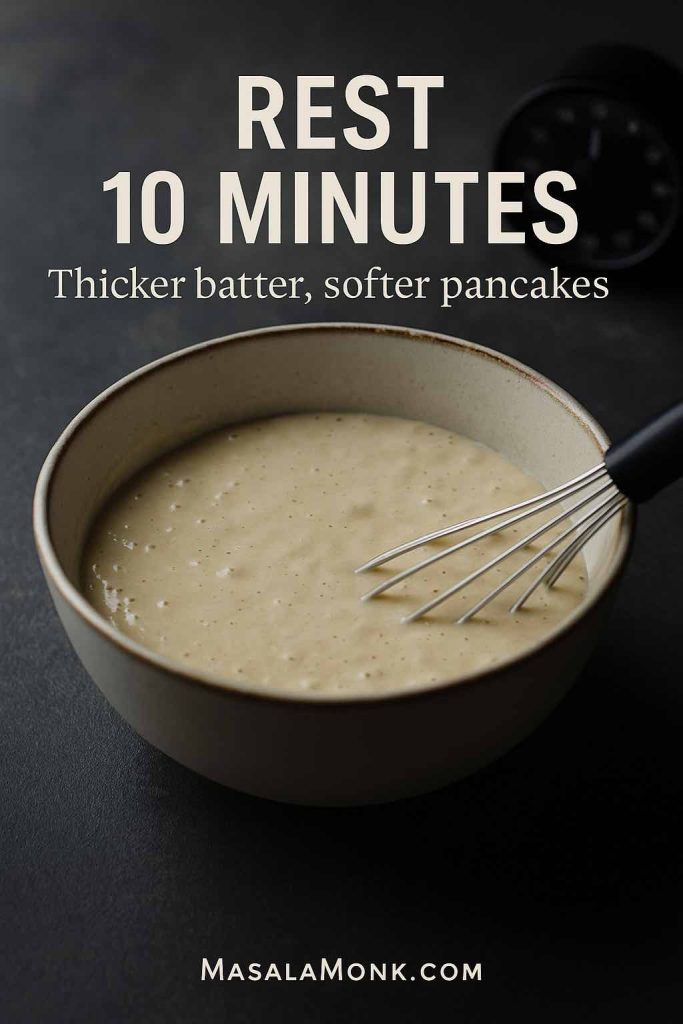
Next, let the batter rest—briefly, not forever
A short rest—about 8 to 15 minutes—lets the flour hydrate and the leavening begin to work. The batter thickens slightly, bubbles form more evenly, and the pancakes cook up softer. Serious Eats has a great, tested perspective on pancake rest and texture: The Easiest, Fluffiest Pancake Recipe.
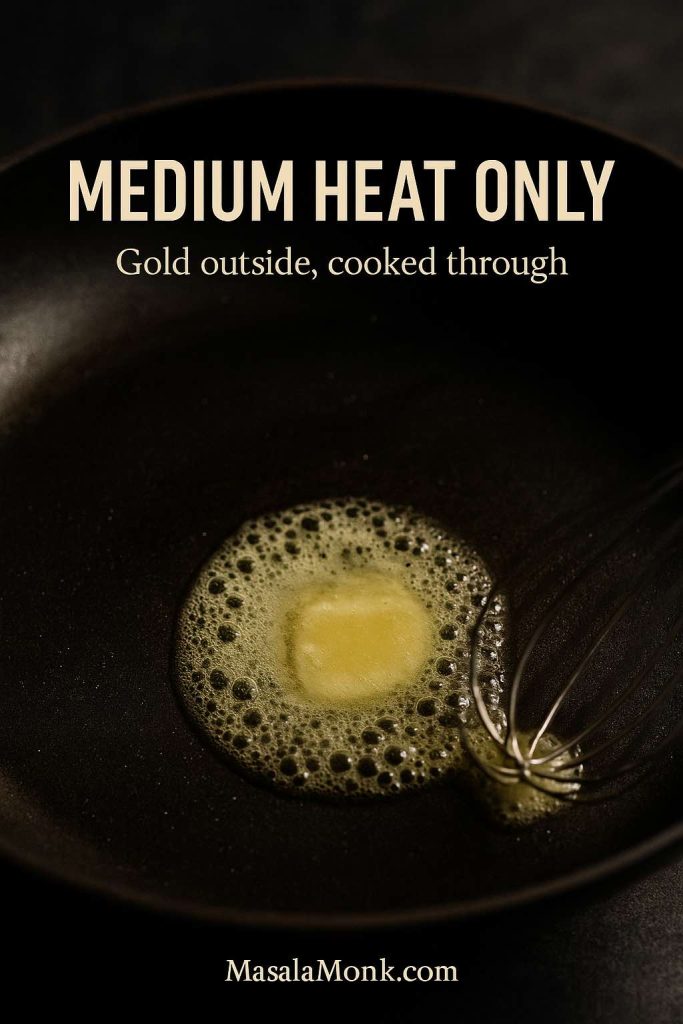
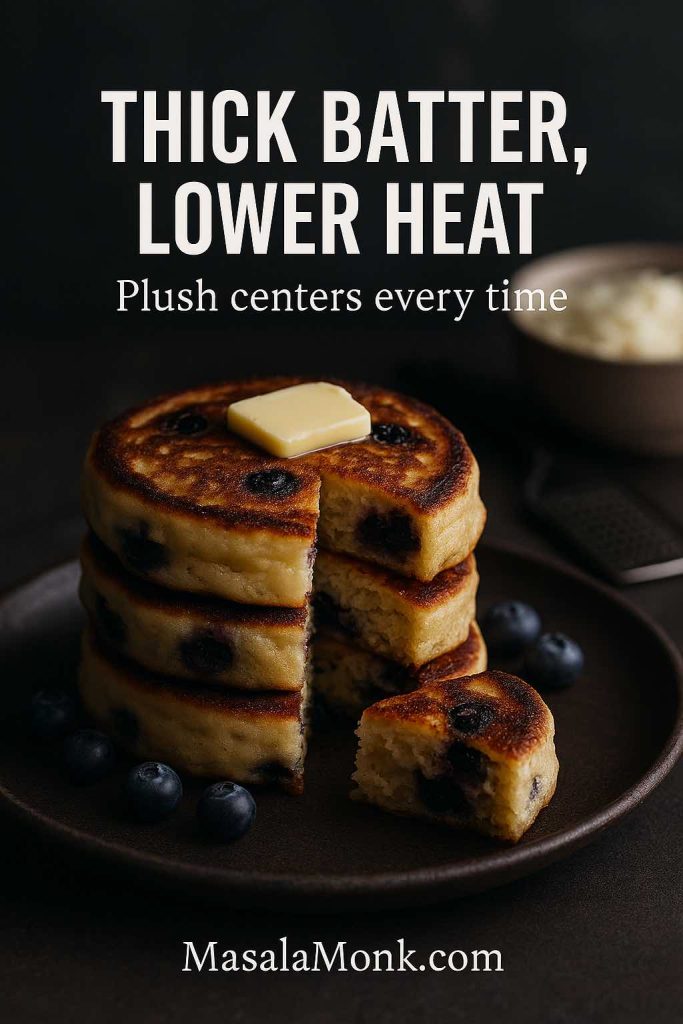
Meanwhile, treat heat like an ingredient
High heat is the fastest way to scorch the outside while leaving the middle undercooked. Low heat, on the other hand, can dry pancakes out before they brown. Medium heat is the sweet spot for most stoves—steady enough to set the center and gentle enough to cook through.
Finally, handle blueberries with intention
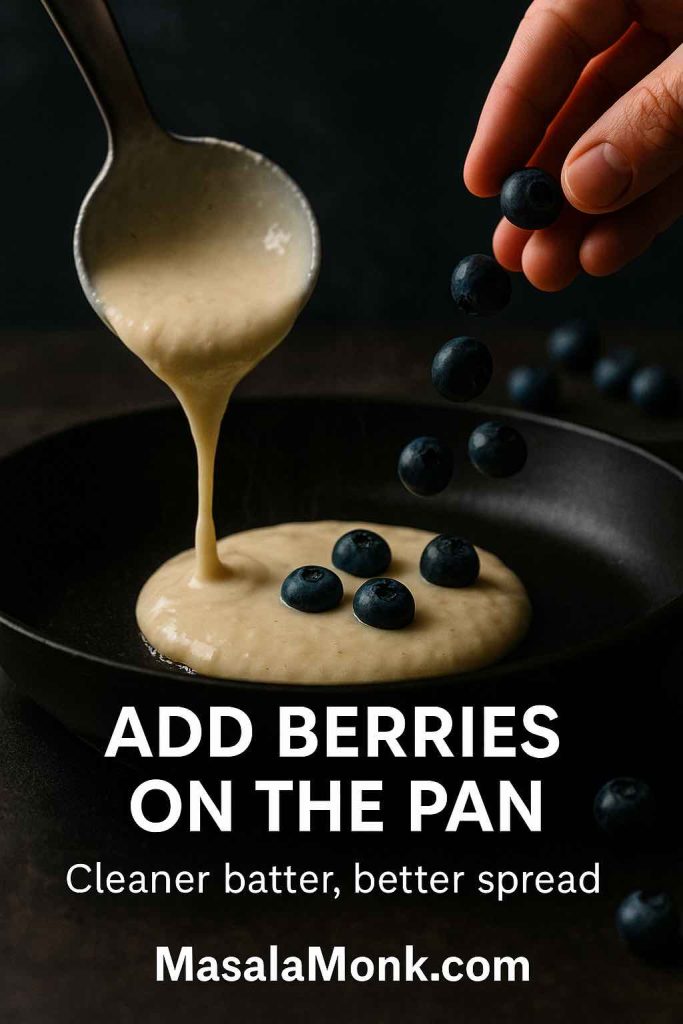
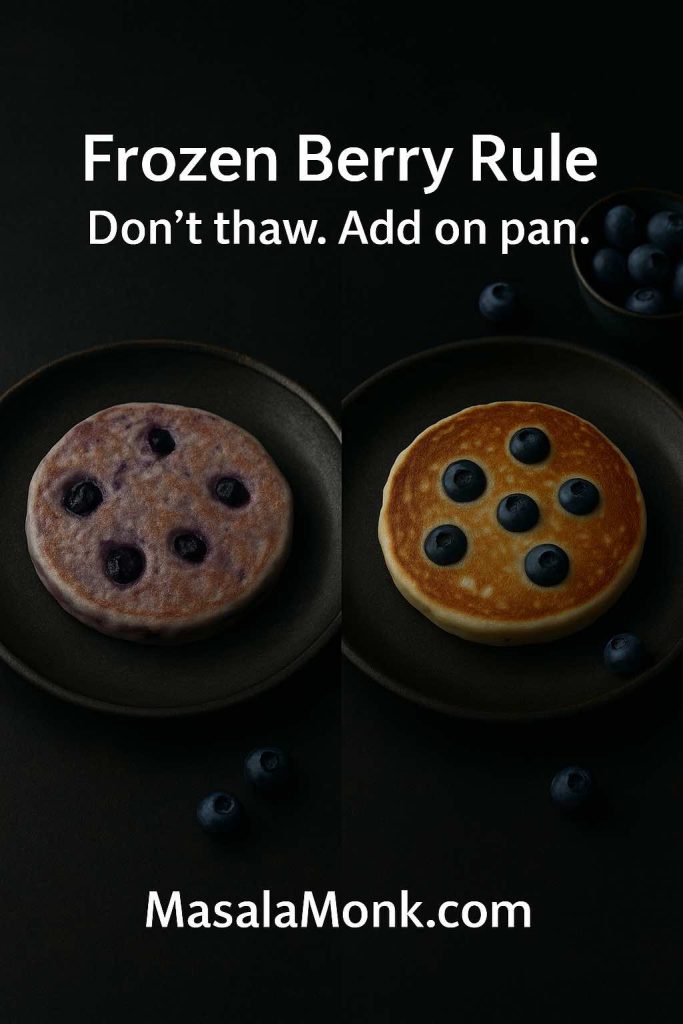
Fresh berries and frozen berries behave differently. Frozen blueberries for pancakes bleed juice as they warm; if you fold them into the bowl, you may end up with purple batter and uneven streaking. Consequently, the simplest move is also the smartest: add blueberries per pancake on the pan rather than mixing all of them into the batter. King Arthur recommends this approach for a reason.
With those basics in place, you’re ready for the classic.
Also Read: Double Chocolate Chip Cookies – Easy Recipe with 7 Variations
Classic Blueberry Pancakes (The Best Blueberry Pancake Base Recipe)
This is the stack that fits almost any situation: weekend brunch, quick weekday comfort, or the kind of morning when you want blueberries and pancakes without fuss. It also forms the backbone for many of the variations below.
Ingredients (makes about 10–12 medium pancakes)
Dry ingredients
- 1 ½ cups (190 g) all-purpose flour
- 2 tbsp (25 g) sugar
- 2 tsp baking powder
- ½ tsp baking soda
- ½ tsp fine salt

Wet ingredients
- 1 ¼ cups (300 ml) buttermilk
- 2 large eggs
- 3 tbsp (45 g) melted butter (or neutral oil)
- 1 tsp vanilla extract (optional)
Berries
- 1 to 1 ¼ cups blueberries (fresh preferred here)
Buttermilk substitute: If you don’t have buttermilk, stir 1 tbsp lemon juice (or vinegar) into 1 ¼ cups milk and let it stand for 5–10 minutes.
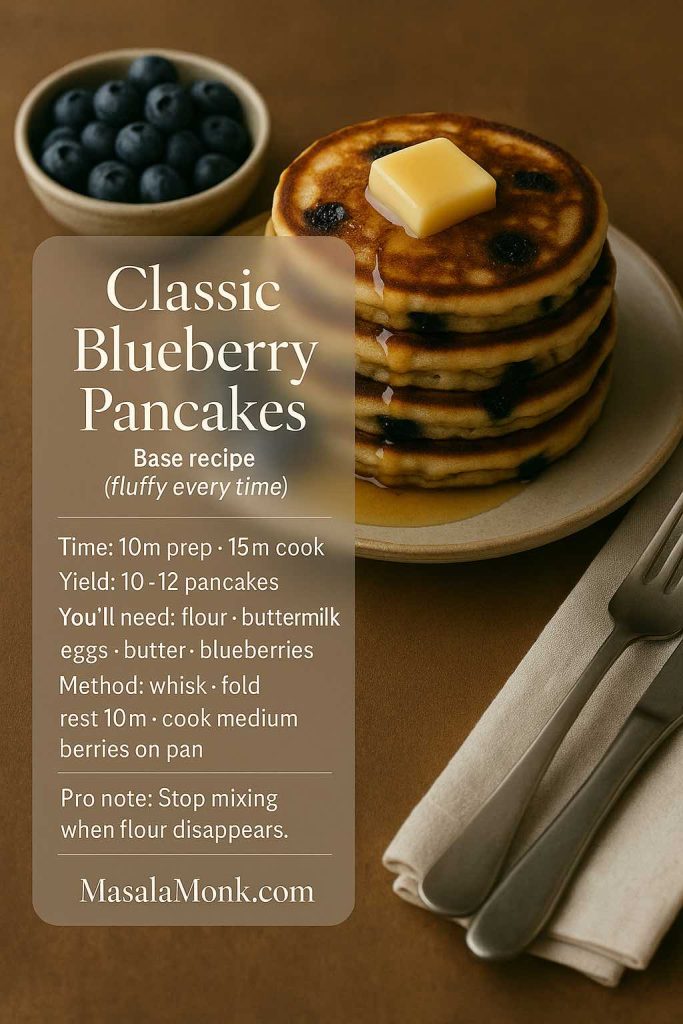
Step by Step Method – How to make Blueberry Pancakes
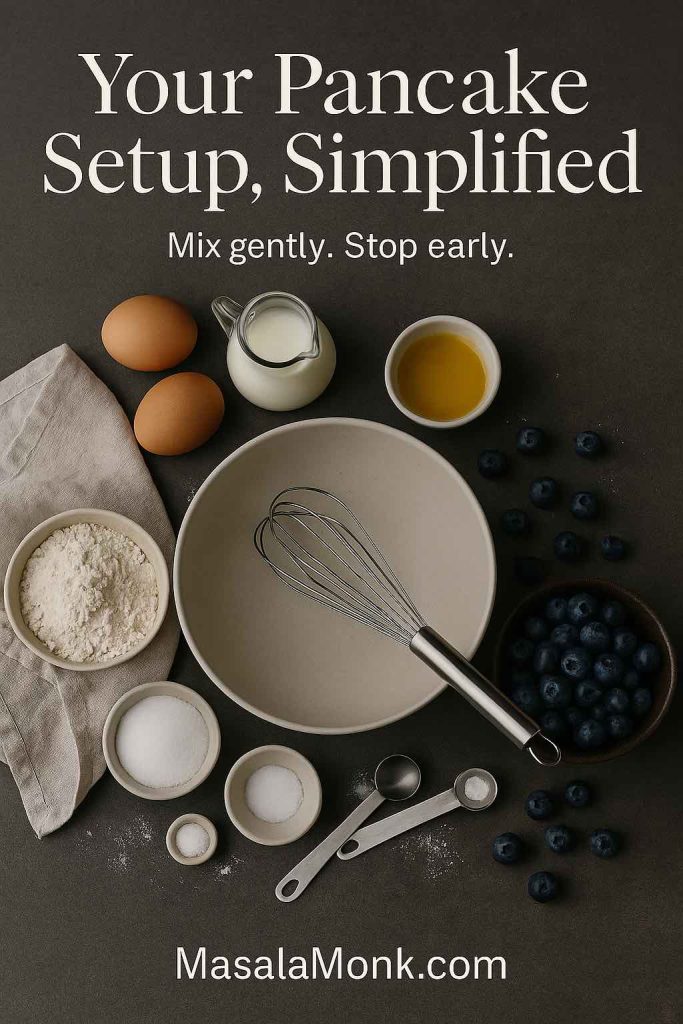
1. Whisk the dry ingredients in a large bowl: flour, sugar, baking powder, baking soda, salt.

2. Whisk the wet ingredients in a second bowl: buttermilk, eggs, melted butter, vanilla.
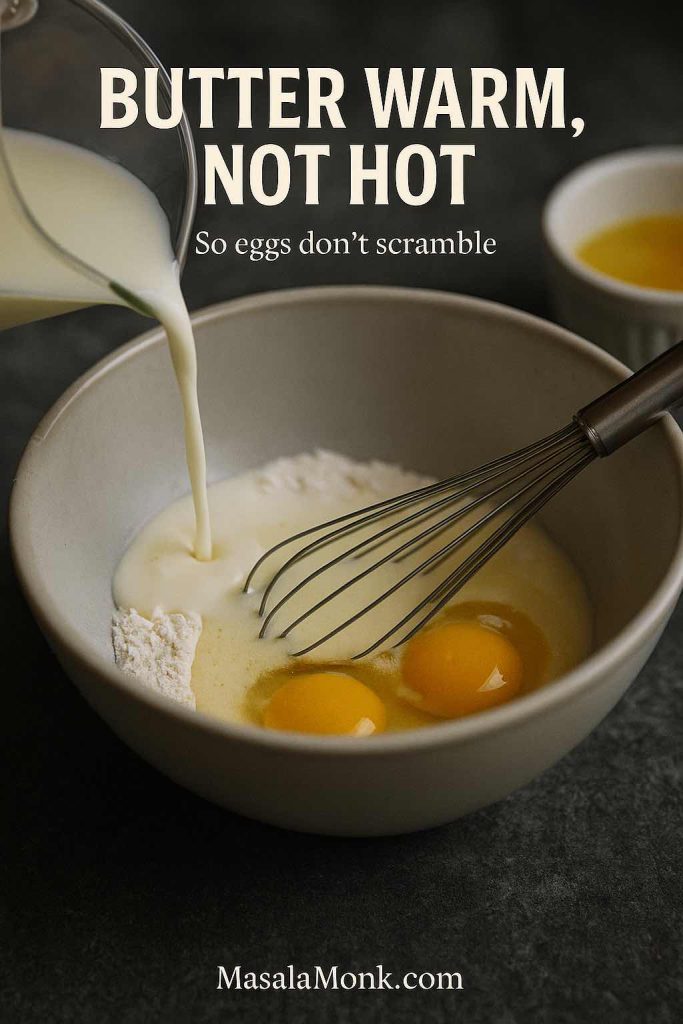
3. Combine gently. Pour wet into dry and fold with a spatula until just combined. Stop the moment the flour disappears.
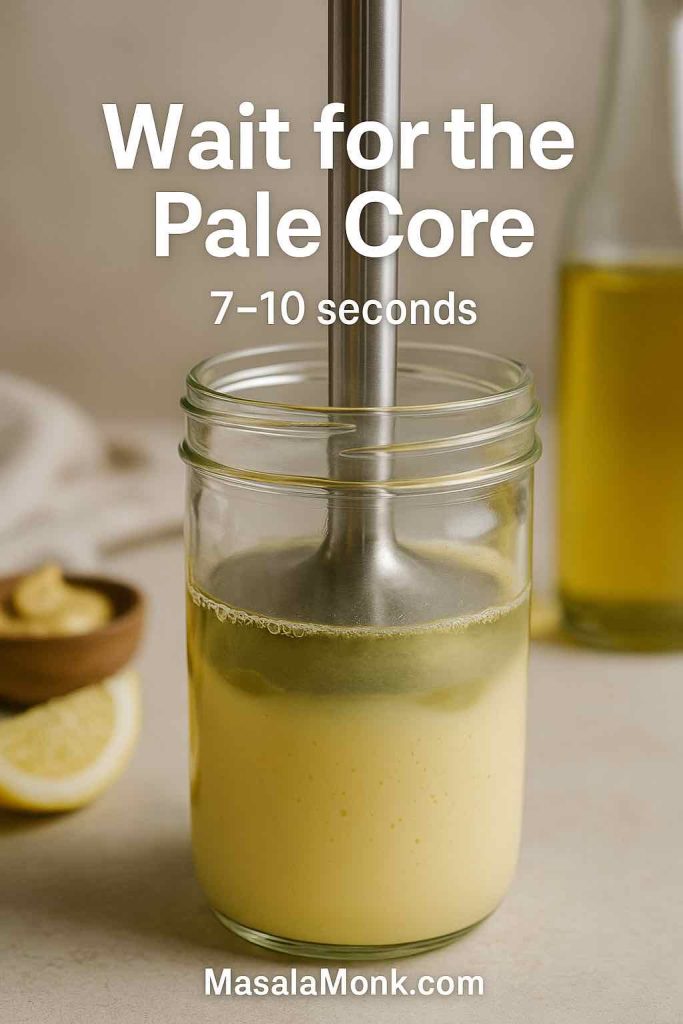
4. Rest the batter for 10 minutes while you warm your pan.
5. Preheat a skillet over medium heat and lightly grease it.
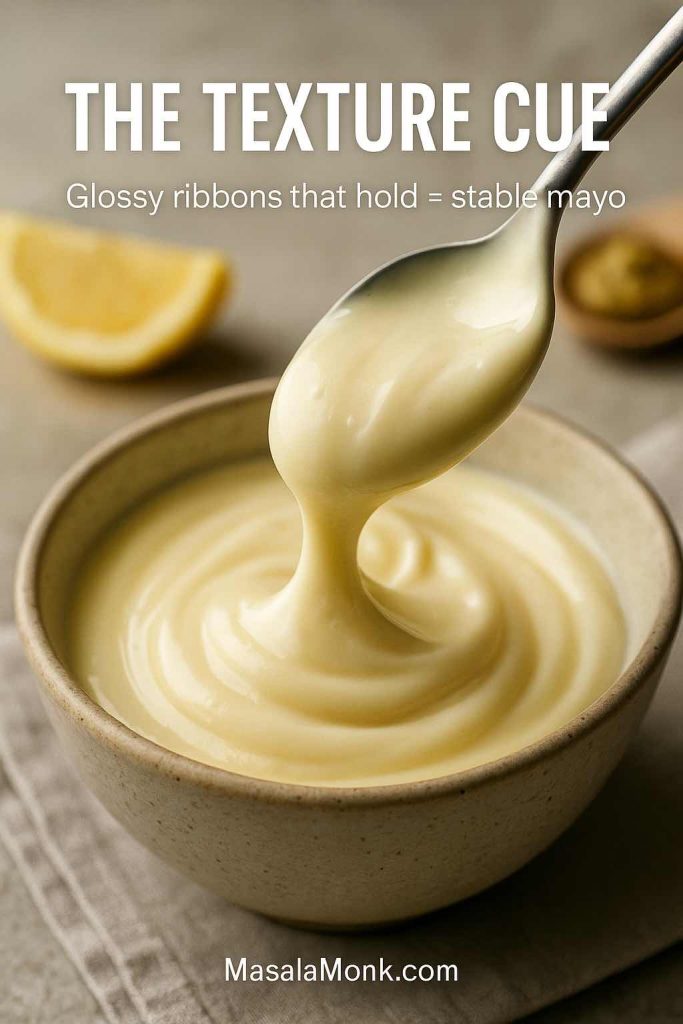
6. Spoon the batter (about ¼ cup per pancake). Immediately sprinkle blueberries on top of each pancake. This keeps the batter from turning grey-purple and ensures berries distribute evenly.
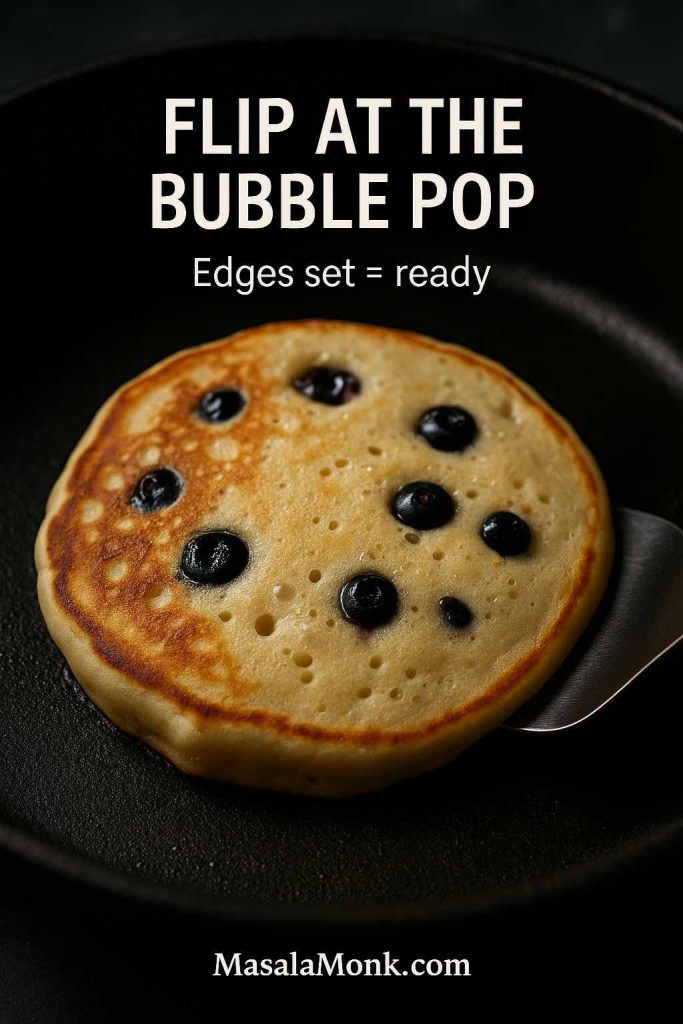
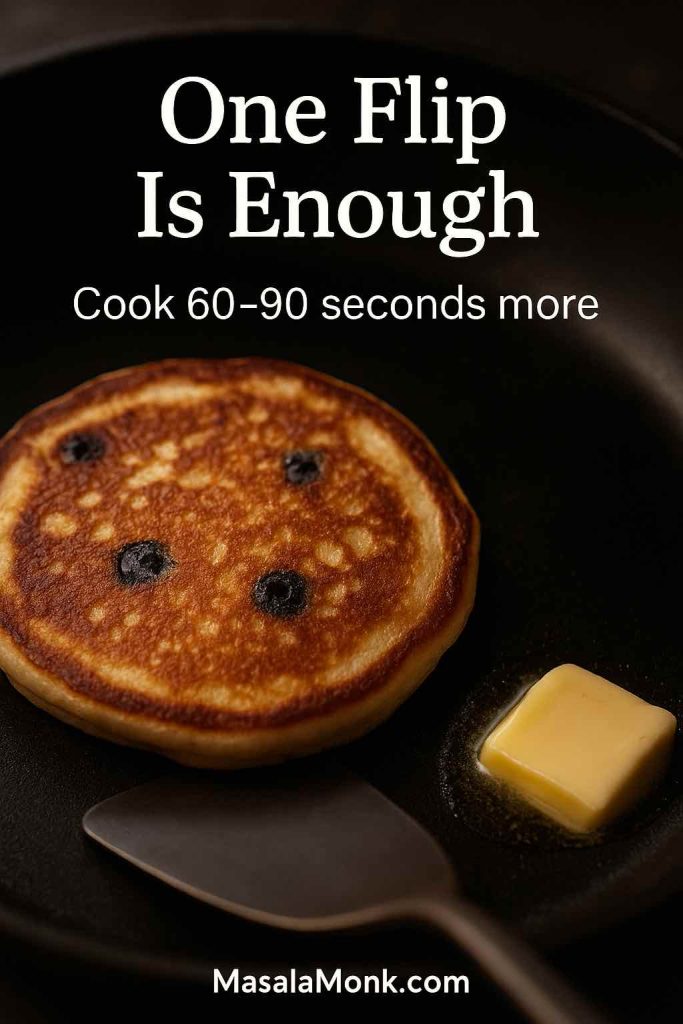
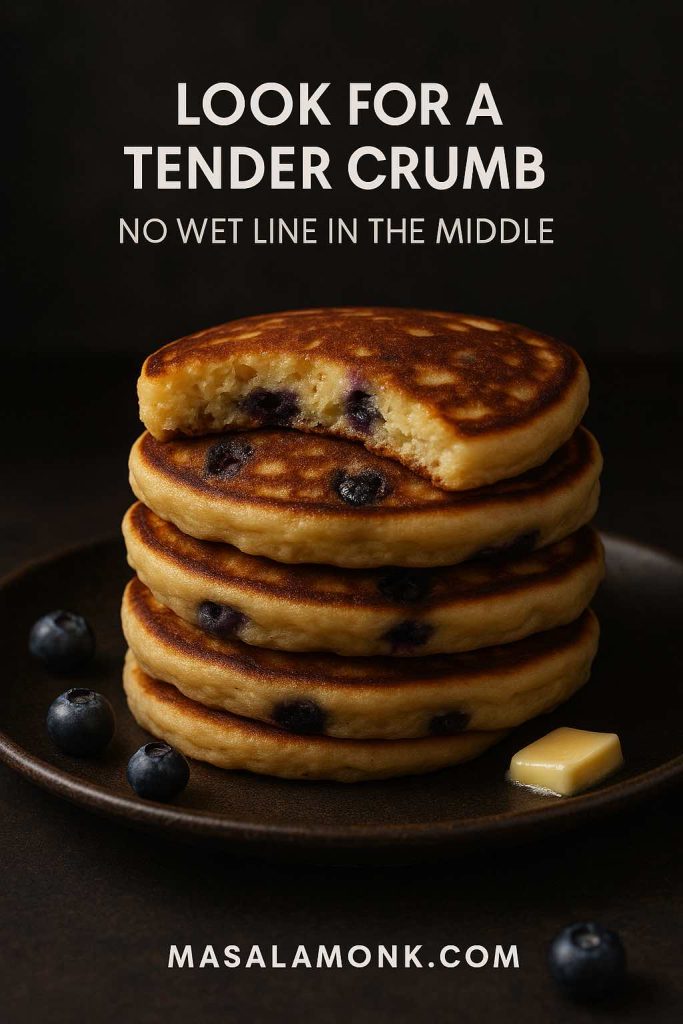
7. Flip when ready. Look for bubbles that rise and pop on the surface and edges that look set. Flip and cook 1–2 minutes more.
Why this classic recipe works
Because the batter is thick enough to suspend bubbles, the rest improves hydration, and the berries are added at the right moment. In other words, the method protects the fluff.
If you’re making a bigger breakfast and want something warm-spiced on the side, you could borrow ideas from fluffy buttermilk pancakes with stewed cinnamon apples—even if you stick with blueberries here.
Blueberry Hotcakes: How to Choose and Store Blueberries for Pancakes
Blueberry hotcakes are only as good as the berries you put in them. Fortunately, “good berries” doesn’t always mean expensive berries—it usually means berries with the right texture and storage.
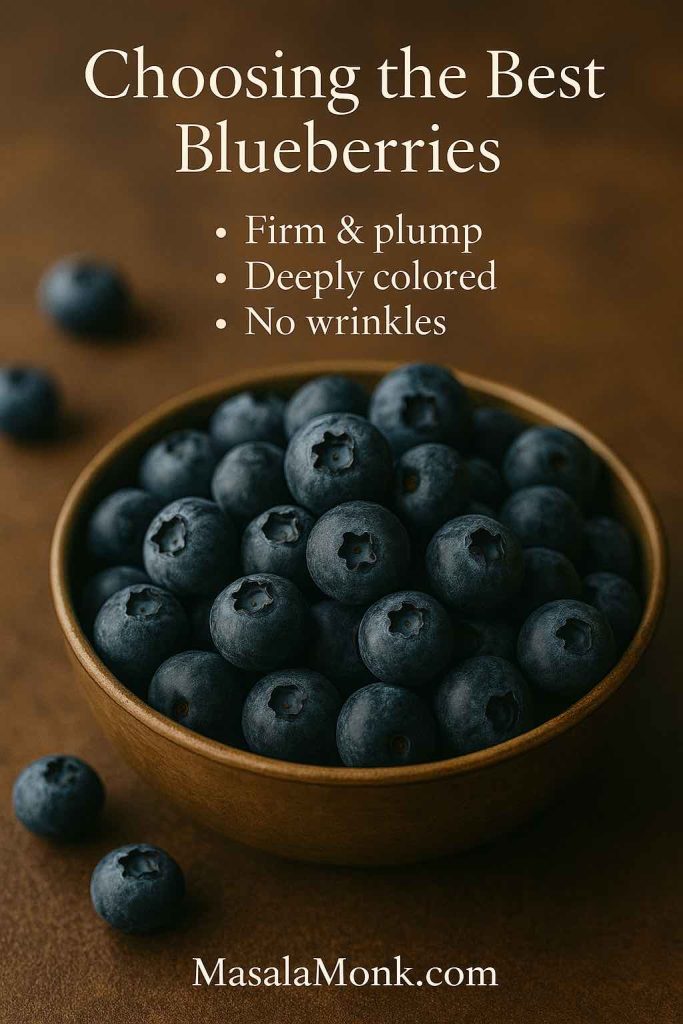
Choosing blueberries
- Look for berries that are plump and deep blue, not shriveled.
- A light silvery “bloom” is normal and protective.
- Avoid wet or leaky containers; moisture speeds spoilage.
For practical storage guidelines on Blueberries, this Martha Stewart guide is straightforward.
Storing blueberries
- Don’t wash berries until you’re ready to use them.
- Keep them chilled and dry.
- If you notice a few soft berries, remove them quickly so the rest stay fresher longer.
If you also enjoy the “why blueberries are good for you” angle—without turning breakfast into homework—this reader-friendly overview is a solid companion: health benefits of blueberries. For a reputable broader look at blueberries and health, the American Heart Association has a helpful summary: fresh or frozen—what to know about blueberries and health.
Now, if fresh berries aren’t an option—or you simply prefer keeping a bag in the freezer—let’s make frozen blueberry pancakes that taste just as good.
Frozen Blueberry Pancakes: How to Use Frozen Blueberries for Pancakes Without Purple Batter
Frozen blueberry pancakes can be wonderful; they can also become streaky and odd-looking if the berries leak too much juice. Thankfully, there’s a calm, dependable approach.
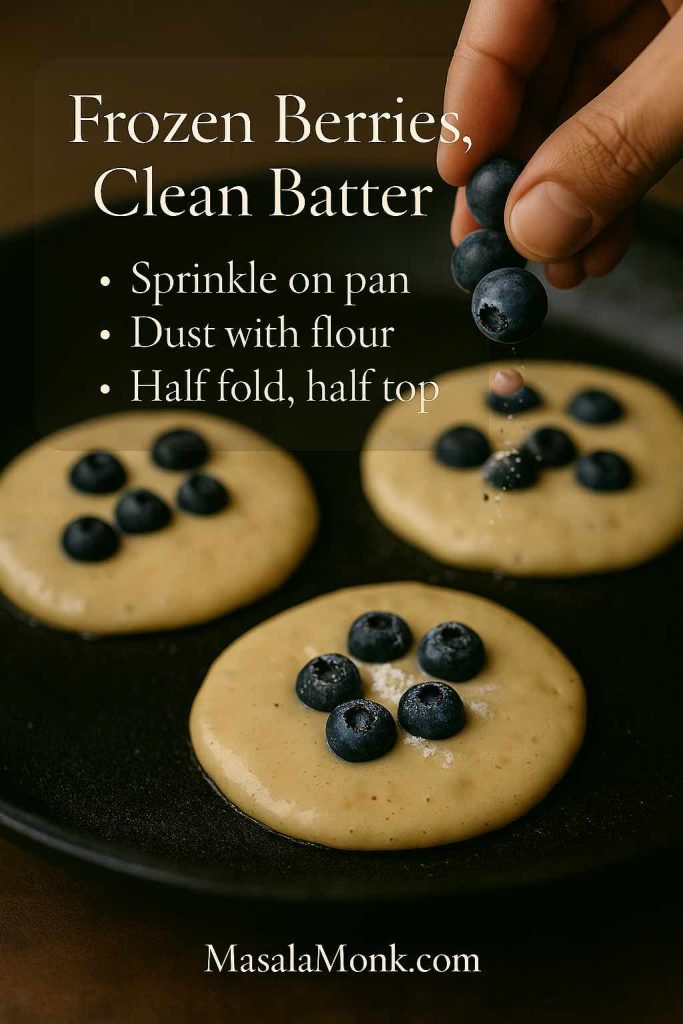
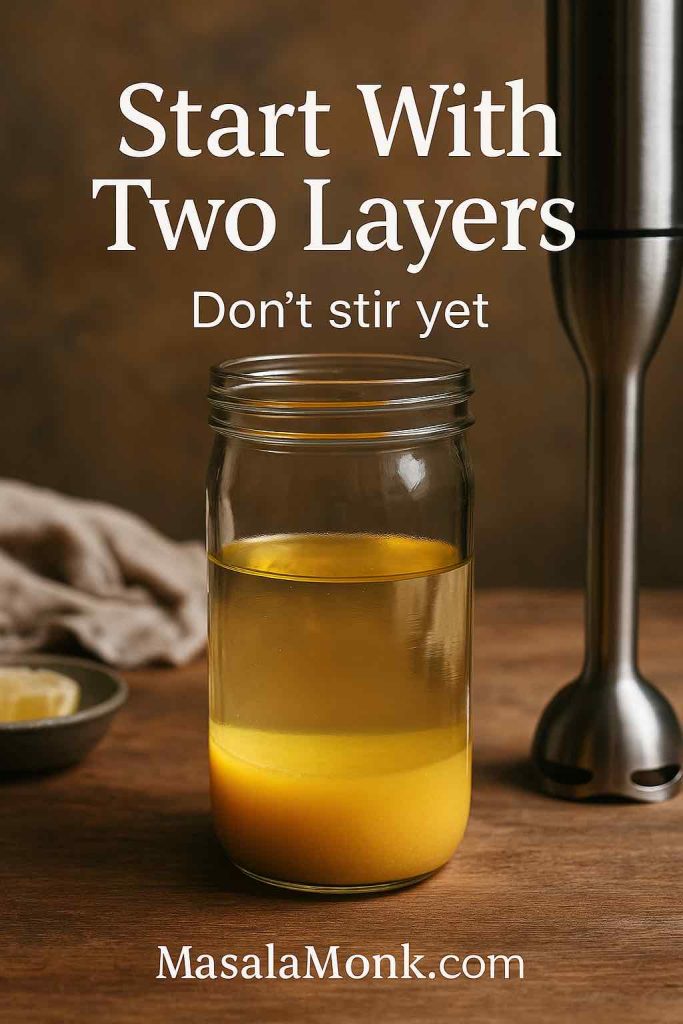
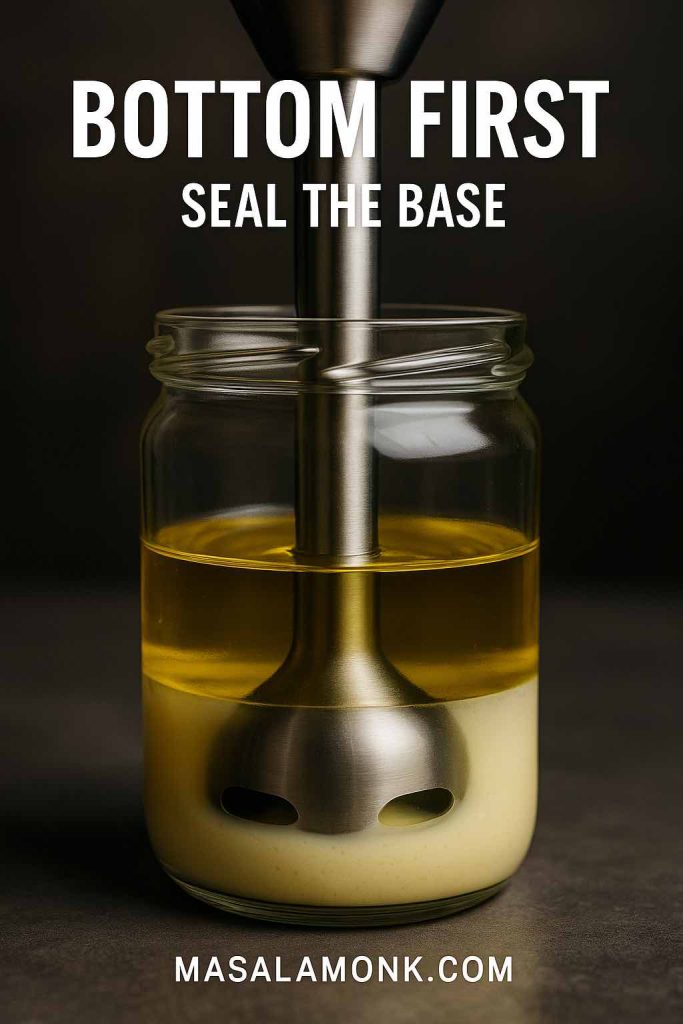
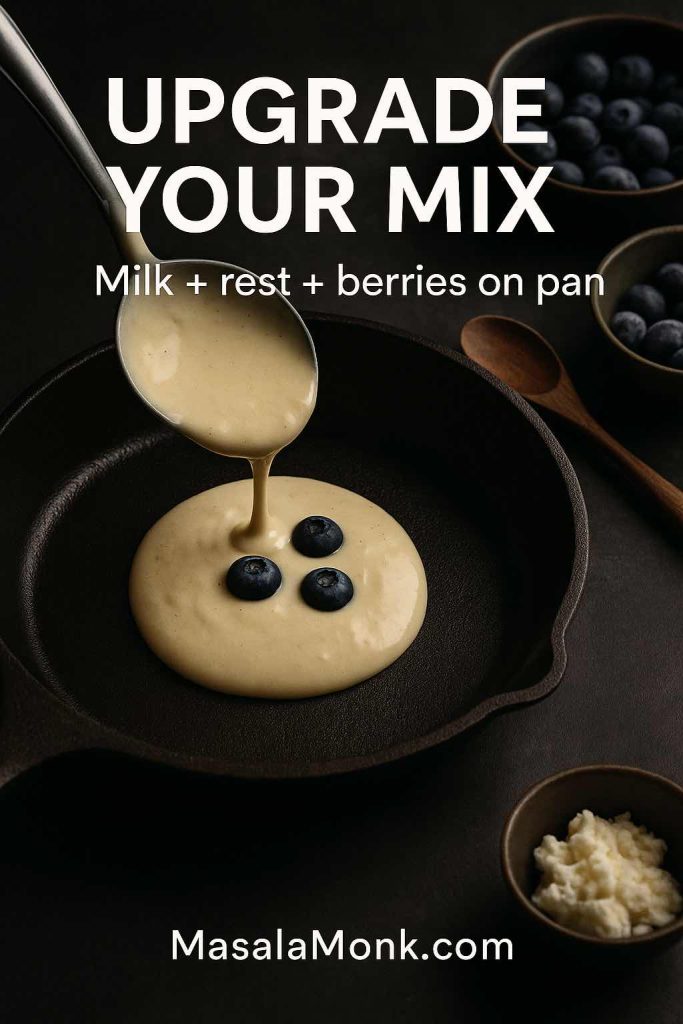
The easiest method: add berries on the pan
Make your batter as usual, then ladle batter onto the hot skillet and sprinkle frozen blueberries right on top. Flip once the edges set. The berries warm inside the pancake rather than staining the whole bowl.

A second method: a light flour coat
If you prefer folding berries into the batter, toss frozen berries with 1 tsp flour per cup of berries. This reduces bleeding and helps the berries grip the batter. Then fold gently and cook immediately.
A third method: half-and-half
Fold in half the berries, then add the rest per pancake on the skillet. This gives you berries throughout without turning everything purple.
For a well-tested, practical take on blueberry handling and pancake texture, King Arthur is again a dependable reference: Blueberry Pancakes recipe.
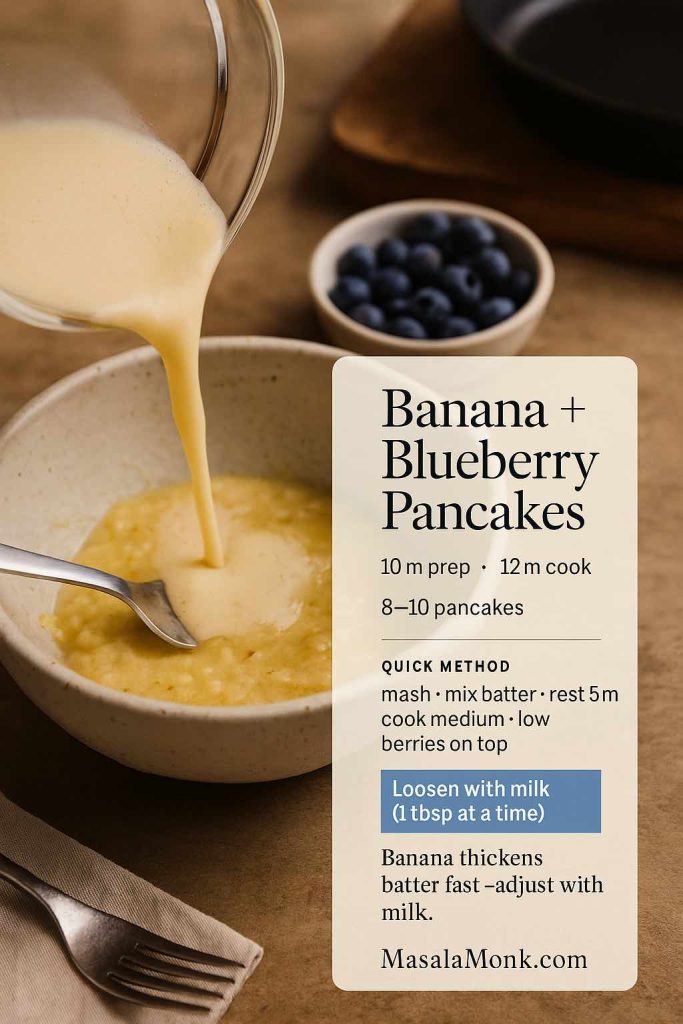
Banana Blueberry Pancake: Banana and Blueberry Pancakes That Stay Light
Banana blueberry pancake batter can become heavy because banana adds moisture and density. The trick is balance: enough banana for sweetness and structure, but not so much that the pancake turns cakey.
Ingredients (makes about 8–10 pancakes)
- 1 ripe banana, mashed (about 120–140 g)
- 1 ¼ cups (160 g) all-purpose flour
- 2 tsp baking powder
- ½ tsp salt
- 1 tbsp sugar or honey (optional, depending on banana)
- 1 large egg
- ¾ cup (180 ml) milk
- 2 tbsp melted butter or oil
- ¾ to 1 cup blueberries
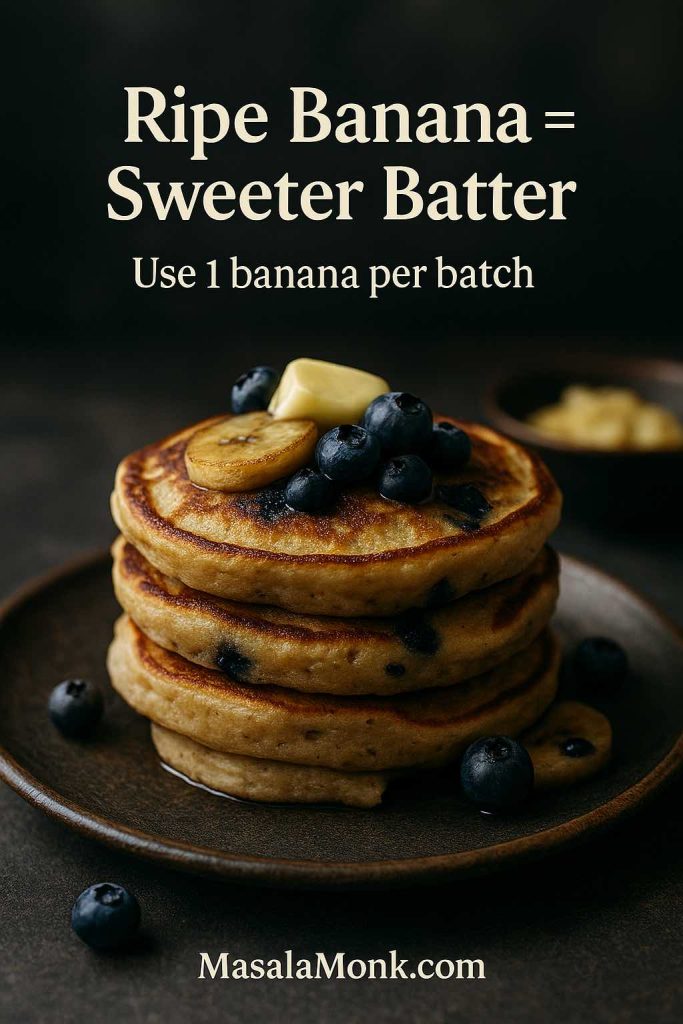
Method
- Mash banana until mostly smooth.
- Whisk in egg, milk, and oil.
- Add flour, baking powder, salt, and sugar if using; fold gently.
- Rest 5–8 minutes.
- Cook on medium heat and add blueberries per pancake on the skillet.
Small upgrades that feel special
- A pinch of cinnamon makes the whole thing taste like banana bread meets blueberry pancakes.
- A little lemon zest brightens the fruit flavour, especially if your blueberries are mild.
If you’re cooking for kids and want another soft breakfast option, you might enjoy apple pancakes for baby-led weaning or toddlers. It’s a different flavour, yet the easy, forgiving style pairs nicely with the banana-blueberry approach.
Also Read: 10 Best Espresso Martini Recipe Variations (Bar-Tested)
Blueberry Lemon Pancake: Bright, Fragrant, and Balanced
A blueberry lemon pancake should taste sunny, not sour. That’s why zest matters more than juice. Juice adds acidity; zest adds aroma and perceived sweetness.
Ingredients (makes about 10 pancakes)
- 1 ½ cups (190 g) flour
- 2 tbsp sugar
- 2 tsp baking powder
- ½ tsp baking soda
- ½ tsp salt
- Zest of 1 lemon
- 1 ¼ cups buttermilk
- 2 eggs
- 3 tbsp melted butter
- 1 cup blueberries

Method
- Whisk flour, sugar, baking powder, baking soda, salt, lemon zest.
- Whisk buttermilk, eggs, melted butter.
- Combine gently; rest 10 minutes.
- Cook on medium heat; add blueberries per pancake on the pan.
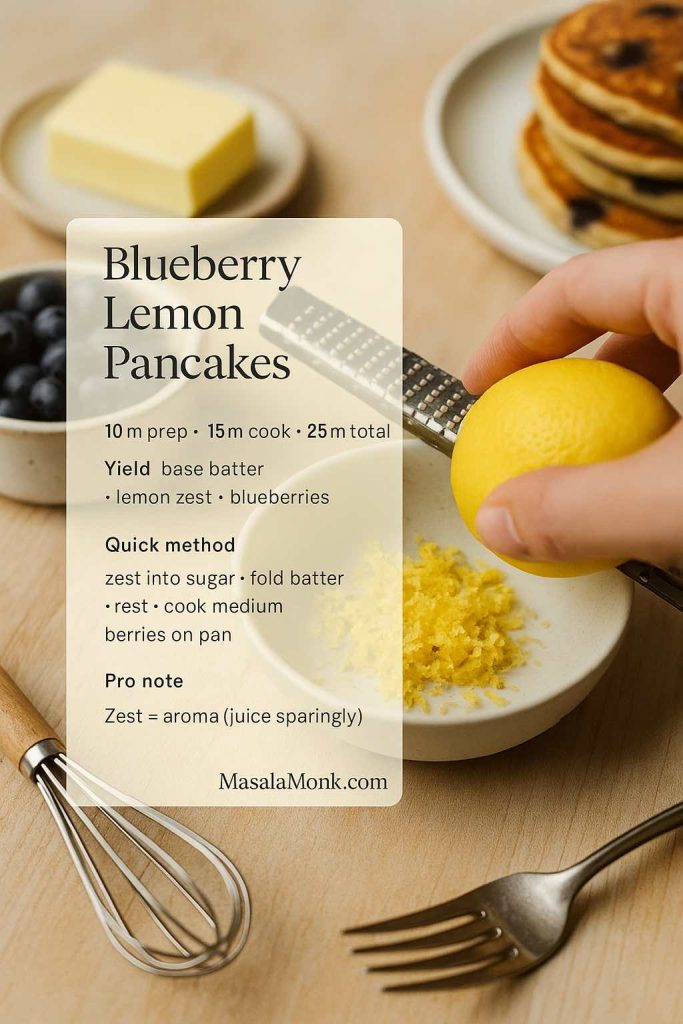
Turning this into blueberry lemon ricotta pancakes
If you want blueberry lemon ricotta pancakes—one of the most craveable brunch variations—stir ⅓ to ½ cup ricotta into the wet ingredients. If the batter looks too thick afterward, loosen it with a splash of milk. The result is softer, richer, and still balanced.
For a topping that leans into the citrus, lemon curd is a classic companion. If you’d like a reliable method you can make once and use all week, this is a solid starting point: silky smooth lemon curd.
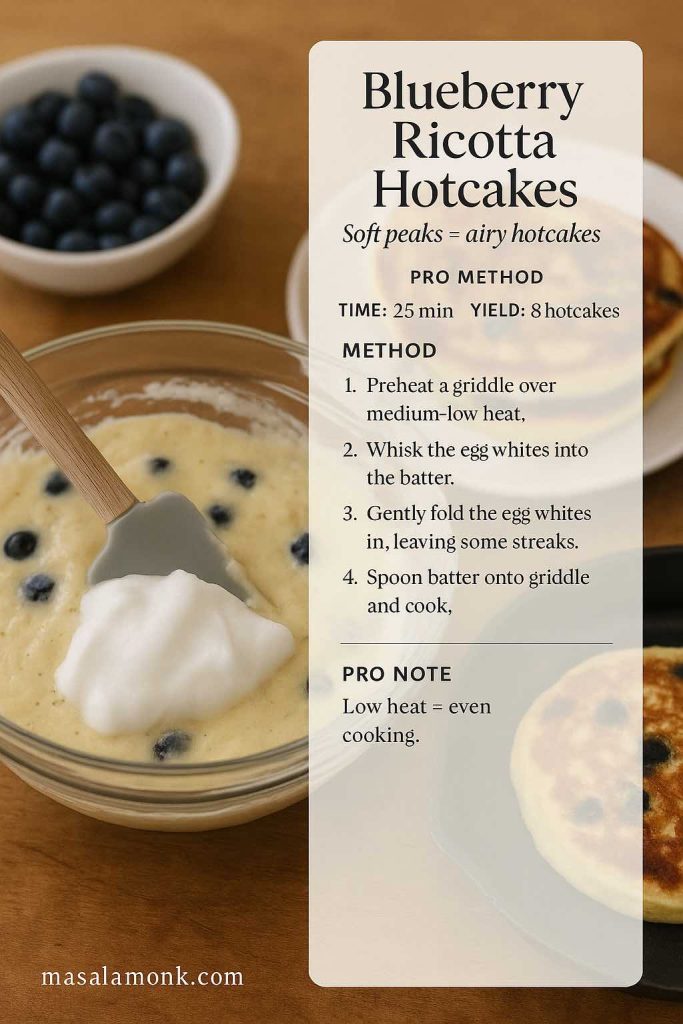
Blueberry Ricotta Hotcakes: Blueberry and Ricotta Pancakes With a Café Feel
Blueberry ricotta hotcakes are tender and slightly rich, the kind of breakfast that feels like a treat even if you’re still in your pajamas. They also align beautifully with searches for blueberry and ricotta pancakes and blueberry ricotta hotcakes because the texture really is different: softer, thicker, and more luxurious.
Ingredients (makes about 8–10 thicker pancakes)
- 1 ¼ cups (160 g) flour
- 2 tbsp sugar
- 2 tsp baking powder
- ½ tsp salt
- 3 eggs, separated
- 1 cup ricotta
- ¾ cup milk (plus a bit more if needed)
- 1 tsp vanilla
- 1 tbsp melted butter or oil
- 1 cup blueberries
Method
- Whisk flour, sugar, baking powder, salt in a bowl.
- In a separate bowl, whisk egg yolks, ricotta, milk, vanilla, melted butter.
- Combine wet and dry gently.
- Whip egg whites to soft peaks and fold them into the batter. This step is what makes the hotcakes airy rather than heavy.
- Cook on medium-low heat because the batter is thicker. Add blueberries per pancake on the skillet.
A lovely pairing
If you’re building a brunch plate, these ricotta hotcakes work beautifully with something crisp and salty—especially bacon cooked in a way that doesn’t splatter your kitchen. This method is simple and reliable: how to cook bacon in the oven.
High Protein Blueberry Pancakes: Blueberry Protein Pancakes That Don’t Taste “Healthy”
High protein blueberry pancakes get searched for constantly, yet many recipes lean too hard on protein powder and end up chalky. Instead, the goal is to keep the pancake structure familiar and use protein in a way that supports tenderness.
Below are two dependable routes: blueberry cottage cheese pancakes (especially easy) and a Greek-yogurt approach that can include protein powder without taking over.
Blueberry Cottage Cheese Pancakes (Blender Option)
These blueberry cottage cheese pancakes are especially popular because they cook up tender and filling, and the batter comes together quickly.
Ingredients
- 1 cup cottage cheese
- 2 eggs
- ½ cup rolled oats (or oat flour)
- 1 tsp baking powder
- ½ tsp vanilla
- Pinch of salt
- ¾ cup blueberries
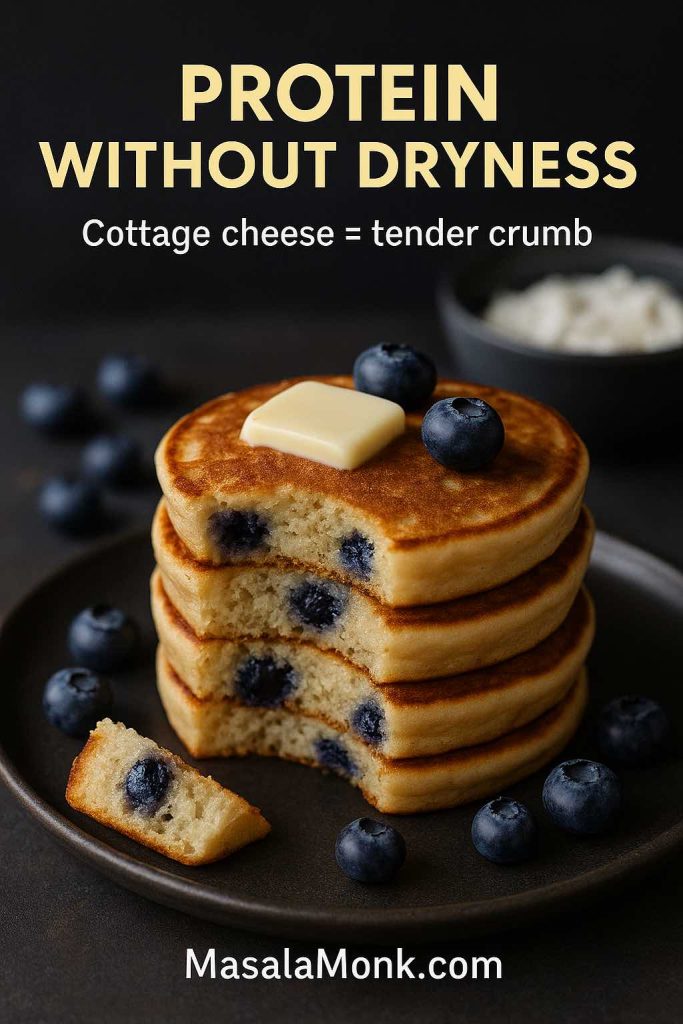
Method
- Blend cottage cheese, eggs, oats, baking powder, vanilla, and salt until smooth.
- Rest 5 minutes; the batter thickens slightly.
- Cook on medium-low heat; add blueberries per pancake on the pan.
- Flip gently once edges set.
If you enjoy learning how cottage cheese can fit into breakfasts beyond pancakes, this is a helpful read: cottage cheese for breakfast.

Blueberry Pancakes Protein Style (Greek Yogurt + Optional Protein Powder)
This version targets blueberry protein pancakes and blueberry pancakes protein queries naturally because the recipe genuinely is protein-forward—yet it still tastes like a pancake.
Ingredients
- 1 cup flour (or ½ flour + ½ oat flour)
- 2 tsp baking powder
- ½ tsp salt
- ¾ cup milk
- ½ cup Greek yogurt
- 2 eggs
- 1 tbsp honey or sugar
- Optional: 1 scoop protein powder (whey or plant)
- ¾ to 1 cup blueberries

Method
- Mix dry ingredients first (including protein powder if using).
- Whisk milk, yogurt, eggs, honey.
- Combine gently; rest 8–10 minutes.
- Cook on medium heat; add blueberries per pancake on the skillet.
If you’re into high-protein breakfast planning more broadly, you might also like how to eat 100 grams of protein a day, as well as high protein overnight oats for mornings when you want “grab-and-go” instead of “stand-and-flip.”
For another protein-leaning pancake idea that’s fruit-based, this is a fun variation to browse: protein rich cherry pancakes.
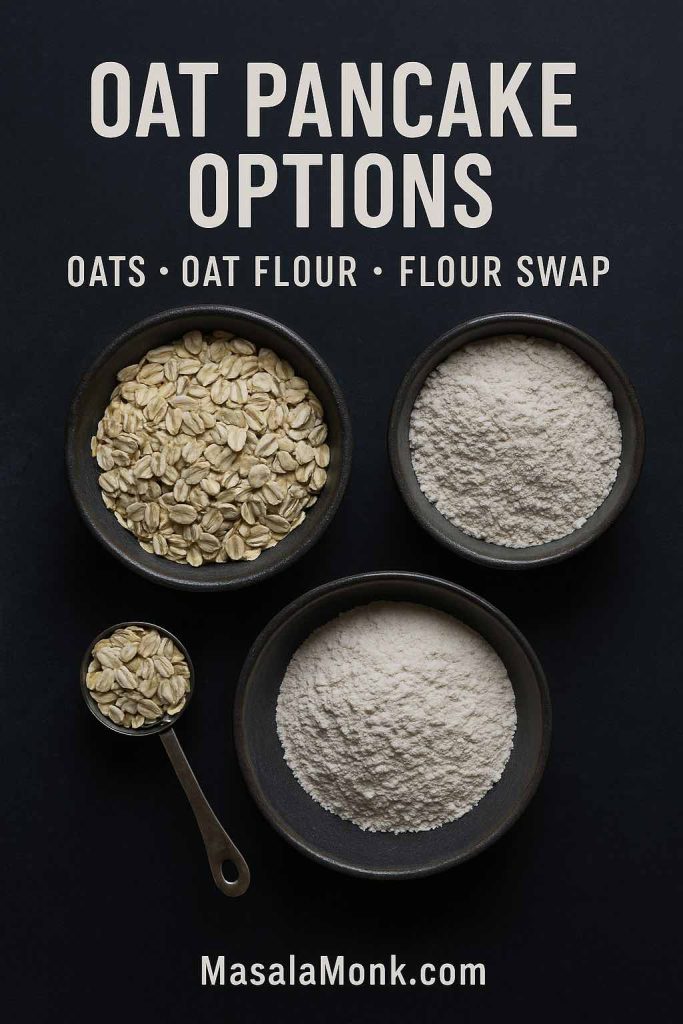
Blueberry Oat Pancakes and Blueberry Oatmeal Pancake Variations
Blueberry oat pancakes sit in a sweet spot: heartier than classic flour pancakes, lighter than a dense “health” pancake, and ideal for anyone who wants a blueberry oatmeal pancake that still feels fluffy.
Here are two options—one softer and one more rustic—so you can pick based on what you have.
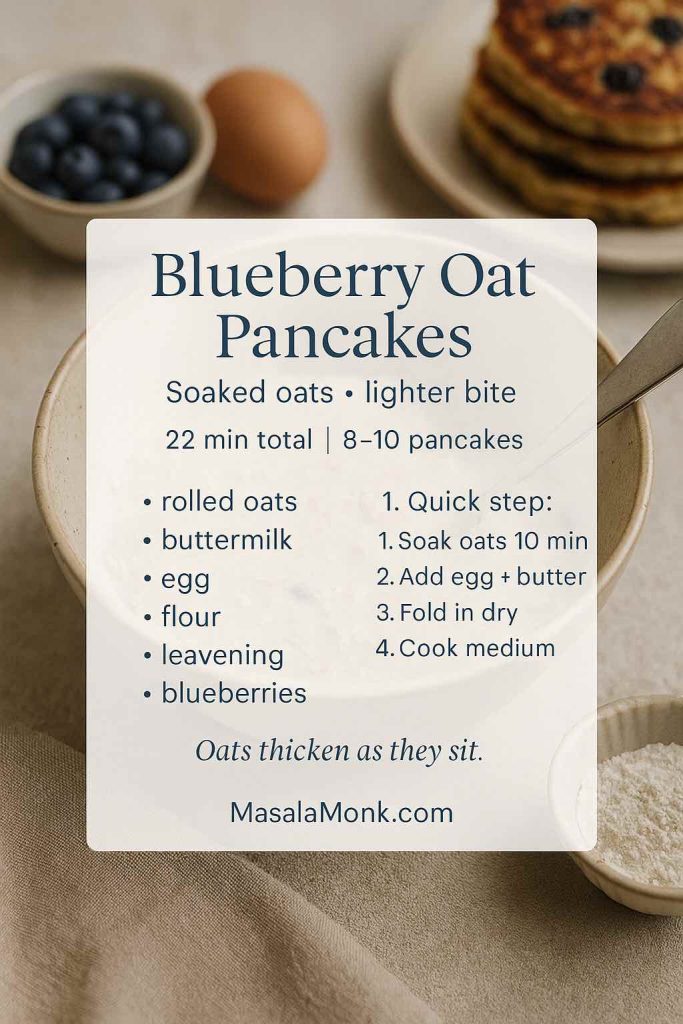
Option A: Soaked-Oat Blueberry Oatmeal Pancake
Ingredients
- 1 cup rolled oats
- ¾ cup buttermilk (or milk + lemon)
- ¾ cup flour
- 1 tbsp sugar or honey
- 1 ½ tsp baking powder
- ½ tsp baking soda
- ½ tsp salt
- 1 egg
- 2 tbsp melted butter or oil
- ¾ to 1 cup blueberries
Method
- Combine oats and buttermilk; soak 10–15 minutes.
- Add egg and melted butter.
- Fold in flour, sugar, baking powder, baking soda, salt.
- Cook on medium heat; add blueberries per pancake.
Option B: Oat-Flour Blueberry Oat Pancakes
This is smoother and more uniform.
Swap
- Replace ⅓ of the flour in the classic recipe with oat flour.
Let the batter rest the full 10–15 minutes so oat flour hydrates properly.
If you’re building meal-prep breakfasts, these oat-based pancakes pair nicely with snackable, make-ahead items like healthy oat protein bars.
Blueberry Pancakes Gluten Free: Blueberry Gluten Free Pancakes and Almond Flour Blueberry Pancakes
Gluten-free blueberry pancakes can be just as tender as the classic if you choose the right structure. Instead of chasing a “perfect substitute,” pick a method that suits the ingredients you have.
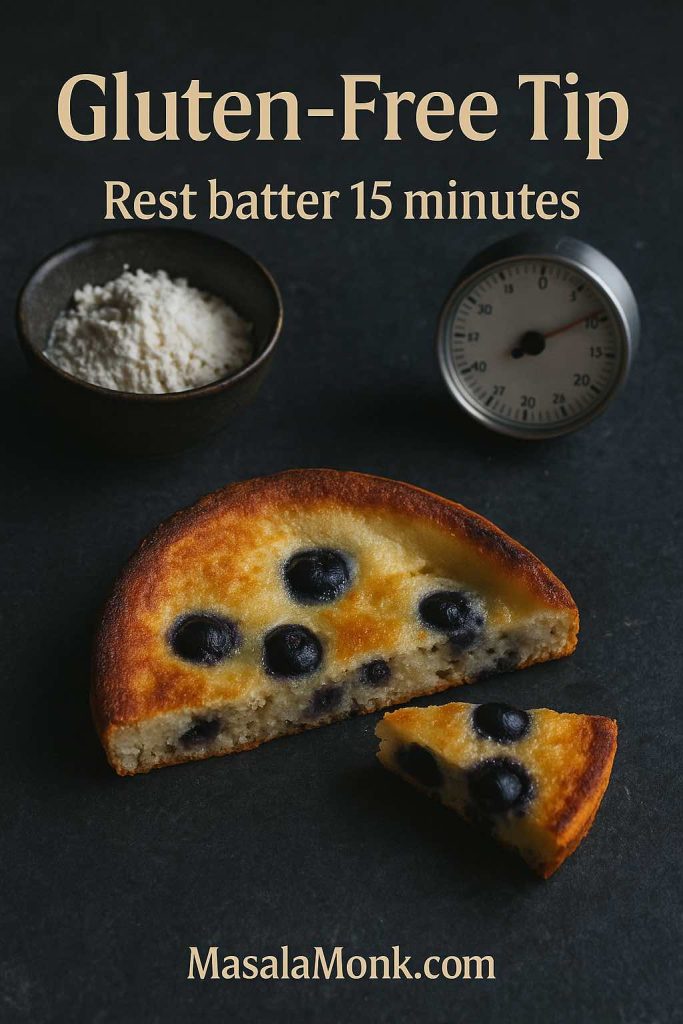
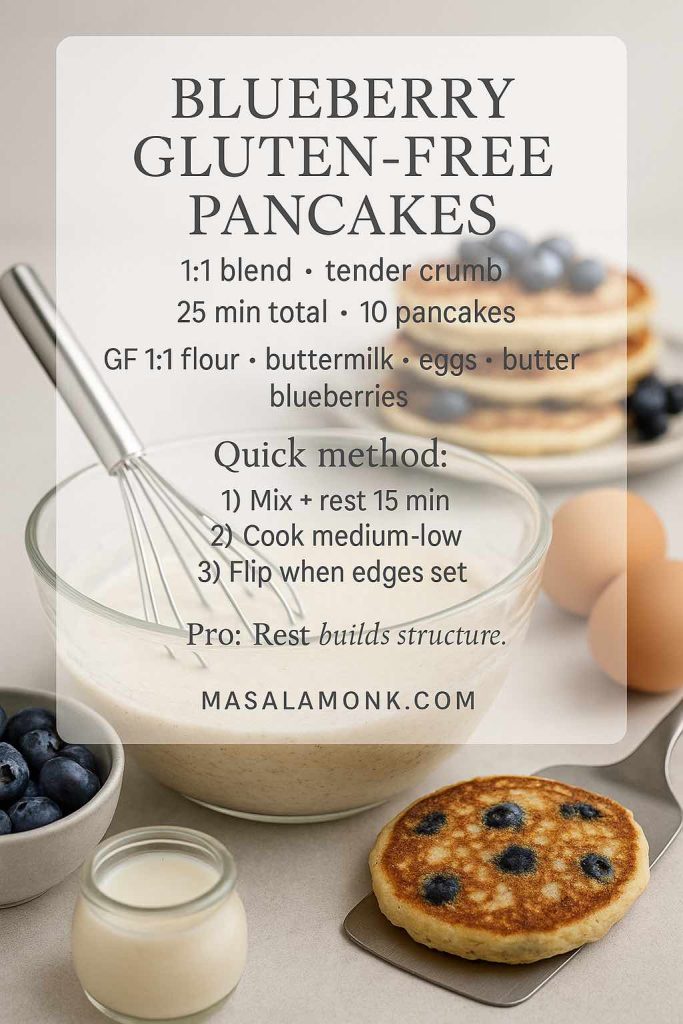
Approach 1: Blueberry Pancakes Gluten Free with a 1:1 Blend
Use your favourite gluten-free 1:1 flour blend in place of all-purpose flour in the classic recipe. Then add one small adjustment: let the batter rest 15 minutes instead of 10. That extra time helps the starches hydrate, which improves tenderness.
Approach 2: Almond Flour Blueberry Pancakes (Tender and Rich)
Almond flour blueberry pancakes tend to be moist and slightly rich; however, almond flour alone can be fragile. So this hybrid approach keeps them tender yet sturdy.
Ingredients
- ¾ cup almond flour
- ½ cup gluten-free 1:1 blend (or oat flour)
- 2 tsp baking powder
- ½ tsp salt
- 2 eggs
- ¾ cup milk (dairy or plant)
- 2 tbsp melted butter or oil
- 1 tbsp honey or sugar
- ¾ cup blueberries
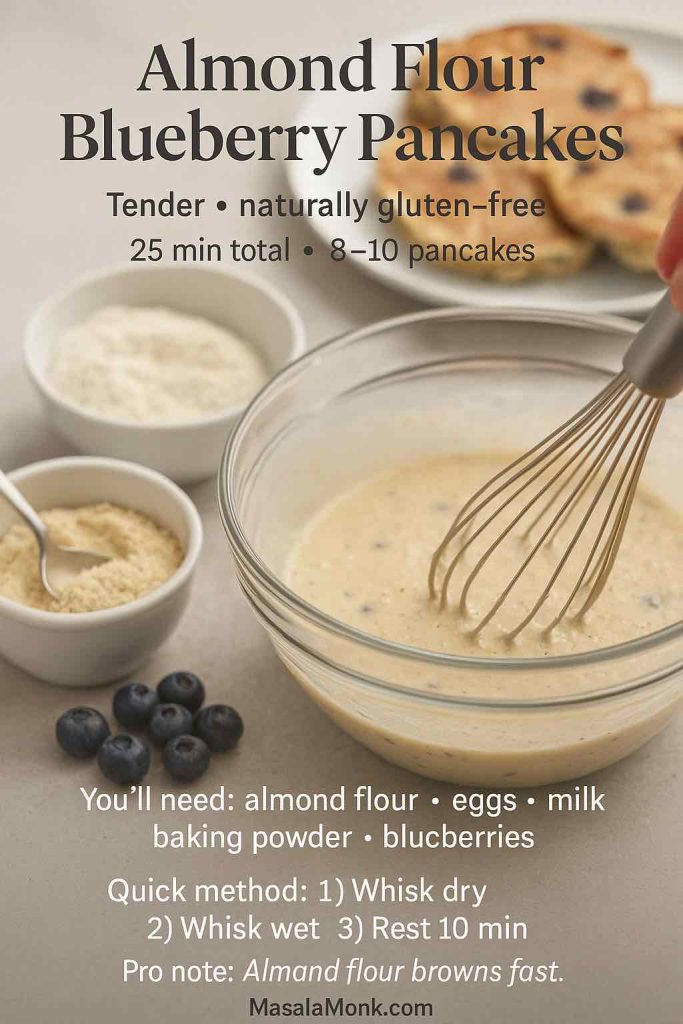
Method
- Whisk dry ingredients.
- Whisk wet ingredients.
- Combine gently; rest 10 minutes.
- Cook on medium-low heat; add blueberries per pancake.
If you like exploring other gluten-free pancake styles, you might enjoy healthy millet protein packed pancakes as another naturally gluten-free direction.
Blueberry Pancake Mix: A Homemade Pancake Mix You’ll Actually Use
A blueberry pancake mix isn’t just about speed. It’s about setting yourself up for mornings when you want pancakes and blueberries without measuring five different leaveners while half-awake.
This homemade pancake mix is a neutral base: you can use it for classic pancakes, blueberry pancakes with pancake mix, blueberry mini pancakes, and even a quick blueberry Dutch pancake. Moreover, if you keep it in an airtight jar, it’s ready whenever you are.
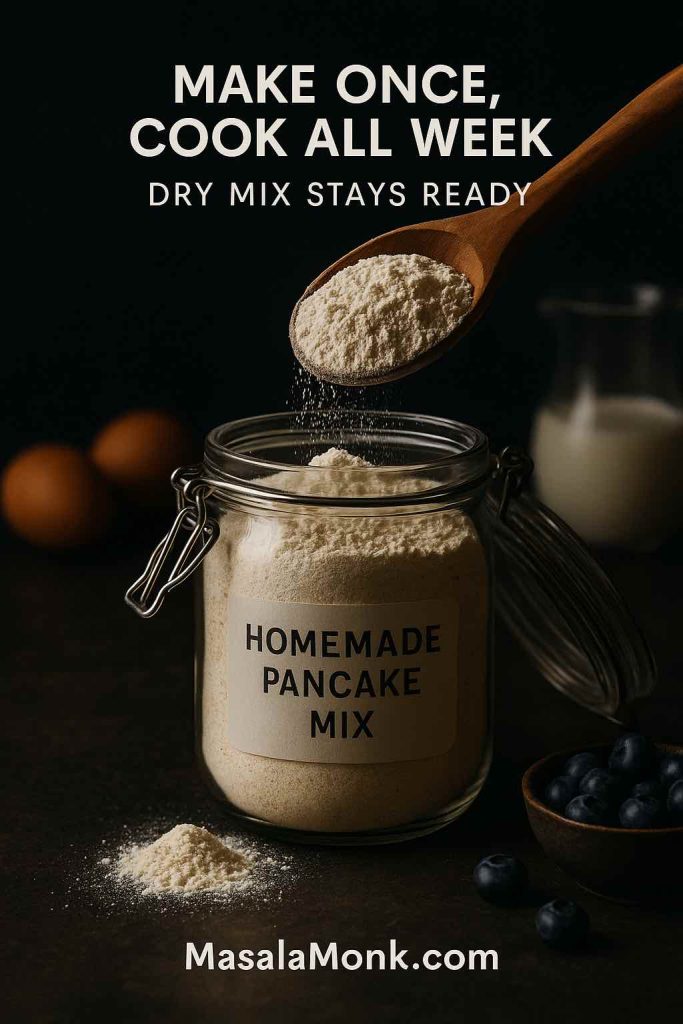
Homemade Pancake Mix (makes about 4–5 batches)
- 4 cups (500 g) all-purpose flour
- ¼ cup (50 g) sugar
- 4 tbsp baking powder
- 1 tbsp baking soda
- 2 tsp fine salt
Whisk thoroughly and store airtight.
If you ever wonder whether your baking powder still has life, King Arthur has an easy freshness test: how to test baking powder and baking soda.
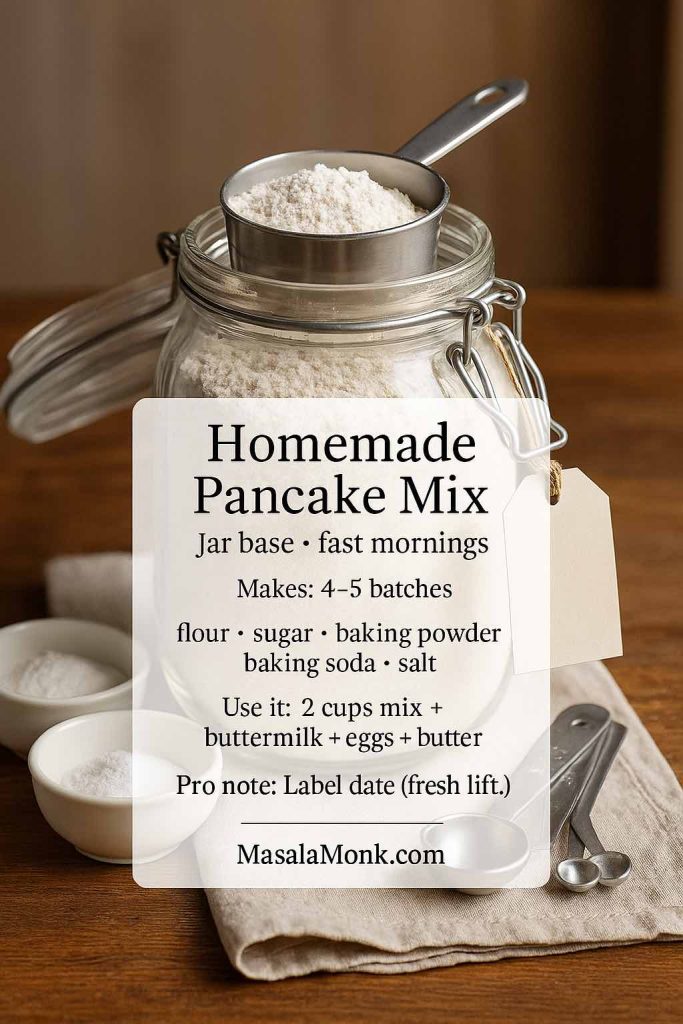
Turning the mix into pancakes (one batch)
- 2 cups pancake mix
- 1 ½ cups buttermilk (or milk + lemon)
- 2 eggs
- 3 tbsp melted butter or oil
- Optional: 1 tsp vanilla
Fold gently, rest 8–10 minutes, cook on medium heat.
Keeping it safe and sensible
Because flour is a raw ingredient, it’s best not to taste raw batter. The FDA explains why raw flour matters here: flour is a raw food. CDC also reinforces the same idea in plain language: don’t eat raw dough or batter.
Blueberry Pancakes with Pancake Mix: How to Make Pancakes from the Mix Taste Homemade
Blueberry pancakes with pancake mix can be excellent. The difference between “boxy” pancakes and “why are these so good?” pancakes is usually just a few small choices.
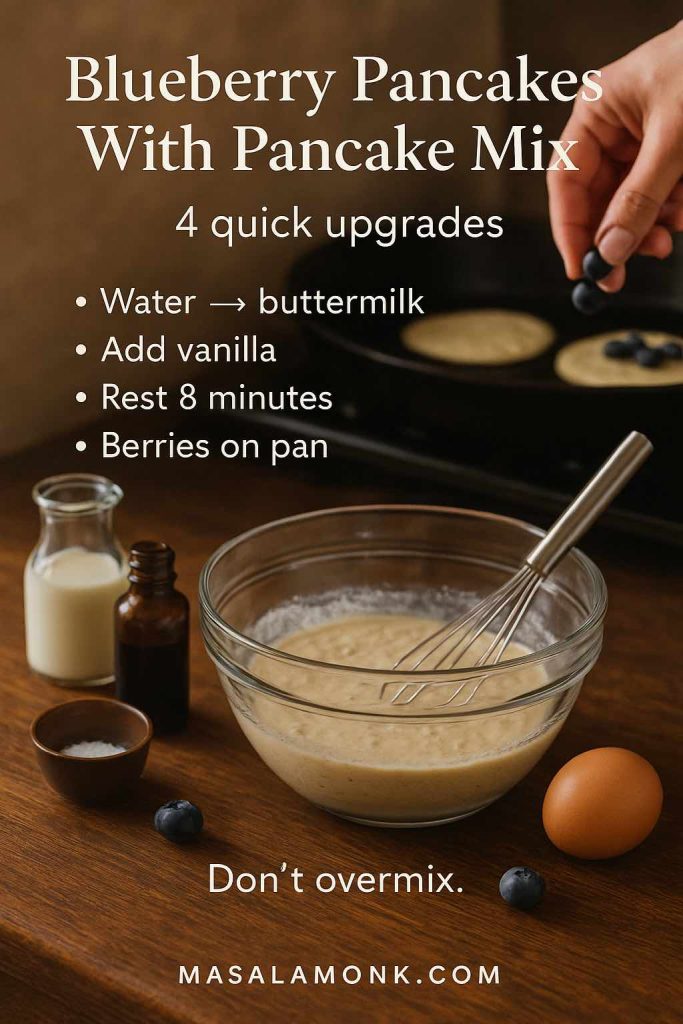
A simple upgrade approach
- Use buttermilk (or milk + lemon) instead of water.
- Add vanilla for warmth.
- Rest the batter briefly.
- Add blueberries on the pan, especially if using frozen berries.
Serious Eats tested mix upgrades thoroughly and shares what’s worth doing: how to make boxed pancake mix even better.
Blueberry pancake mix variations without a second recipe
Once you have the base pancake mix in a jar, you can steer it toward different styles:
- For a more hearty flavour, replace part of the flour with oat flour and you’re halfway to blueberry oat pancakes.
- For a lighter texture, add a tablespoon of cornstarch per batch.
- For a warm brunch vibe, add cinnamon and a pinch of nutmeg—especially good for banana blueberry pancake stacks.
Blueberry Mini Pancakes: Tiny, Quick, Freezer-Friendly
Blueberry mini pancakes feel playful, yet they’re also practical. They cook faster, they’re easy for kids, and they reheat beautifully. Additionally, they’re perfect for those mornings when you want pancakes and blueberries but don’t want to commit to a tall stack.

How to make blueberry mini pancakes
Use any batter above—classic, pancake mix, oat, protein, or gluten-free—then spoon 1 to 2 tablespoons per pancake onto a medium skillet. Sprinkle blueberries on top. Flip sooner than usual; mini pancakes set fast.
Turning them into frozen blueberry pancakes for busy mornings
Cool completely, freeze in a single layer on a tray, then transfer to a bag. Reheat in the toaster for crisp edges.

If you need a simple, reliable freezing and reheating guide, Better Homes & Gardens lays it out well: how to freeze and reheat pancakes. For broader freezer safety grounding, USDA has a clear overview: freezing and food safety.

Blueberry Dutch Pancake: The Big, Puffy Oven Version
A blueberry Dutch pancake is a different experience from classic blueberry pancakes: it’s puffed and dramatic, more custardy in the center, crisp at the edges, and made in one pan. It’s also a great choice when you want blueberries and pancakes but don’t want to stand at the stove flipping.
Ingredients (serves 2–3)
- 3 eggs
- ¾ cup milk
- ½ cup flour (or ⅓ cup pancake mix as a shortcut)
- Pinch of salt
- 1 tbsp sugar (optional)
- 2 tbsp butter for the pan
- ¾ cup blueberries

Method
- Preheat oven to 220°C / 425°F. Put a cast-iron skillet (or oven-safe pan) in the oven to heat.
- Blend or whisk eggs, milk, flour (or pancake mix), salt, and sugar until smooth.
- Carefully remove hot pan, add butter, swirl to coat.
- Pour in batter and scatter blueberries over the top.
- Bake 14–18 minutes until puffed and golden.
Serve immediately; Dutch pancakes deflate quickly, but that’s part of their charm.
Also Read: What to Mix with Jim Beam: Best Mixers & Easy Cocktails
Blueberry Maple Pancakes and Other Toppings That Make the Stack Sing
Sometimes the pancake is the main event; other times, toppings turn a good pancake into a “remember this breakfast” pancake. Blueberry maple pancakes are a classic direction—blueberries and maple simply belong together.
A few topping routes that feel natural
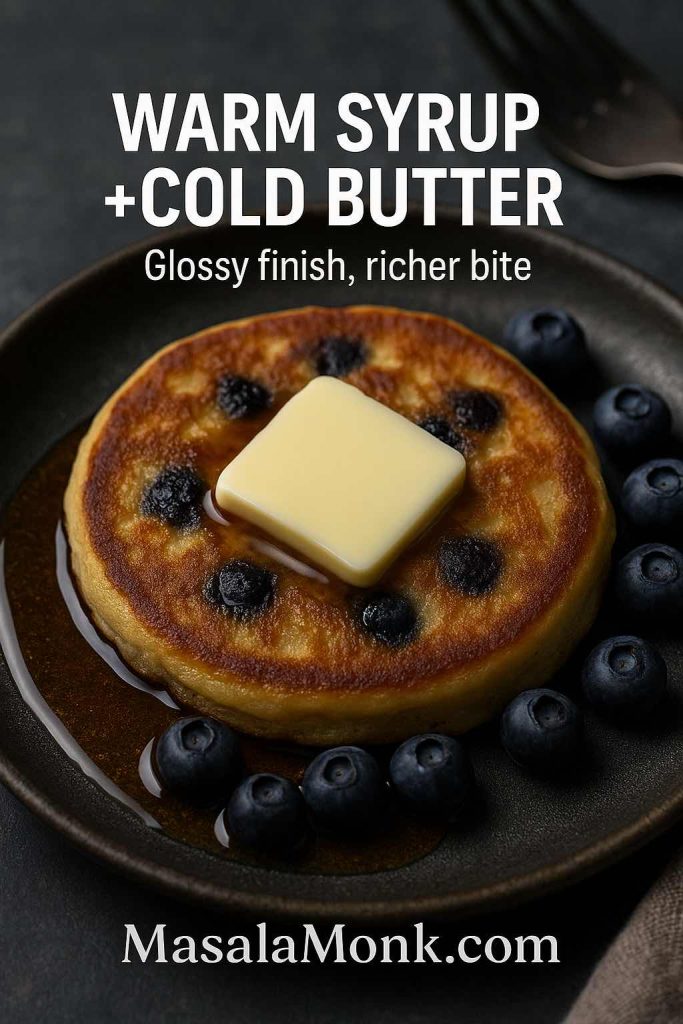
- Warm maple syrup and butter for that classic blueberry maple pancakes finish. If you’re curious about maple syrup from a nutrition standpoint, this is a thoughtful read: maple syrup vs sugar.
- Chocolate drizzle when you want dessert energy: 3-minute homemade chocolate syrup.
- Lemon curd for citrus-bright stacks: silky smooth lemon curd.
- A tart holiday-style topping that’s surprisingly good with blueberries: cranberry sauce with orange juice.
If you’d rather keep it ultra-simple, don’t underestimate fresh berries scattered on top. Sometimes blueberries and pancakes need no persuasion.
What to Serve with Blueberry Pancakes (So Breakfast Feels Complete)
A stack is wonderful on its own; nevertheless, adding one drink and one side can make breakfast feel like a proper moment.
Drinks that pair beautifully
- Cozy and familiar: homemade hot chocolate with cocoa powder.
- Fall-leaning brunch energy: healthy pumpkin spice latte.
- Bright and energizing for mornings when you want something lighter: matcha smoothie recipes with spinach.
- If you want blueberry flavours in your glass as well as your stack: blueberry morning drinks or this smoothie roundup that includes a blueberry cashew idea: nut-infused smoothies.
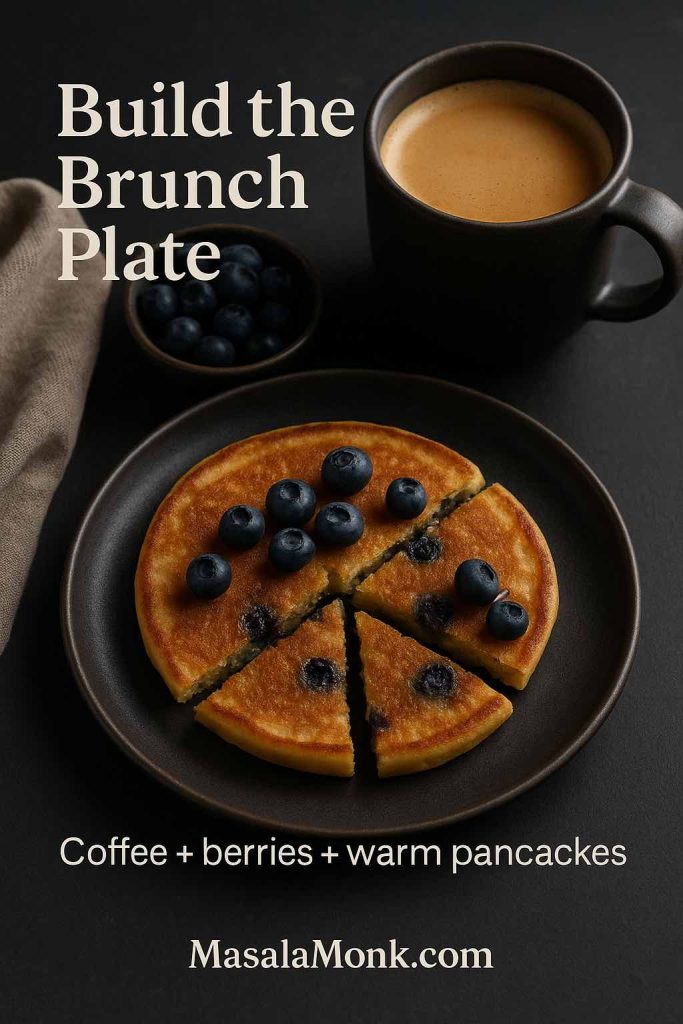
Sides that balance sweetness
- Crisp, salty contrast: how to cook bacon in the oven.
- Kid-friendly add-on that’s easy to bake or air fry: French toast sticks.
- Make-ahead option when you want breakfast ready tomorrow: high protein overnight oats.
A Few Final Details That Make Every Batch Better
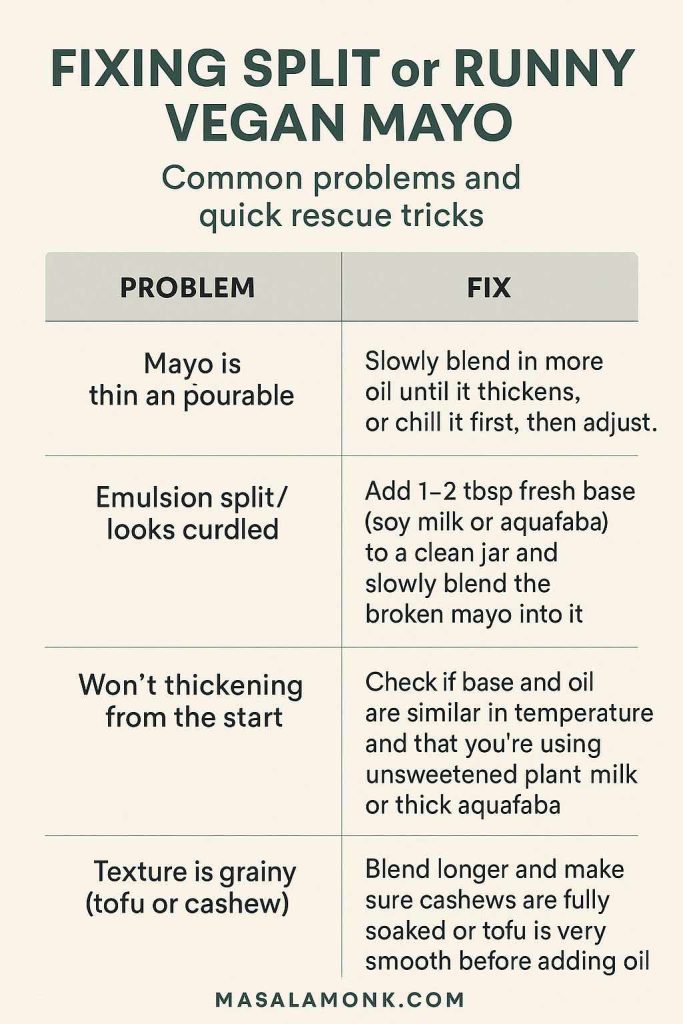
Even a great recipe can stumble if one small detail goes off. So before you close the tab and heat the pan, here are the most common friction points—plus the quick fixes that keep blueberry pancakes fluffy.
If pancakes turn dense
Mix less. Seriously. Fold until the flour disappears and stop. Also, let the batter rest so the flour hydrates. If you want the science behind the tenderness, Scientific American has a friendly explanation on gluten and pancakes: the science of gluten in pancakes.
If pancakes brown too fast
Lower the heat. Thick pancakes—especially blueberry ricotta hotcakes and high protein blueberry pancakes—need steadier, gentler heat than thin batters.
If your blueberries sink
Either your batter is thin or your berries went in too early. In either case, add berries per pancake on the skillet. It’s a small habit that pays off immediately.
If you’re cooking for later
Freeze properly so your frozen blueberry pancakes reheat with good texture. The Better Homes & Gardens guide is a great quick reference: how to freeze and reheat pancakes.
Also Read: Mayo Recipe: 15+ Homemade Mayonnaise Variations
FAQs
1) What makes blueberry pancakes turn out fluffy instead of flat?
Fluffy blueberry pancakes usually come from a thicker batter, minimal mixing, and cooking over steady medium heat. In addition, letting the batter rest briefly helps the texture set up so the pancakes rise rather than spread.
2) Can I use frozen blueberries for pancakes without the batter turning purple?
Yes. To avoid streaky batter, use frozen blueberries straight from the freezer and add them after you pour the batter onto the pan. That way, the berries warm inside the pancake instead of bleeding into the bowl.
3) Should I fold blueberries into the batter or add them on top?
For the most even distribution, add blueberries on top of each pancake right after ladling the batter. This method works for blueberries and pancakes in general, and it’s especially helpful for frozen blueberry pancakes.
4) Why do my blueberries sink to the bottom of the pancakes?
Most often, the batter is too thin or the berries were stirred in early. As a result, the berries drop before the pancake sets. A thicker batter and adding berries per pancake solves it.
5) How do I keep blueberry hotcakes from burning on the outside?
If blueberry hotcakes brown too quickly, the heat is likely too high. Instead, lower the heat slightly and give the pan time to stabilize before cooking the next batch.
6) What’s the best blueberry pancake batter consistency?
The batter should be thick enough to mound slightly when spooned, then slowly spread. If it pours like milk, the pancakes may end up thin; conversely, if it’s stiff like dough, they can turn dense.
7) How long should I rest blueberry pancake batter?
Generally, 8–15 minutes is enough. Meanwhile, preheat the pan and prep toppings. Longer rests can work too, yet over-resting may reduce lift as the leavening loses strength.
8) Can I make blueberry pancakes with pancake mix and still get a homemade taste?
Absolutely. Start by using milk (or buttermilk) instead of water, then let the batter rest briefly. Finally, add blueberries on the pan so the mix stays light and the berries stay distinct.
9) What is blueberry pancake mix, and is it different from regular pancake mix?
Blueberry pancake mix may refer to a plain mix used to make blueberry pancakes, or a mix that already includes blueberry flavouring. Either way, you can create a better “blueberry pancakes with pancake mix” result by adding real berries during cooking.
10) How do I make pancakes from the mix without ending up with rubbery texture?
Mix gently, avoid over-stirring, and don’t cook on high heat. Additionally, resting the batter for a few minutes helps the flour hydrate, which leads to softer pancakes.
11) How can I make a blueberry oatmeal pancake that isn’t heavy?
Soak oats briefly before cooking, and keep the batter from getting too thick. Also, cook on medium heat so the center sets without drying out the edges.
12) Are blueberry oat pancakes the same as blueberry oatmeal pancakes?
They’re closely related. Blueberry oat pancakes often use oat flour or blended oats, while a blueberry oatmeal pancake usually features rolled oats for texture. Either way, both pair well with blueberries.
13) How do I make banana and blueberry pancakes without them becoming dense?
Use one ripe banana rather than multiple bananas, and keep mixing minimal. Furthermore, if the batter feels too thick, add a small splash of milk to loosen it.
14) What’s the difference between blueberry pancakes and blueberry hotcakes?
Typically, “hotcakes” are thicker and sometimes slightly sweeter, while “pancakes” can range from thin to thick. However, most recipes can be adjusted either way by tweaking batter thickness and pan temperature.
15) How do I make blueberry mini pancakes that cook evenly?
Use smaller portions of batter and keep the heat moderate. Then, add blueberries to each mini pancake before flipping so they don’t scatter in the pan.
16) Can I freeze blueberry pancakes for later?
Yes. Cool them fully, freeze in a single layer first, then store in a bag. Afterward, reheat in a toaster or oven for the best texture.
17) How do I reheat frozen blueberry pancakes so they don’t get soggy?
To avoid sogginess, reheat in a toaster or oven rather than microwaving. If you must microwave, use short bursts and finish briefly in a pan to restore texture.
18) How do I make high protein blueberry pancakes that still taste good?
Choose protein sources that add tenderness—like Greek yogurt or cottage cheese—rather than relying only on protein powder. Also, keep the batter moist and cook at a slightly lower heat.
19) Are blueberry protein pancakes and blueberry pancakes protein searches basically the same thing?
Yes—both phrases generally refer to pancakes designed to be higher in protein. Accordingly, the best recipes emphasize both nutrition and a fluffy, pleasant bite.
20) How do blueberry cottage cheese pancakes taste compared to classic pancakes?
They’re usually a bit creamier and more filling, with a tender interior. Moreover, they can be either smooth or lightly textured depending on whether you blend the batter.
21) What are blueberry ricotta hotcakes, and how are they different?
Blueberry ricotta hotcakes are thicker, softer pancakes enriched with ricotta. Consequently, they tend to feel more “brunch-style,” with a rich, delicate crumb.
22) Can I make blueberry and ricotta pancakes without separating eggs?
Yes. You can whisk ricotta into the wet ingredients and proceed normally. Still, separating eggs and folding in whipped whites often creates a lighter hotcake texture.
23) How do I make blueberry lemon pancake flavour stand out without making it sour?
Prioritize lemon zest for aroma and use lemon juice sparingly. Then, balance the brightness with a touch of sweetness and plenty of blueberries.
24) What are blueberry lemon ricotta pancakes, and why are they popular?
They combine berry sweetness, citrus fragrance, and creamy ricotta richness. As a result, they deliver a layered flavour that feels special while staying easy to cook.
25) Can I make blueberry pancakes gluten free without them crumbling?
Yes. Use a reliable gluten-free flour blend, let the batter rest longer, and avoid flipping too early. Additionally, cooking on medium-low heat helps the structure set before turning.
26) Are almond flour blueberry pancakes naturally gluten free?
They can be, since almond flour doesn’t contain gluten. Nevertheless, almond flour often benefits from extra eggs or a small amount of gluten-free blend to improve structure.
27) What’s the best way to keep blueberries from bursting too much?
Add blueberries on the pan rather than mixing aggressively, and avoid pressing them into the batter. Also, cook on moderate heat so the berries warm gently instead of exploding quickly.
28) Why do some “best blueberry pancake” recipes recommend buttermilk?
Buttermilk adds acidity that reacts with baking soda, which improves rise and tenderness. In turn, it creates a softer crumb and a pleasant tang that complements blueberries.
29) Can I make blueberry pancakes ahead for brunch guests?
Definitely. Make a large batch, keep them warm in a low oven, and serve in stacks. Meanwhile, you can cook bacon, prep toppings, or mix up drinks without rushing.
30) What’s a blueberry dutch pancake, and can I use blueberries in it?
A blueberry dutch pancake is an oven-baked, puffy pancake with crisp edges and a custardy center. Yes, blueberries work beautifully—scatter them over the batter before baking for a dramatic, fruit-studded result.