A moscow mule recipe can look almost too easy to be memorable: vodka, lime, ginger fizz, ice. And yet, when it’s built well, it tastes like clarity—cold, bright, and sharply refreshing, with ginger heat that arrives just after the sip. Still, because it’s so simple, it can also fall apart fast. If the lime is dull, the ginger is warm, or the ice is stingy, the whole thing turns flat or sweet or watery. Fortunately, once you understand the structure behind a dependable moscow mule recipe, you can make it confidently, adjust it on the fly, and branch into variations without learning a new cocktail every time.
This guide gives you one master formula first. Then, step by step, it takes you through the versions people keep coming back to at home: Mexican Mule, Kentucky Mule, Irish Mule, Gin Mule, Italian Mule, Cranberry Moscow Mule, Apple Mule, a Ginger-forward Mule, and a Tropical Mule with coconut water that feels especially at home on MasalaMonk. Along the way, you’ll also learn what to do when you only have ginger ale, how to make a Moscow Mule without ginger beer, how to build a quick make-ahead base, and how to serve a crowd without losing fizz.
For classic reference points, the backbone of this drink shows up consistently across trusted cocktail sources such as Serious Eats’ Moscow Mule and Liquor.com’s Moscow Mule cocktail recipe. However, the most useful thing isn’t memorizing any single set of numbers. Instead, it’s learning the “why” behind the balance so the drink works with the ginger fizz you have, the bottle you have, and the mood you’re in.
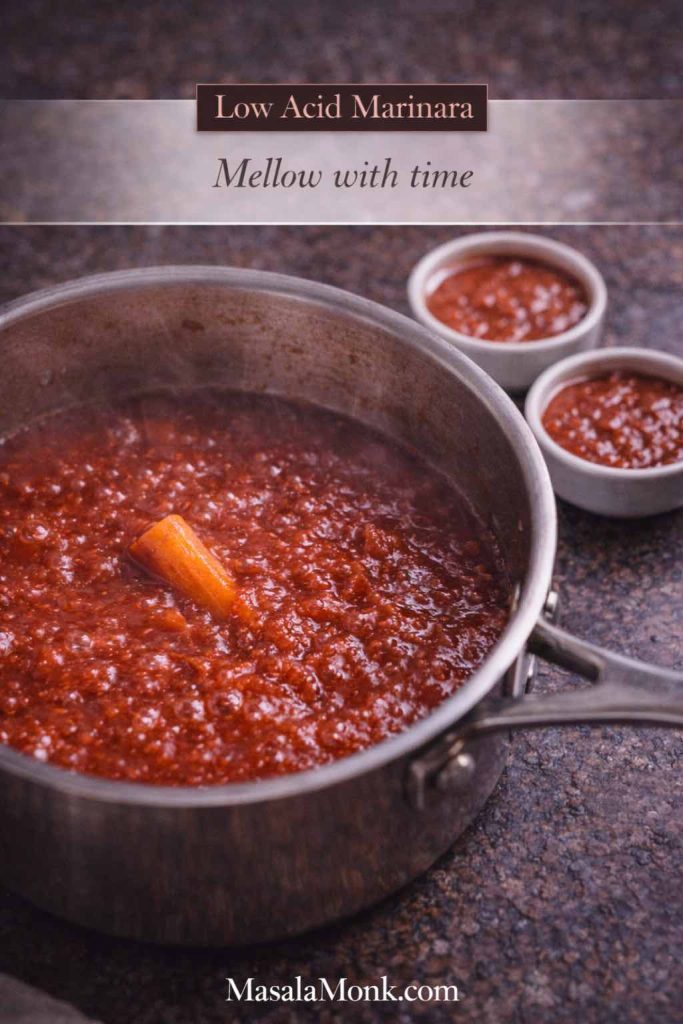
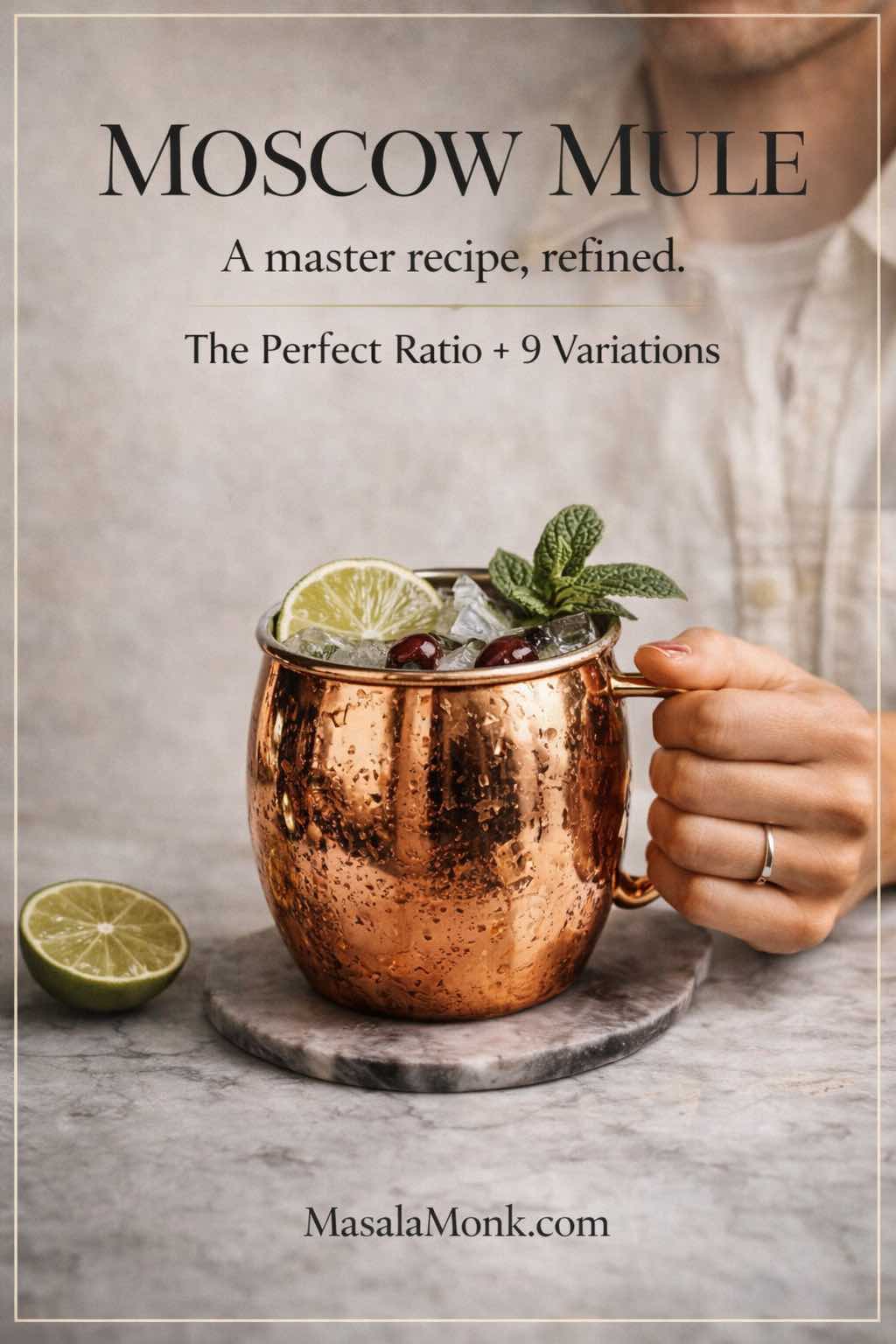
Moscow mule recipe: the master ratio that makes everything easy
Before measurements, think in parts. A reliable moscow mule recipe is simply a long, fizzy highball built from four ideas:
- a clean spirit foundation
- a bright citrus snap
- a spicy ginger lift
- a cold temperature and controlled dilution
So, the master ratio is:
- 1 part vodka
- ½ part fresh lime
- 2–3 parts ginger beer
- a lot of ice
Because ginger beers vary wildly in sweetness and spice, that 2–3 parts range matters. Consequently, you’re not “failing the recipe” if you pour a little more or less—rather, you’re tailoring it to the fizz in your fridge.
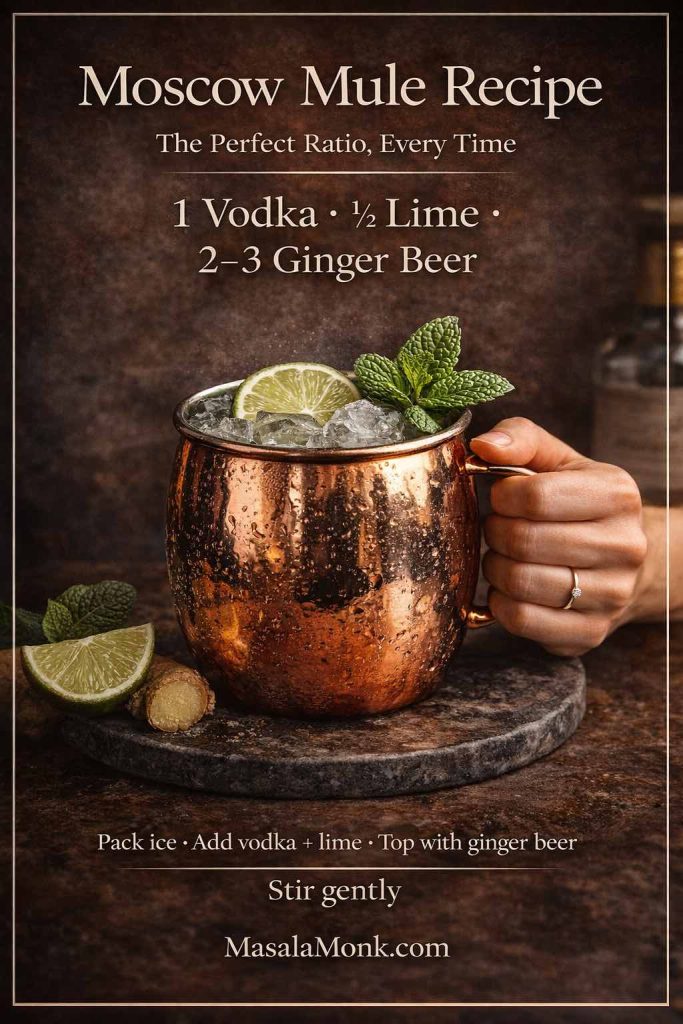
Moscow mule recipe (single-serve master build)
Ingredients
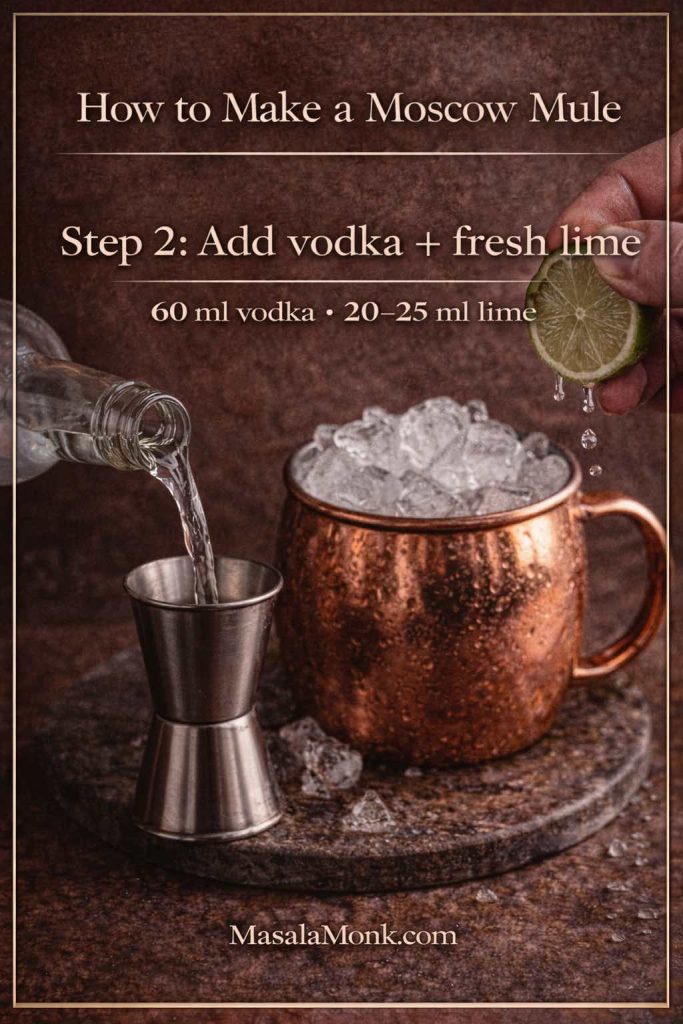
- 60 ml vodka
- 20–25 ml fresh lime juice
- 120–180 ml chilled ginger beer
- plenty of ice
- lime wheel or wedge (mint optional)
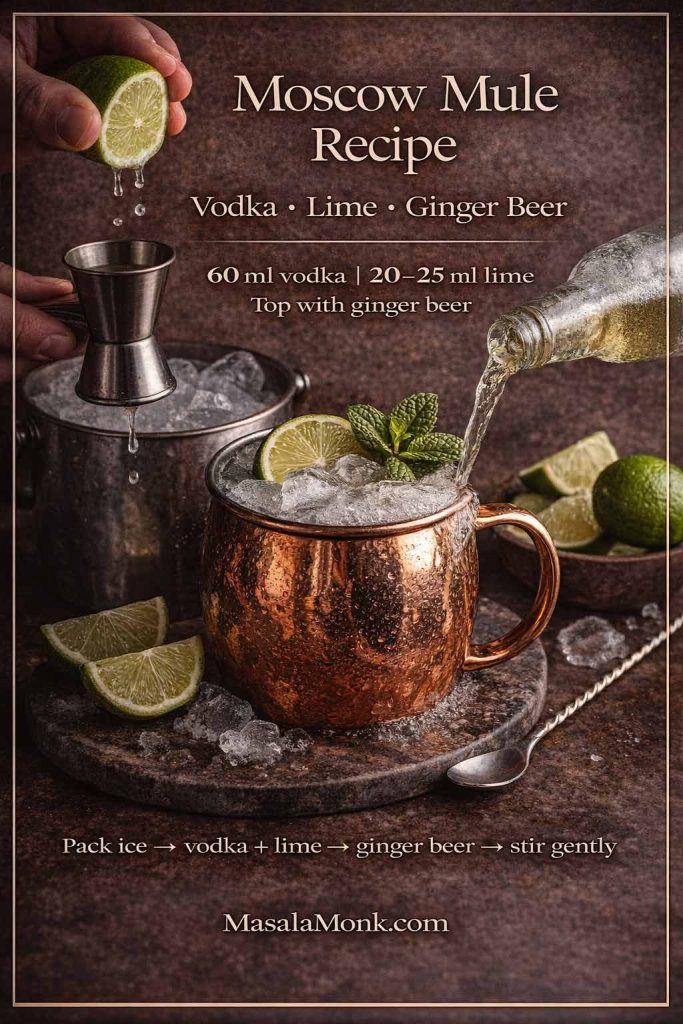
Method
- Chill your mug or glass briefly if possible; even a few minutes helps.
- Fill it completely with ice.
- Add vodka and lime juice.
- Top with cold ginger beer.
- Stir gently once or twice—just enough to combine.
- Garnish and serve immediately.
That’s the core moscow mule recipe, and it’s the one you’ll return to. From here, everything is just a variation on the same theme.
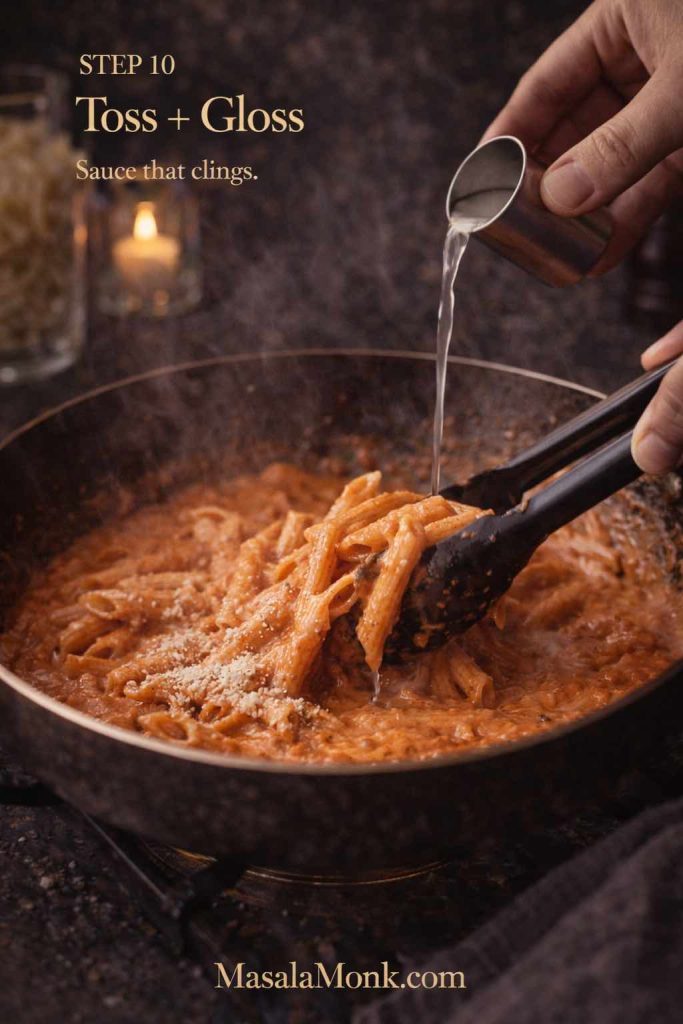
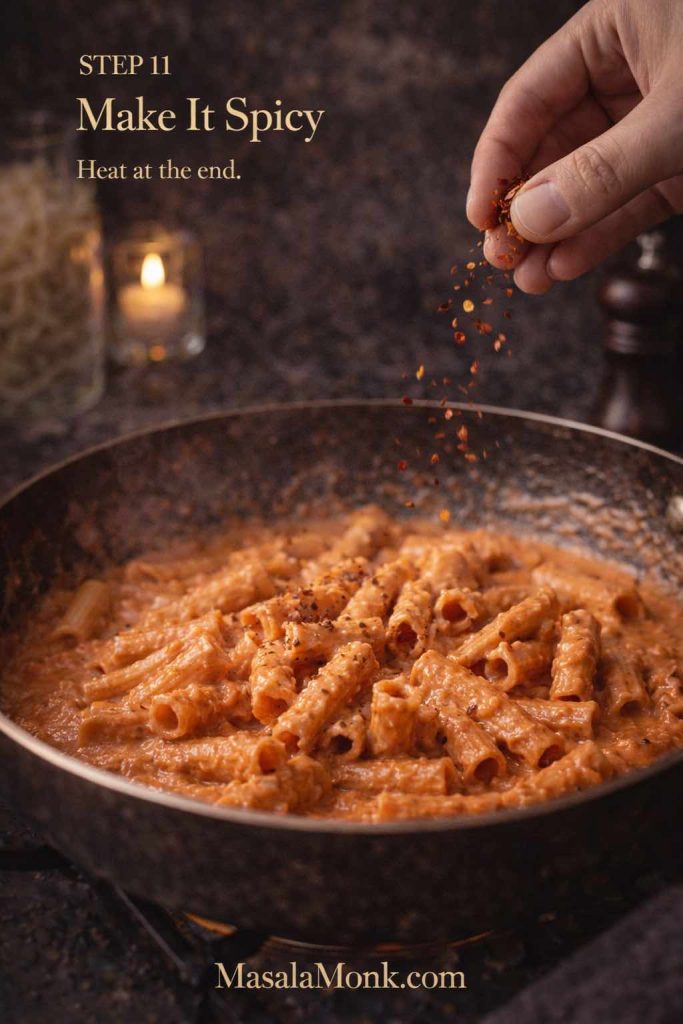
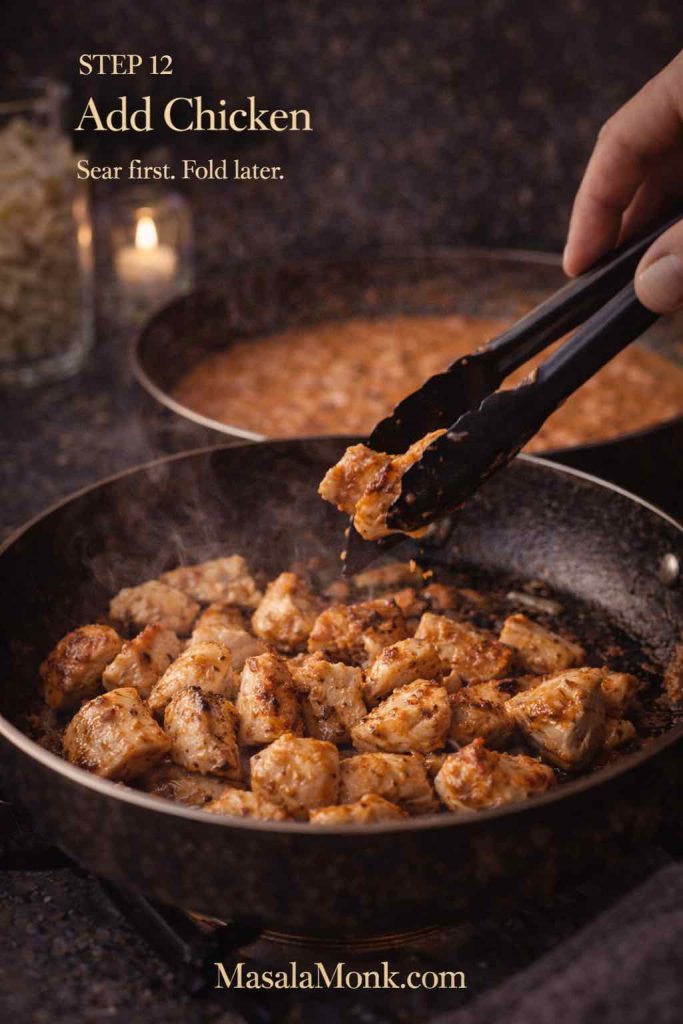
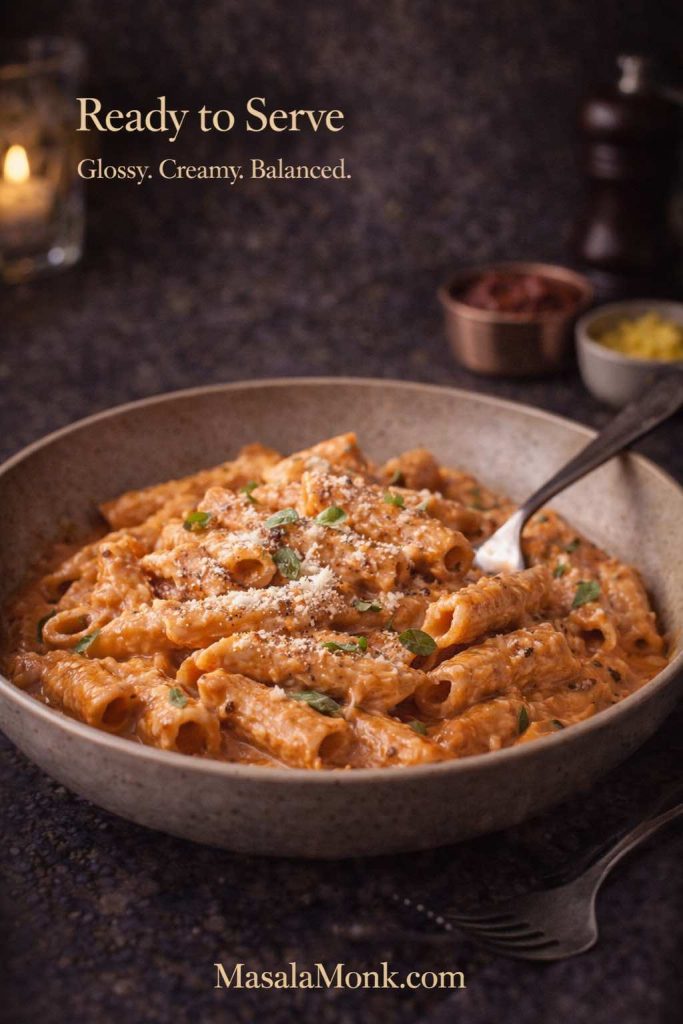
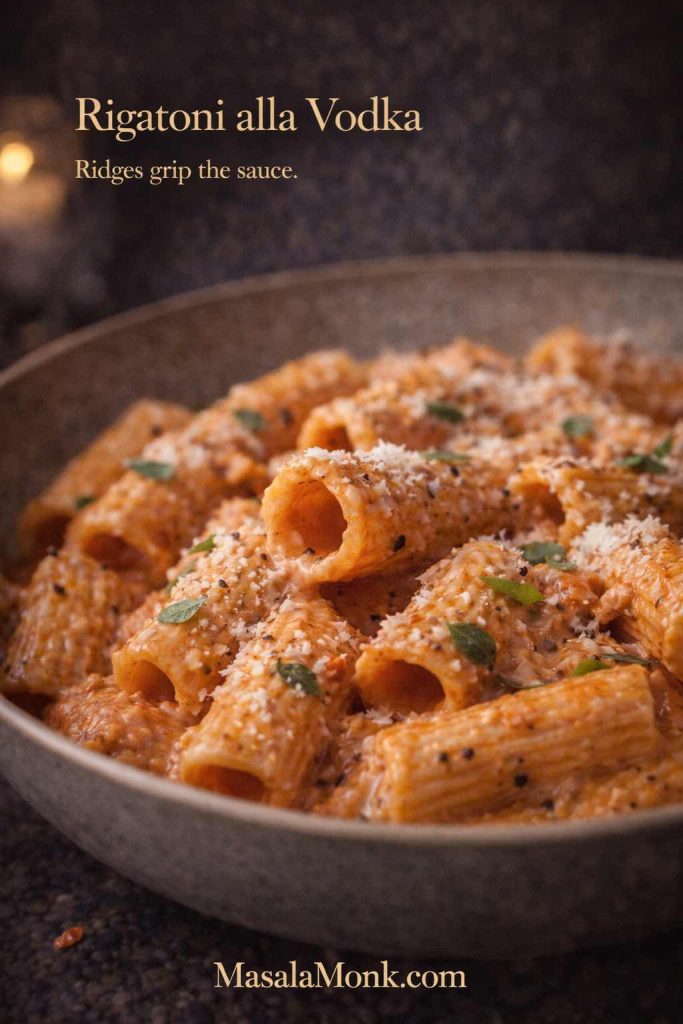
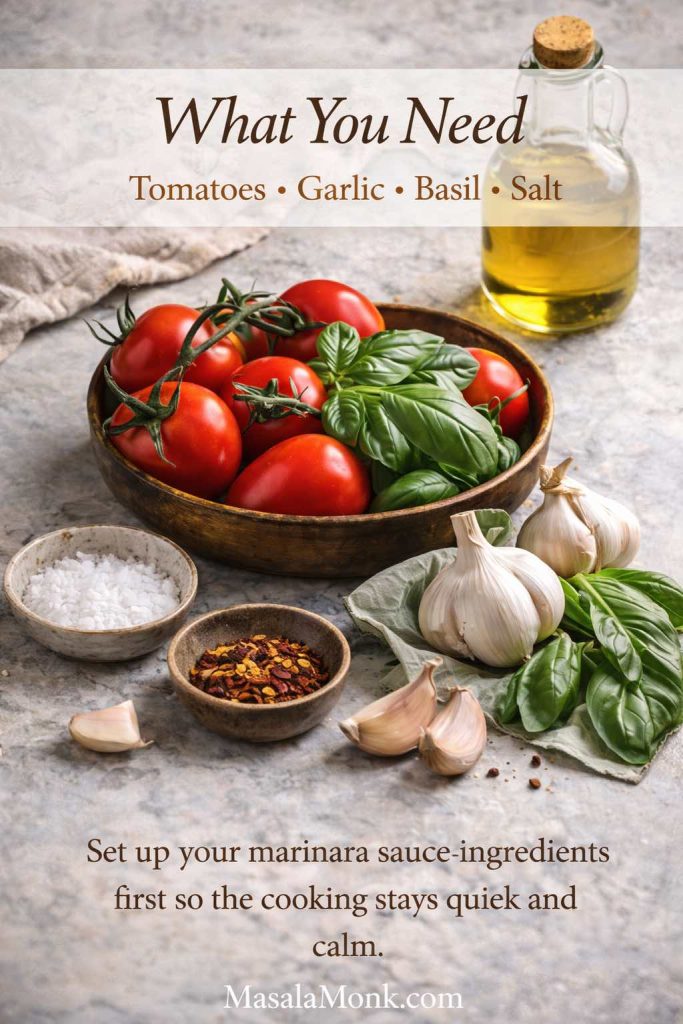
Also Read: Vodka Pasta (Penne alla Vodka) + Spicy Rigatoni, Chicken, and Gigi Recipes
Moscow mule ingredients: the few details that change the whole drink
Because the ingredient list is short, each piece has an oversized role. Therefore, small upgrades matter more here than they do in a complicated cocktail.
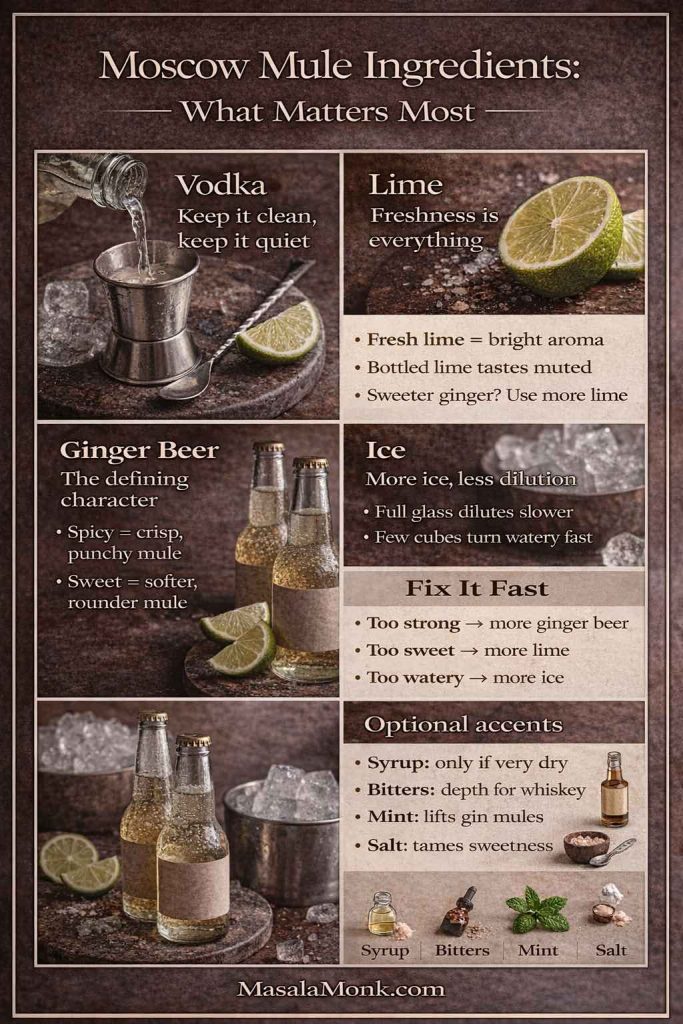
Vodka: keep it clean, keep it quiet
In a classic moscow mule recipe, vodka is the support beam, not the decoration. It should taste neutral enough that ginger and lime stay in front. That said, you don’t need a luxury bottle. Instead, choose a vodka you find reasonably smooth in a simple soda-and-lime.
If your vodka tastes sharp, you can still make a great Mule. However, you’ll likely prefer:
- slightly more ginger beer to lengthen the drink
- slightly more lime to brighten the finish
- plenty of ice to keep the alcohol from feeling loud
Lime: freshness is everything
Fresh lime gives both acidity and aroma. Meanwhile, bottled lime can taste muted or “cooked,” which makes the drink feel less alive. If you only upgrade one thing in your moscow mule recipe, make it fresh lime.
Also, lime quantity isn’t fixed in stone. If your ginger beer is sweeter, you can use more lime. Conversely, if your ginger beer is very dry and spicy, you may prefer slightly less lime so the drink doesn’t feel sharp.
Ginger beer: the defining character
Ginger beer is the “spark” that makes this drink feel special. Moreover, different ginger beers produce noticeably different Mules:
- spicy, peppery ginger beer → crisp, punchy Mule
- sweet, mild ginger beer → softer, rounder Mule
- very carbonated ginger beer → bright and lively, with more lift
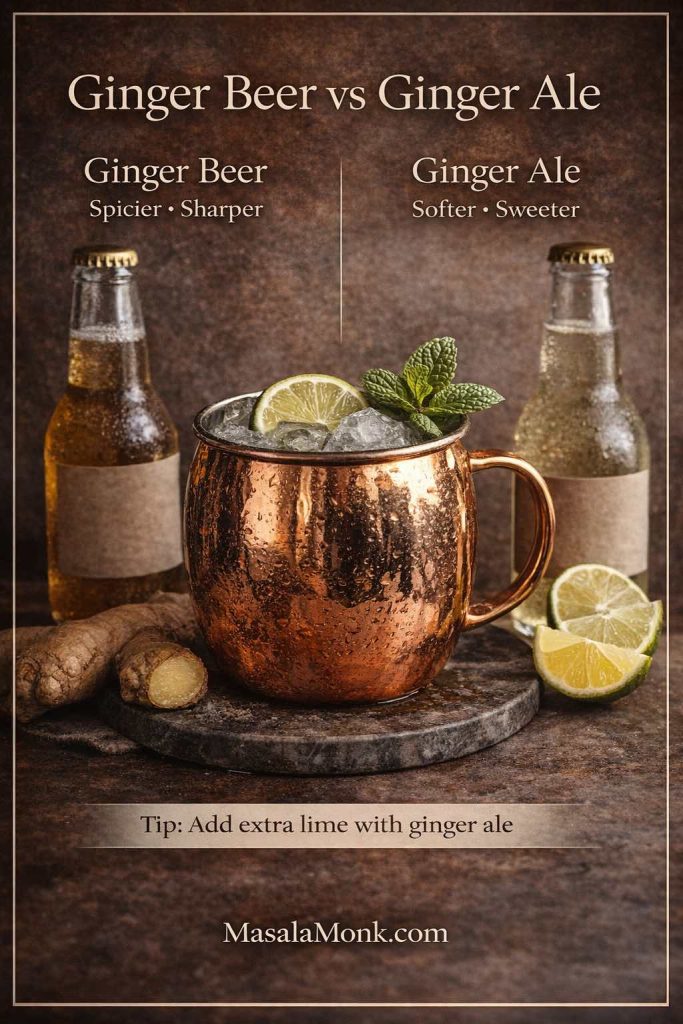
If you’re curious about how ginger beer differs from ginger ale in practical terms, this quick explainer is useful: ginger beer vs. ginger ale. The short version is that ginger ale is often sweeter and gentler, while ginger beer tends to be bolder and more ginger-forward.
Ice: more ice usually means less dilution
It sounds backwards, yet it’s true: a glass packed with ice often dilutes more slowly than a glass with a few cubes. Consequently, a Mule built with “a mountain of ice” stays balanced longer. On the other hand, a Mule built with minimal ice warms fast and becomes watery.
Optional accents: only when they solve a specific problem
A Mule doesn’t need much else. Still, these small accents can help:
- Simple syrup (tiny amount): only if your ginger beer is extremely dry and you want a rounder sip
- Aromatic bitters: especially helpful in bourbon or whiskey versions for depth
- Mint: adds aroma and freshness, especially in gin mules
- A pinch of salt: surprisingly useful when your ginger fizz makes the drink taste too sweet
If you enjoy the ginger side of this drink beyond cocktails, you might also like MasalaMonk’s ingredient-focused read: Ginger And Its Stunning Health Benefits. It’s not a cocktail guide, but it does deepen appreciation for ginger’s role in drinks.
Also Read: French 75 Cocktail Recipe: 7 Easy Variations
How to make a Moscow mule recipe that stays crisp to the last sip
A Mule’s charm is how quickly it comes together. Nevertheless, a few habits separate a bright, snappy drink from a flat one.
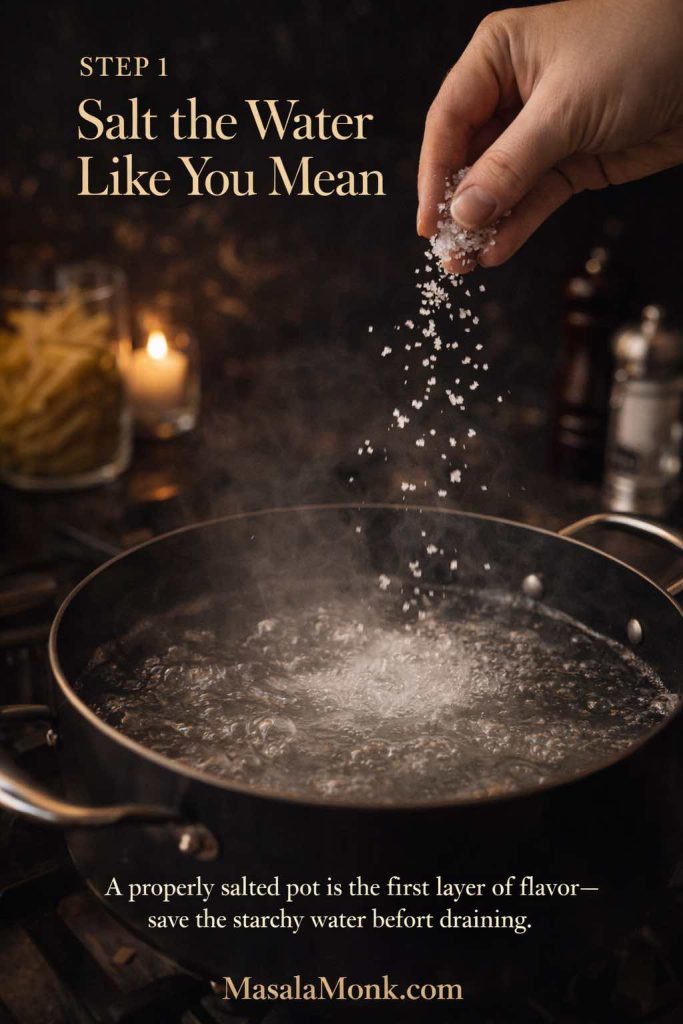
Step 1: Chill what you can, because temperature matters
If the ginger beer is cold, carbonation feels sharper. If it’s warm, the drink tastes softer and flatter. So, chill your ginger beer and chill your glass when possible.
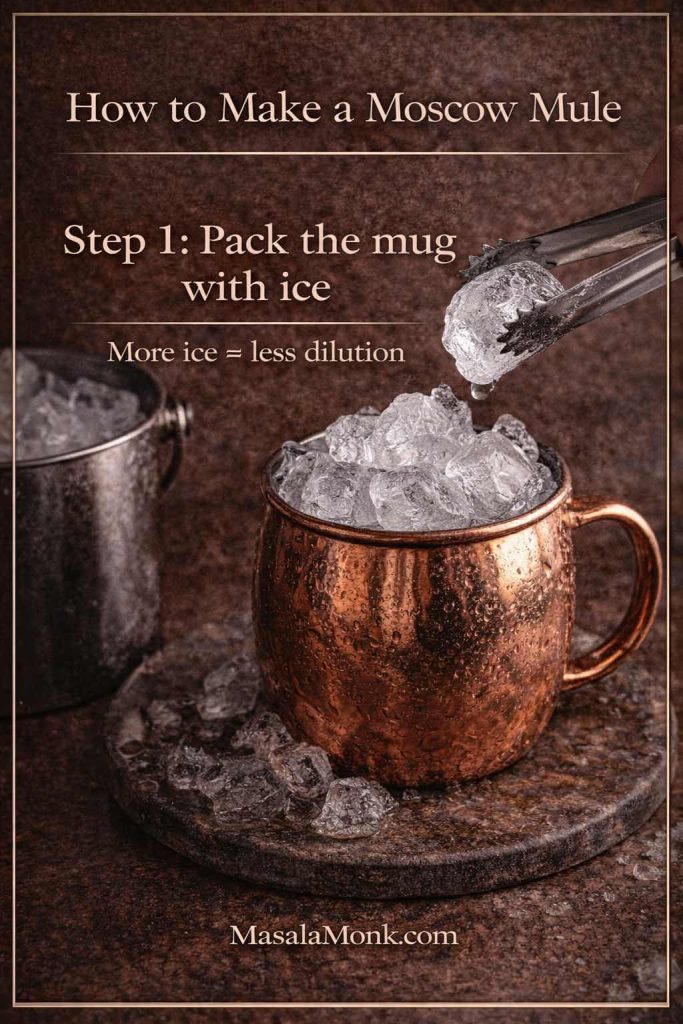
Step 2: Pack the ice, then build quickly
A packed ice bed keeps everything cold. Moreover, it slows down dilution. Build the drink swiftly so the ice doesn’t melt while you’re hunting for garnish.
Step 3: Add ginger beer last, then stir gently
Because ginger beer is carbonated, it loses sparkle when it’s shaken or stirred aggressively. Therefore, stir just once or twice, gently.
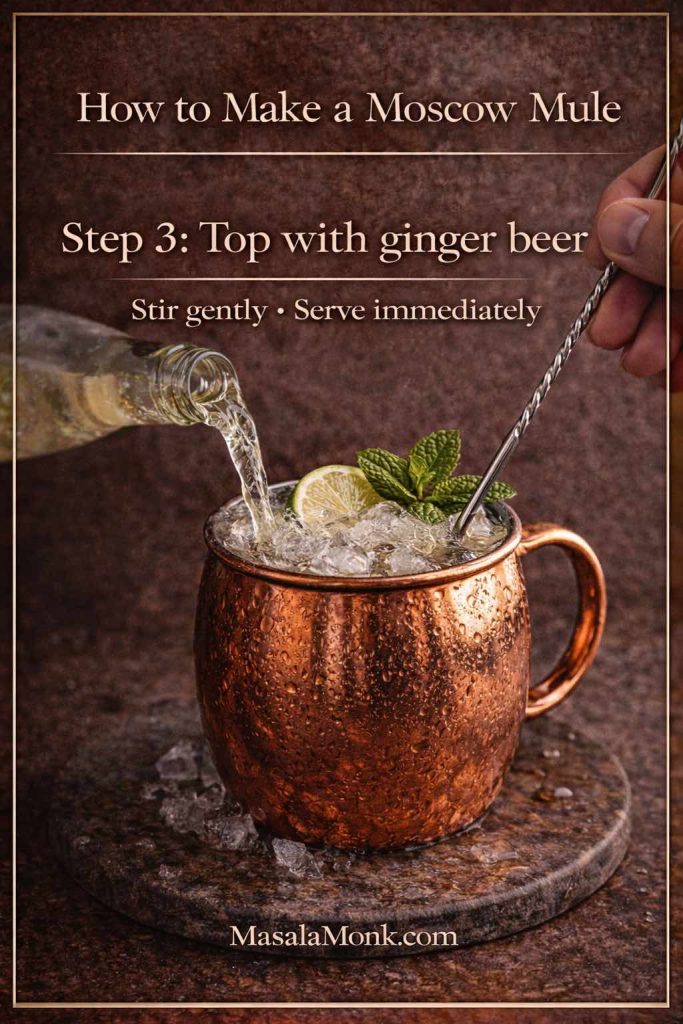
This is why the classic method in sources like Liquor.com’s Moscow Mule and Serious Eats’ Moscow Mule keeps things simple: build in the glass, top with ginger beer, and don’t overwork it.
Also Read: Negroni Recipe: Classic Cocktail & Its Variation Drinks
Moscow mule recipe with ginger beer vs ginger ale: how to balance either one
Sometimes you have ginger beer. Sometimes you have ginger ale. Either way, you can make a refreshing drink. Still, because the sweetness and spice differ, the balancing approach changes.
When ginger beer is spicy and dry
In that case, the moscow mule recipe can stay very clean:
- vodka at 60 ml
- lime around 20–25 ml
- ginger beer to lengthen as you like
Because the ginger has bite, the drink tastes lively even without extra tricks.
When ginger beer is sweet and mild
Then you’ll often want:
- slightly more lime
- slightly less ginger beer at first
- no additional sugar
Otherwise, the drink can drift into soda territory.
Moscow mule recipe with ginger ale (the version that still tastes “right”)
Ginger ale tends to be milder and sweeter. Consequently, the best approach is to push brightness and keep sugar out.
Try this structure:
- 60 ml vodka
- 25–30 ml lime juice
- chilled ginger ale to top
- plenty of ice
If it tastes too sweet, you have two easy levers:
- increase lime slightly
- add a tiny pinch of salt (it doesn’t taste salty; it tastes more balanced)
For a non-alcoholic detour with similar “fizz + fruit + citrus” logic, MasalaMonk’s Apple Juice Mocktails are a great companion. Even though those drinks aren’t Mules, the balancing instincts are surprisingly transferable.
Moscow mule recipe without ginger beer (still bright, still refreshing)
If you don’t have ginger beer and you don’t want to rely only on ginger ale, you can still build something close to the Mule experience.
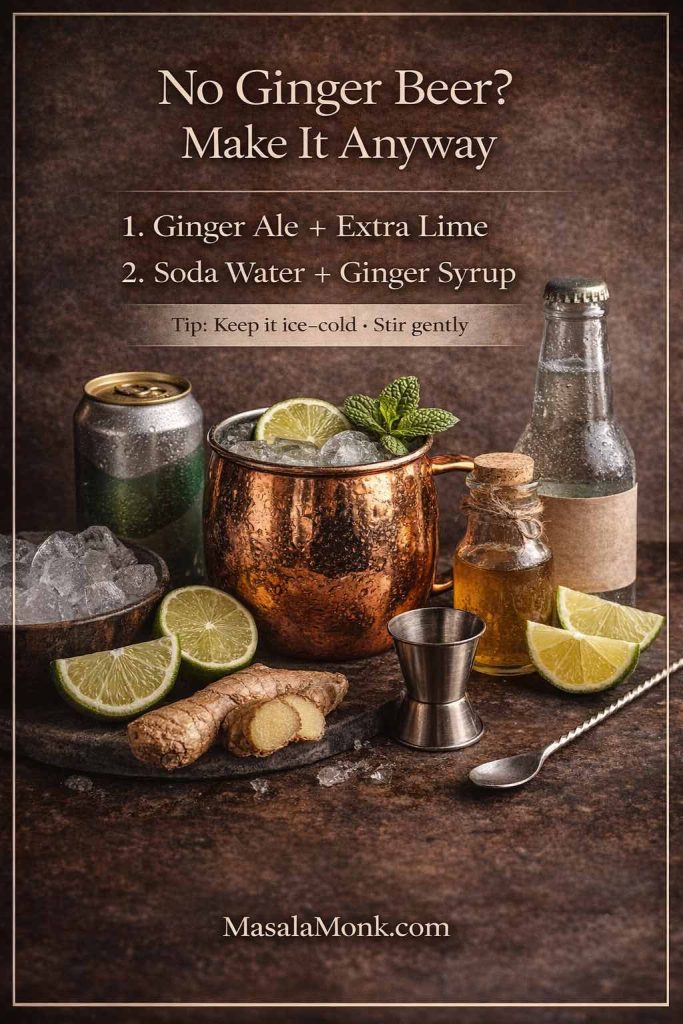
Approach A: Ginger ale + fresh ginger boost
Build vodka + lime over ice, top with ginger ale, then add:
- a thin slice of fresh ginger, lightly muddled, or
- a small splash of ginger syrup
Because fresh ginger adds bite, the drink feels more Mule-like.
Approach B: Soda water + lime + ginger syrup
This becomes a ginger-lime highball. It’s not identical to the classic moscow mule recipe, yet it delivers the same cold, zippy satisfaction.
Either way, chill everything and keep the stir gentle.
Also Read: 10 Best Espresso Martini Recipe Variations (Bar-Tested)
Moscow mule recipe adjustments: fix the drink in the glass
Even a good moscow mule recipe can taste “off” because ginger fizz varies, limes vary, and ice varies. Fortunately, you can fix most issues fast.
If it tastes too sweet
First, add more lime. Then, if it still feels candy-like, add a tiny pinch of salt. Next time, choose a spicier ginger beer or start with a smaller pour and top up slowly.
If it tastes too strong
Instead of adding more ice, add more ginger beer. That lengthens the drink while keeping it lively. Meanwhile, keep lime steady so it stays bright.
If it tastes flat
Usually, one of these happened:
- the ginger fizz wasn’t cold
- the bottle was opened long ago
- the drink was stirred too hard
- the drink sat too long before serving
Next time, chill harder and add ginger beer at the last second.
If it tastes watery
This is almost always an ice problem. Use more ice and build quickly. Also, don’t let the drink sit around before it’s served.
Also Read: Whiskey Sour Recipe: Classic Cocktail, Best Whiskey & Easy Twists
Moscow mule recipe variations: one template, many personalities
The Mule works because it’s a template: spirit + lime + ginger fizz. Consequently, swapping the spirit changes the character without requiring new technique. That “template” idea is reflected even in mainstream recipe sources like Epicurious’ Moscow Mule, which notes how naturally it spins into different versions.
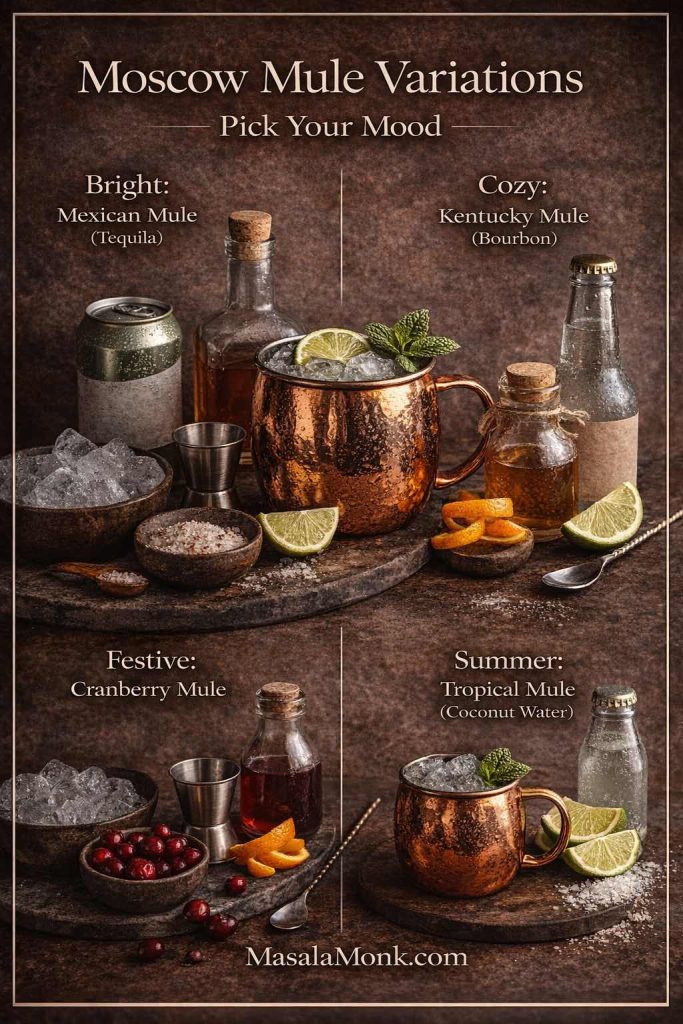
Below are the variations that truly earn their place. Each one starts from the same master build, then shifts one major element.
Mexican mule recipe: tequila mule with bright, bold energy
A Mexican Mule is often the first variation people fall for, because tequila and ginger are natural friends. Moreover, tequila’s agave character makes the drink feel sunny and lively.
For a classic reference, see Difford’s Mexican Mule.
Mexican mule recipe (classic build)
- 60 ml tequila (blanco for crispness, reposado for warmth)
- 20–25 ml lime
- ginger beer to top (chilled)
- optional: a small spoon of syrup if your ginger beer is very dry
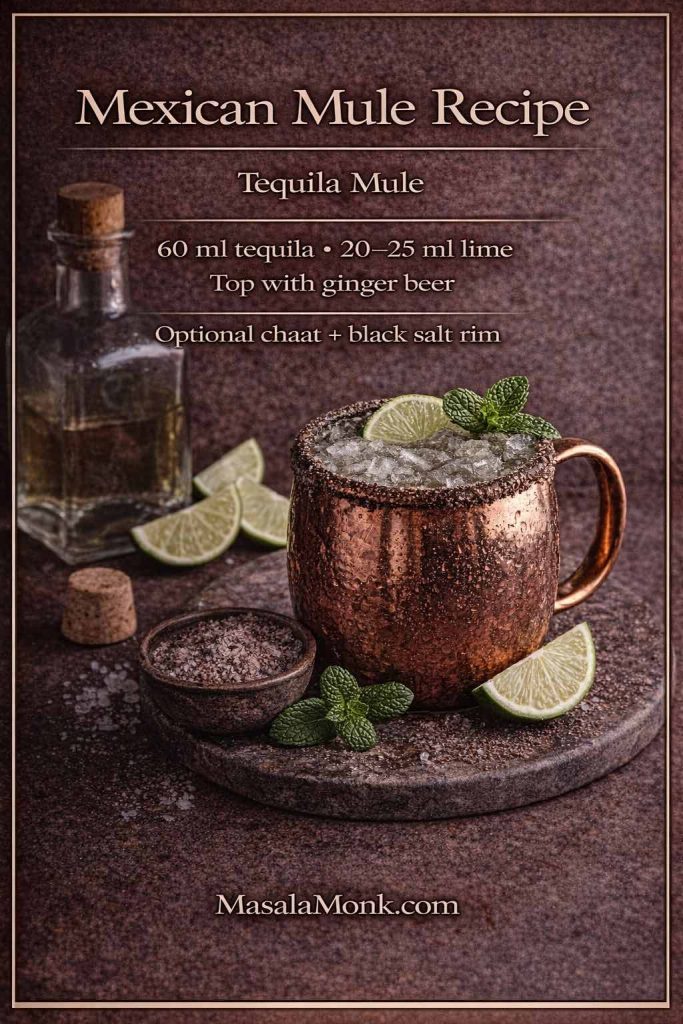
A MasalaMonk-style twist: a chaat rim that makes sense
Instead of treating garnish like decoration, use it like seasoning. Rim half the glass with:
- a pinch of chaat masala
- a pinch of black salt
Suddenly, the drink feels like it belongs next to street snacks. Consequently, the Mexican mule recipe becomes more than a cocktail; it becomes a pairing.
If you want an easy, satisfying snack partner, Homemade French Fries are an obvious win—especially with a chili-lime dust. Meanwhile, for something herby and tangy, Falafel with Indian twists fits beautifully.
Kentucky mule recipe: bourbon mule that’s warm, spicy, and comforting
A Kentucky Mule takes the moscow mule recipe structure and makes it richer. Bourbon brings vanilla and caramel notes; ginger keeps the finish snappy. Therefore, it feels cozy without becoming heavy.
For a whiskey-mixer perspective that aligns with this logic, MasalaMonk’s What to Mix with Jim Beam is a helpful companion.
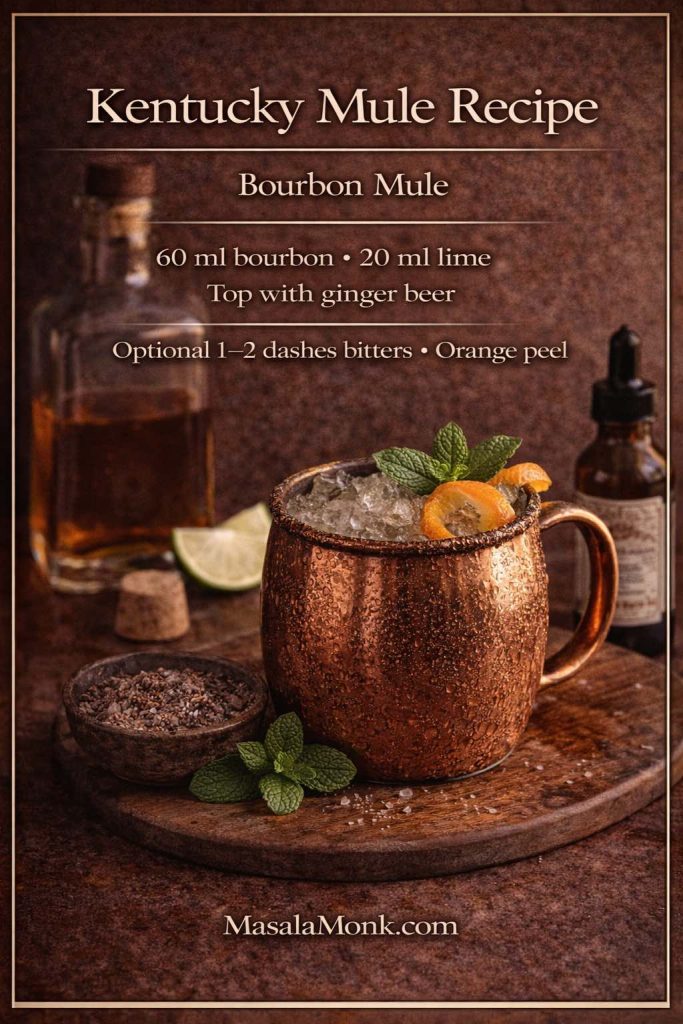
Kentucky mule recipe (easy build)
- 60 ml bourbon
- 20 ml lime
- ginger beer to top
- optional: 1–2 dashes aromatic bitters
- garnish: lime or orange peel
A small shift that makes it feel “bar-quality”
Instead of changing ingredients, change emphasis:
- choose a spicier ginger beer
- keep lime slightly lower if your bourbon is delicate
- add bitters if you want depth without sugar
As a result, the drink tastes layered rather than sweet.
Also Read: Daiquiri Recipe (Classic, Strawberry & Frozen Cocktails)
Irish mule recipe: smooth, bright, and quietly addictive
An Irish Mule often feels gentler than a bourbon version, because Irish whiskey can be lighter and less oaky. Consequently, ginger and lime remain front and center.
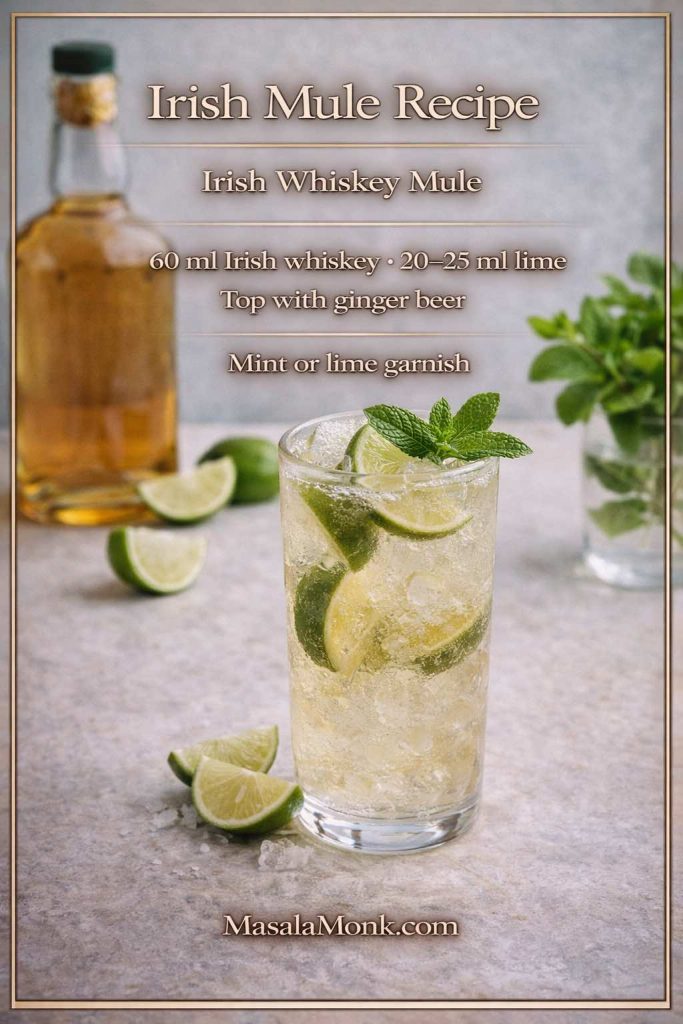
Irish mule recipe (simple build)
- 60 ml Irish whiskey
- 20–25 ml lime
- ginger beer to top
- garnish: mint or lime
Because this version is so approachable, it works well as a “welcome drink” when friends arrive. Meanwhile, if you want it even fresher, mint adds aroma without changing the structure.
Also Read: Simple Bloody Mary Recipe – Classic, Bloody Maria, Virgin & More
Gin mule recipe: botanical freshness with ginger lift
Gin changes the Mule’s personality immediately. Instead of “clean and crisp,” the drink becomes aromatic and herbal. Moreover, cucumber and mint fit naturally.
A closely related drink, the Gin-Gin Mule, leans into mint; see The Spruce Eats’ Gin-Gin Mule for a reference build.
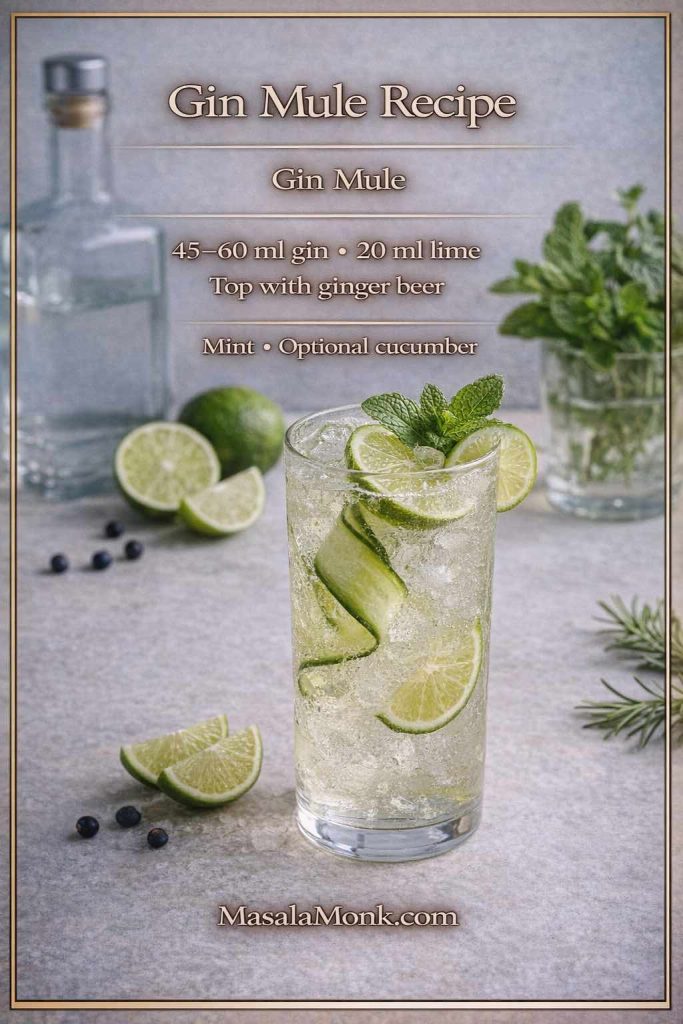
Gin mule recipe (everyday build)
- 45–60 ml gin
- 20 ml lime
- ginger beer to top
- mint garnish
- optional: cucumber slice
Because gin mules feel lighter, they pair especially well with tangy, herby foods. Therefore, Falafel with Indian twists makes a lot of sense here, particularly if you serve it with a bright sauce.
Also Read: Bolognese Sauce Recipe: Real Ragù & Easy Spag Bol
Italian mule recipe: aperitivo bitterness meets ginger fizz
An Italian Mule adds gentle bitterness—often through Aperol or a light amaro. As a result, the drink tastes more layered and “menu-worthy,” even though it’s just as easy to build.
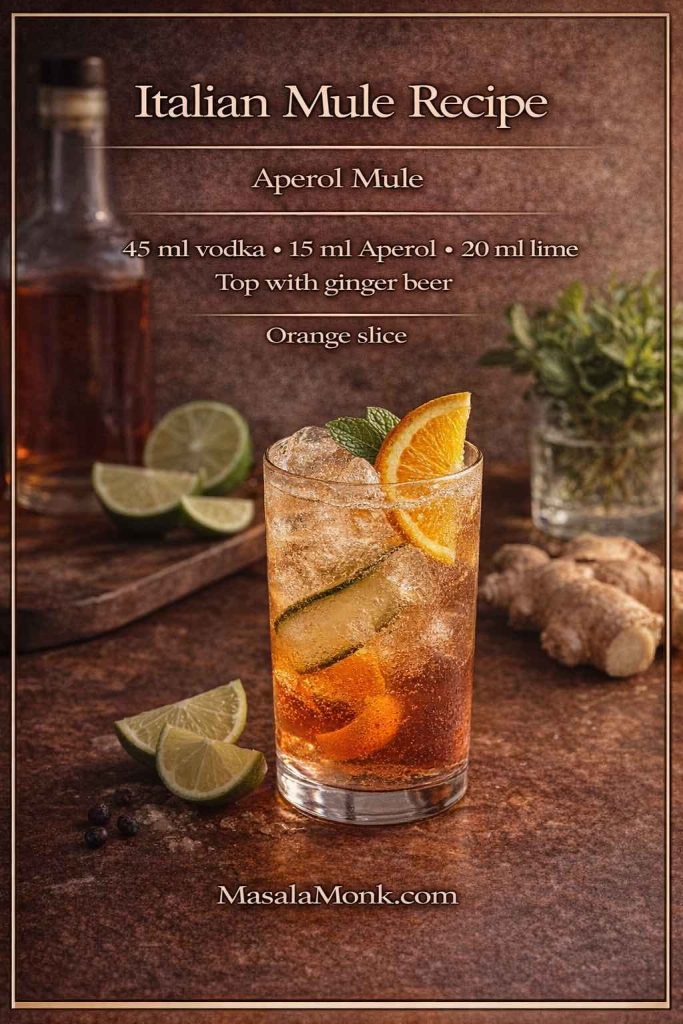
Italian mule recipe (aperitivo build)
- 45 ml vodka
- 15 ml Aperol (or a light amaro)
- 20 ml lime
- ginger beer to top
- garnish: orange slice
This version is especially useful when your ginger beer runs sweet. Consequently, bitterness keeps the drink from feeling like orange soda.
Also Read: Blueberry Pancakes (6 Recipes) + Homemade Pancake Mix
Cranberry Moscow mule recipe: tart, festive, and easy to love
A cranberry Moscow mule feels celebratory without being heavy. Moreover, it’s a crowd-pleaser because it tastes fruity while staying sharp.
For a close external reference, see Liquor.com’s Apple Cranberry Moscow Mule. Even if you don’t add apple, the balancing logic is similar.
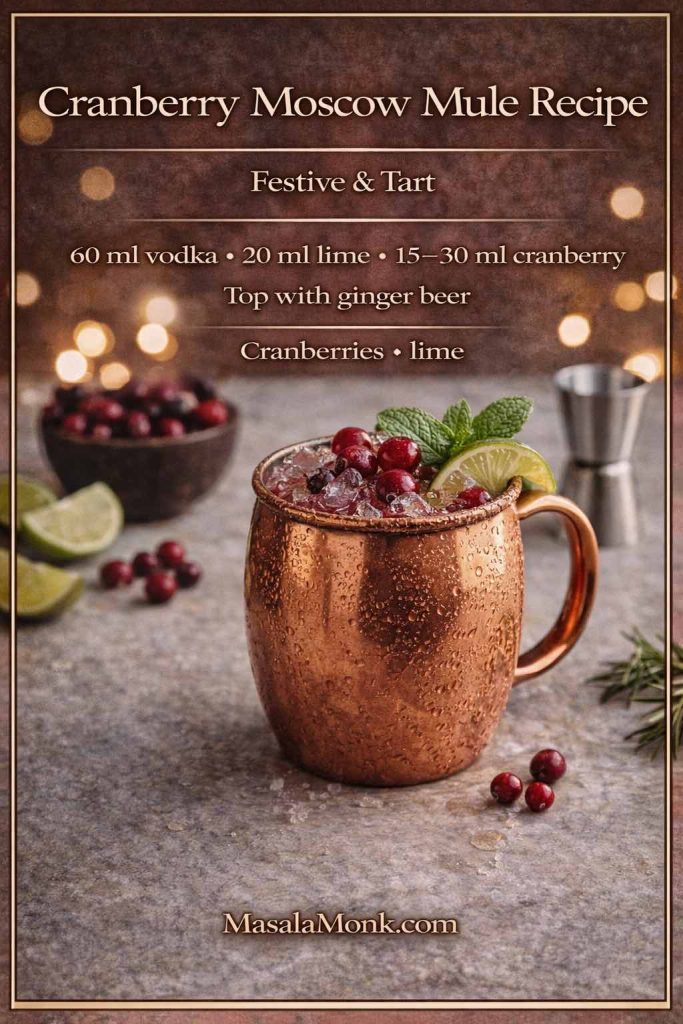
Cranberry Moscow mule recipe (balanced build)
- 60 ml vodka
- 15–30 ml cranberry juice (start small)
- 20 ml lime
- ginger beer to top
A tangy detour for readers who enjoy “bright” drinks
If you like cranberry’s sharpness, you might also enjoy a zero-proof cousin with similar flavors. MasalaMonk’s ACV and cranberry drink ideas fit naturally as a companion read because the taste family overlaps: tart, refreshing, and a little zippy.
Dessert pairing that fits the mood
Because cranberry loves spice, a warm, fragrant dessert works beautifully alongside it. For an indulgent but on-brand option, Churros with Indian-inspired variations can turn a simple drink night into something that feels planned.
Apple mule recipe and cinnamon-apple mule recipe: crisp, cozy, and surprisingly elegant
Apple and ginger are a natural pairing: apple brings sweetness and aroma, while ginger adds bite. Therefore, this variation works year-round—light in summer, cozy in cooler months.
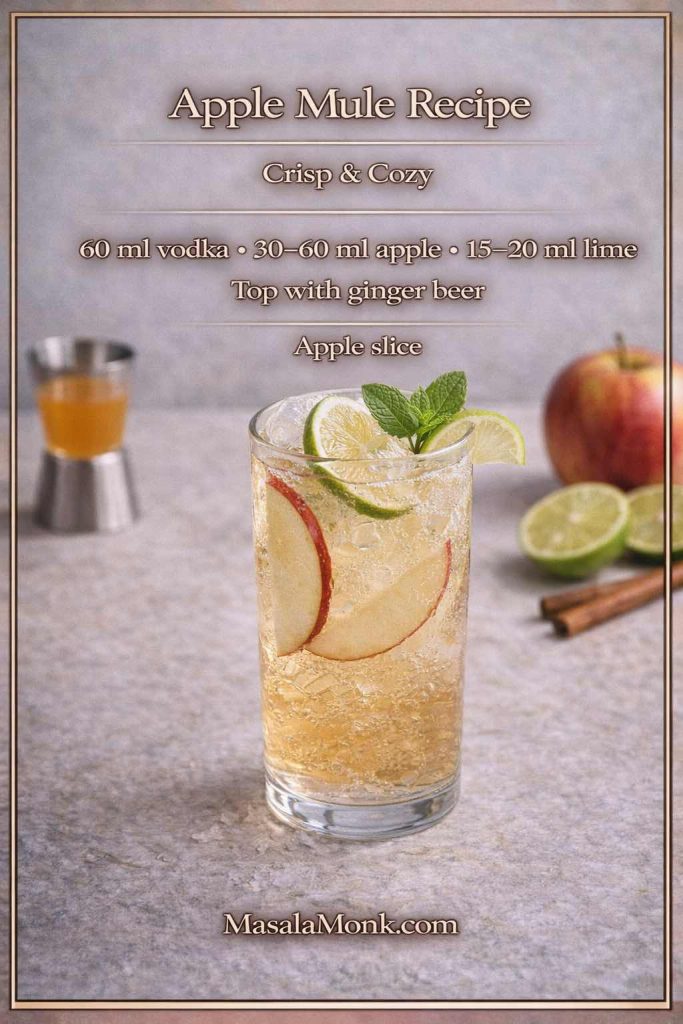
Apple mule recipe (crisp build)
- 60 ml vodka (or bourbon for a warmer version)
- 30–60 ml apple juice or cider
- 15–20 ml lime
- ginger beer to top
- garnish: apple slice
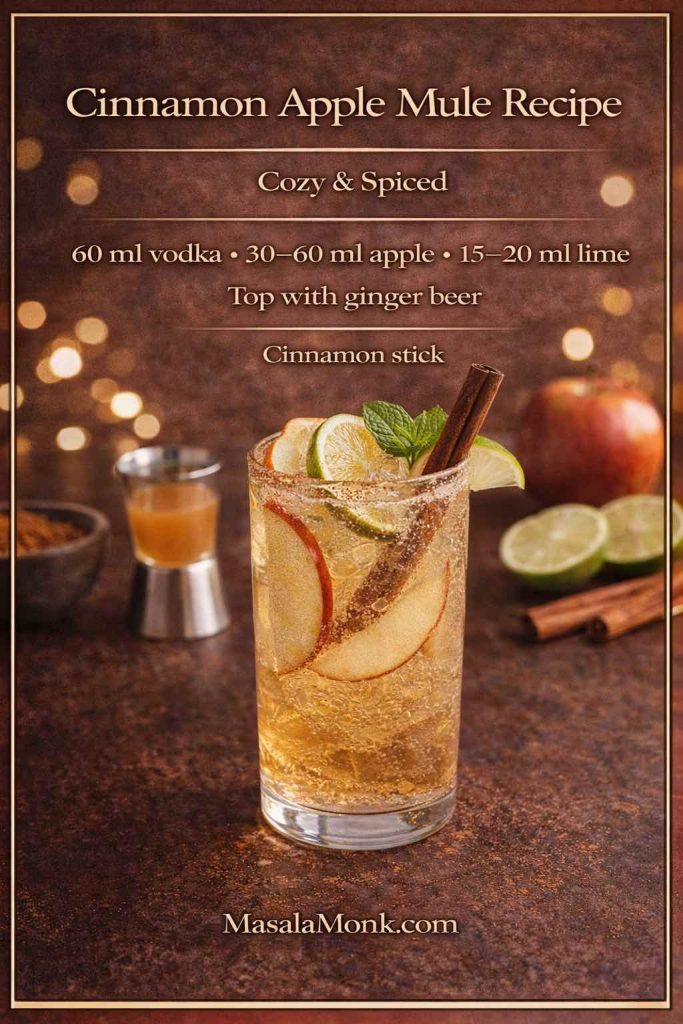
Cinnamon-apple mule recipe (cozy twist)
Use the Apple Mule build, then add:
- a cinnamon stick garnish, or
- a tiny pinch of cinnamon
Keep it subtle, because cinnamon can dominate if you’re heavy-handed.
For a non-alcoholic sibling that still captures the “apple + citrus + fizz” vibe, MasalaMonk’s Apple Juice Mocktails are a lovely companion link.
Ginger mule recipe: when you want more bite and less sweetness
Sometimes you don’t want a longer drink—you want the ginger to lead. In that case, choose a spicier ginger beer, keep lime bright, and avoid extra sugar.
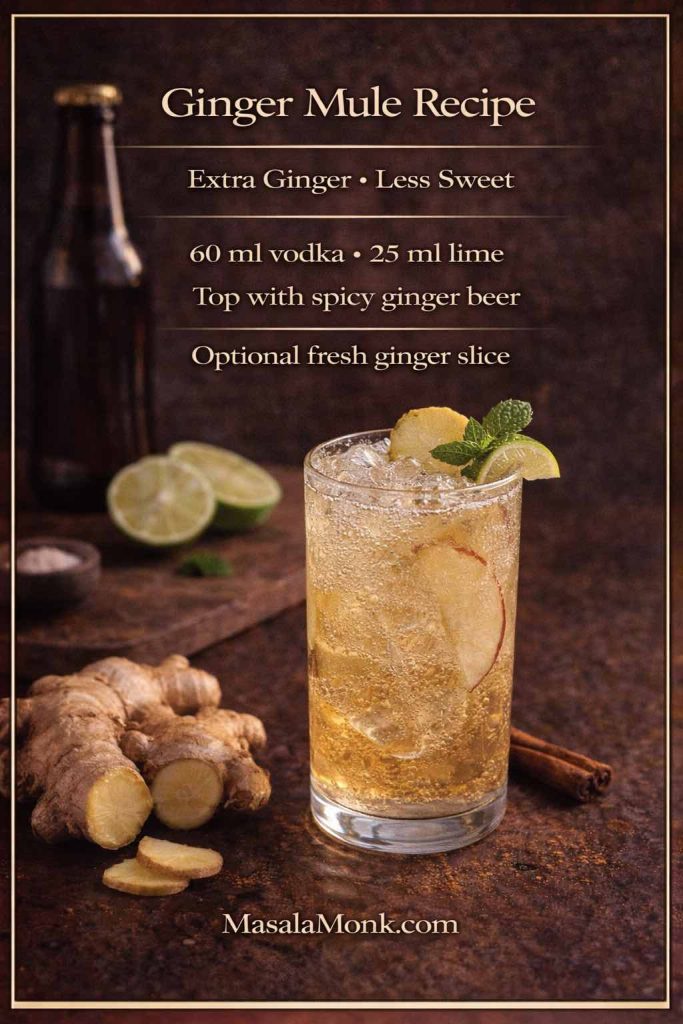
Ginger mule recipe (extra-ginger build)
- 60 ml vodka
- 25 ml lime
- ginger beer to top (start modest; add if needed)
- optional: fresh ginger slice, lightly muddled
- skip syrup unless your ginger beer is extremely dry
If you enjoy ginger beyond cocktails, MasalaMonk’s Ginger And Its Stunning Health Benefits is a natural internal link here because it keeps the reader in the same ingredient universe.
Also Read: One-Pot Chicken Bacon Ranch Pasta (Easy & Creamy Recipe)
Tropical mule recipe: coconut water, lime, and ginger fizz for hot evenings
A Tropical Mule feels like summer logic. Coconut water softens the edges, lime keeps it bright, and ginger adds the signature snap. Consequently, it’s an easy “conversion” drink for people who usually avoid cocktails.
MasalaMonk already plays in this space with Tropic Like It’s Hot: Coconut Water Cocktails, which includes Mule-style ideas that fit perfectly as a variation.
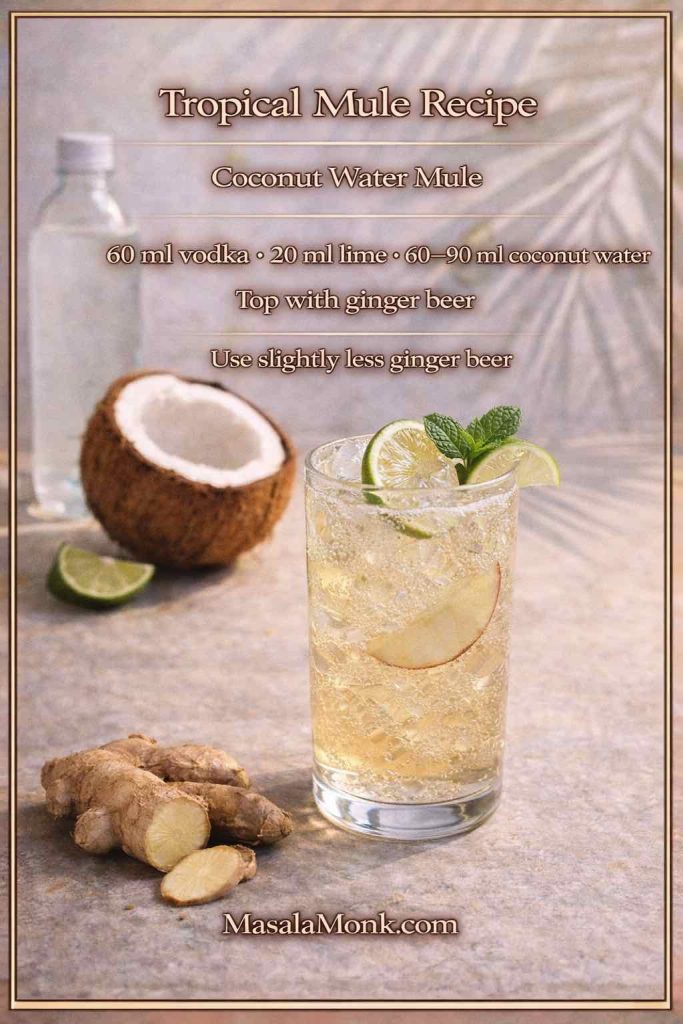
Tropical mule recipe (quick build)
- 60 ml vodka
- 20 ml lime
- 60–90 ml chilled coconut water
- ginger beer to top (slightly less than usual so ginger stays present)
Because coconut water adds volume, the slightly smaller ginger beer pour keeps the drink from becoming too diluted.
Also Read: French Toast Sticks (Air Fryer + Oven Recipe) — Crispy Outside, Custardy Inside
Moscow mule recipe with the bottle you already have: keeping balance without overthinking
Sometimes the only decision you’ve already made is the bottle sitting on your counter. Fortunately, the Mule is forgiving: you don’t need a brand-specific recipe; you just adjust balance.
- If your vodka tastes very clean and neutral, the Mule will feel crisp and classic, so you can push lime slightly higher if you enjoy sharpness.
- If your vodka tastes rounder or softer, a spicier ginger beer keeps the finish lively.
- If your vodka is exceptionally smooth, adding a touch more ginger bite (or a ginger garnish) keeps the drink from feeling muted.
The same logic applies to whiskey versions. Irish whiskey tends to make a brighter, gentler drink; bourbon tends to make a warmer, richer one. Consequently, once you know the master moscow mule recipe structure, you can adapt it without stress.
Also Read: Whole Chicken in Crock Pot Recipe (Slow Cooker “Roast” Chicken with Veggies)
Moscow mule recipe as a make-ahead base: fast drinks without losing fizz
Sometimes you want a Mule to be effortless—something you can make in under a minute while still tasting fresh. That’s where a make-ahead base helps. However, the trick is to keep carbonation separate until the last moment.
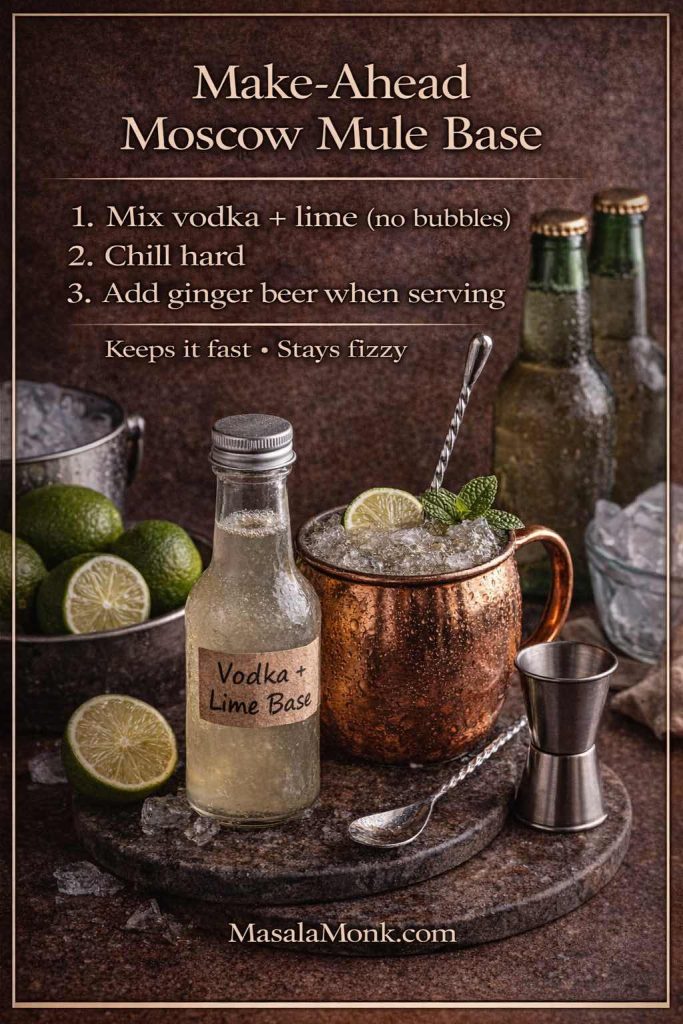
Make-ahead base (still ingredients only)
Combine:
- vodka
- lime juice
- optional: a very small amount of syrup (only if needed)
Chill the base. Then, when serving, pour it over ice and top with ginger beer. As a result, you get the convenience of a “mix” without sacrificing sparkle.
What you don’t want to do is pre-mix ginger beer and let it sit. Carbonation fades, and the drink loses its lift.
Also Read: Authentic Louisiana Red Beans and Rice Recipe (Best Ever)
Batch Moscow mule recipe for a party: keep it bright, keep it fizzy
A pitcher Mule sounds perfect until the last glass is flat. Nevertheless, batching can work beautifully if you respect the order of operations: still ingredients first, carbonation last.
For a clear, practical guide to cocktail batching principles, see Serious Eats’ how to batch cocktails. The key idea is simple: chill the base hard, then add bubbly components right before serving.
If you enjoy entertaining, it’s also helpful to see how party-friendly prep works in other drink formats. MasalaMonk’s Punch recipes with pineapple juice offer a nice internal companion link because they live in the same hosting universe: big flavors, smart dilution, and last-minute fizz.
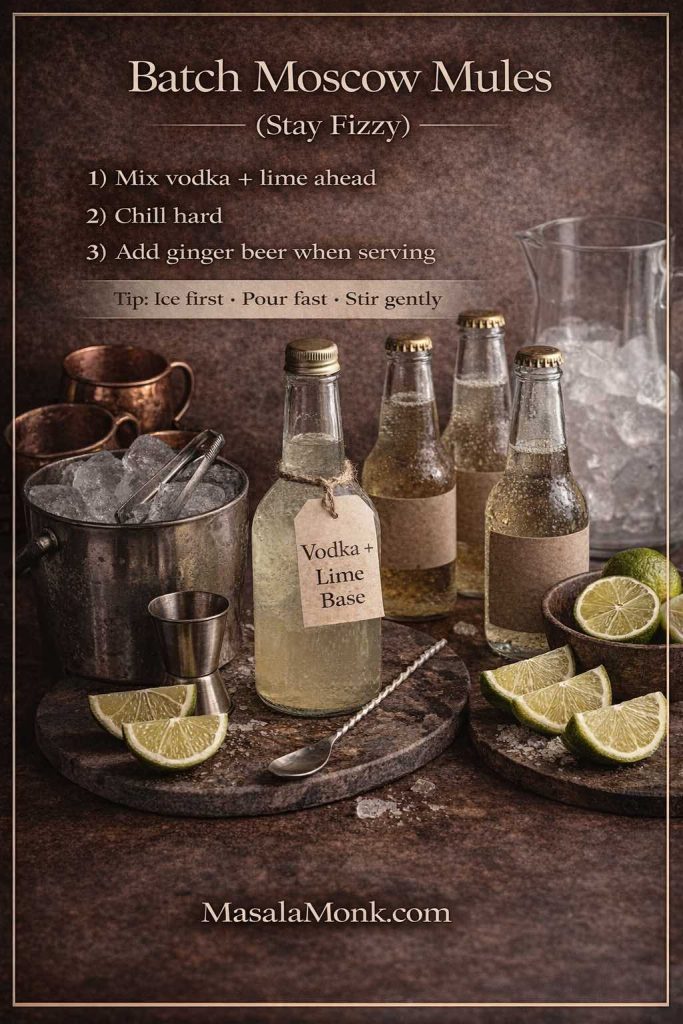
A party setup that prevents flat drinks
Instead of one giant pitcher, set up a quick build station:
- chilled base (vodka + lime, optional syrup)
- plenty of ice
- ginger beer on the side
- lime wedges
- optional garnishes (mint, orange slices, apple slices)
Then, guests can build classic Mules or variations. Meanwhile, you avoid the “sad final glass” problem entirely.
Also Read: Pepper Sauce Recipe Guide: Classic Vinegar Heat to Chipotle, Ají & Peppercorn
Moscow mule recipe and copper mugs: iconic style, plus one calm safety note
Copper mugs are part of the Mule’s identity: they look great, they stay cold, and they make the drink feel special. If you want the story in a quick read, why Moscow mules are served in copper mugs is a good explainer.
At the same time, lime juice is acidic, and unlined copper isn’t ideal for acidic drinks. For an official reference point, the FDA Food Code discusses copper use limitations for acidic foods and beverages here: FDA Food Code (Food Code 2022).
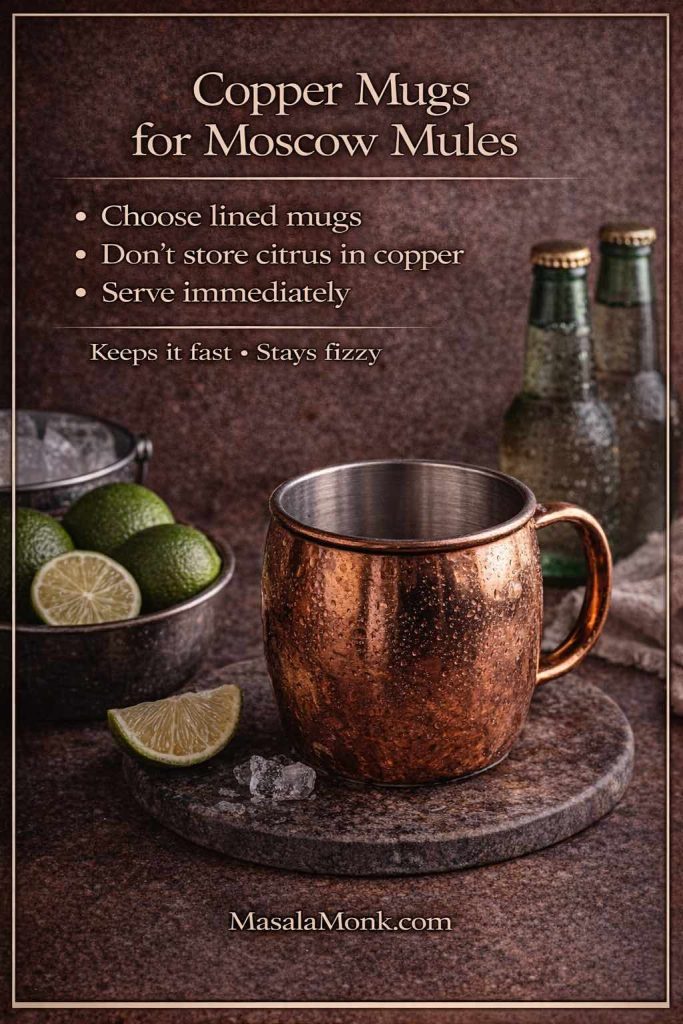
In practical terms, it’s simple:
- choose lined copper mugs if you’re buying
- don’t store citrus drinks in copper
- use a glass when you’re unsure
Either way, the moscow mule recipe still tastes fantastic.
Also Read: Baked Jalapeño Poppers (Oven) — Time, Temp & Bacon Tips
What to serve with a Moscow mule recipe: snacks, food, and desserts that match
A Mule tastes bright, gingery, and lime-forward. Therefore, it loves foods that are salty, crispy, tangy, or gently spiced. When you pair it thoughtfully, the drink seems even brighter.
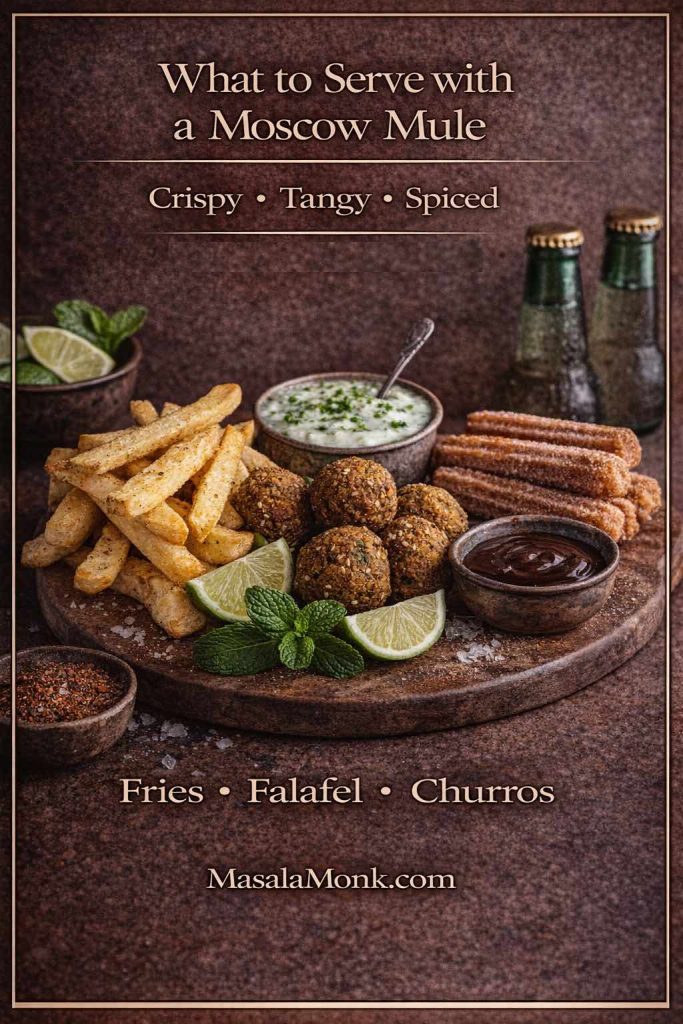
Crispy, salty comfort (easy and satisfying)
Fries are a classic pairing for a reason: salt amplifies ginger, while lime keeps everything from feeling heavy. For a great home version, MasalaMonk’s Homemade French Fries are perfect—especially if you finish them with a spice dust.
This pairing works across variations. For example, it’s excellent with a Mexican Mule because tequila and chili-lime seasoning are natural friends. Similarly, it’s great with a Kentucky Mule because ginger cuts through bourbon warmth.
Tangy, herby bites (lighter, brighter)
Falafel is a surprisingly good companion for Mules: crisp outside, tender inside, and often served with sauces that echo the drink’s citrus. For an Indian-leaning take that fits MasalaMonk’s style, Falafel with Indian twists is an easy internal link that feels genuinely relevant.
This pairing shines with gin mules and Irish mules, because those drinks lean refreshing and aromatic. Consequently, the whole table feels light rather than heavy.
Desserts that don’t fight the drink
Because Mules are zippy, desserts that lean into spice and warmth match beautifully. A cinnamon-apple mule, for instance, practically begs for something fragrant. Meanwhile, a cranberry Moscow mule loves festive spice.
For a sweet companion that still feels on-brand, Churros with Indian-inspired variations can turn “just drinks” into a full evening.
The simple reason this Moscow mule recipe keeps working
The Mule lasts because it solves a craving: cold, bright, fizzy, and ginger-spiced. Moreover, it’s flexible without becoming complicated. Once you learn the master moscow mule recipe, you can keep the structure and shift the personality depending on season and mood.
On a warm evening, the Tropical Mule makes sense. On a festive night, the cranberry Moscow mule feels right. When you want comfort, the Kentucky mule recipe is the move. When you want something sharper and louder, the Mexican mule recipe delivers. Meanwhile, when you want fragrance and lift, a gin mule recipe changes the whole atmosphere of the drink.
So start with the master build, keep everything cold, let lime and ginger do their job, and adjust with confidence. After all, the best moscow mule recipe is the one you’ll actually make again—and this one is designed to earn that repeat.
Also Read: Vegan Mayo Recipe Guide: 5 Plant-Based Mayonnaise
FAQs
1) What is the best Moscow mule recipe for beginners?
If you’re just starting, the best Moscow mule recipe is the classic build: vodka, fresh lime juice, and chilled ginger beer over plenty of ice. To begin with, use 60 ml vodka, 20–25 ml lime, then top with ginger beer. After that, adjust the ginger beer amount based on how strong or light you want the drink.
2) What are the essential Moscow mule ingredients?
At minimum, Moscow mule ingredients include vodka, fresh lime juice, ginger beer, and ice. Additionally, a lime wedge is the most common garnish. Occasionally, mint or bitters are added, although the core Moscow mule recipe doesn’t require them.
3) How do I make a Moscow Mule that doesn’t taste watery?
Primarily, pack the glass completely with ice and use well-chilled ginger beer. Next, build the drink quickly so the ice doesn’t melt while you measure. Finally, stir only once or twice; otherwise, you’ll speed up dilution and flatten the fizz.
4) How to make a Moscow mule at home without a copper mug?
Simply make the Moscow mule recipe in a highball or any sturdy glass. Even so, the most important part is keeping everything cold. In fact, glassware matters far less than fresh lime, cold ginger fizz, and plenty of ice.
5) Why are Moscow mules served in copper mugs?
Traditionally, copper mugs became associated with the drink because they look distinctive and feel colder in the hand. Still, you can enjoy the same Moscow mule cocktail flavor from any glass, so it’s more about experience than necessity.
6) Can I make a Moscow mule with ginger ale instead of ginger beer?
Yes. Instead of ginger beer, use ginger ale and increase lime slightly so the drink stays bright. Also, skip extra sweeteners, since ginger ale is often sweeter. As a result, the Moscow mule with ginger ale stays balanced rather than tasting like soda.
7) How do I make a Moscow mule without ginger beer?
If you don’t have ginger beer, you can use ginger ale plus a small boost of fresh ginger or ginger syrup. Alternatively, you can combine soda water with lime and ginger syrup for a similar ginger-lime highball feel. Either way, keep everything cold so the drink remains crisp.
8) What’s the difference between a vodka Moscow mule and a vodka mule drink?
Practically speaking, they’re the same drink. In other words, “vodka mule drink” is simply another way of referring to the classic Moscow mule recipe built with vodka, lime, and ginger beer.
9) What is the best vodka for a Moscow mule?
Generally, the best vodka for a Moscow mule is clean and neutral, because the Moscow mule cocktail is meant to highlight ginger and lime. If your vodka tastes sharper, add a touch more ginger beer; conversely, if it’s very smooth, choose a spicier ginger beer to keep the finish lively.
10) How much alcohol is in a Moscow Mule?
Typically, a standard Moscow mule recipe uses a single 60 ml pour of vodka, then gets lengthened by ginger beer and ice. Consequently, it often drinks lighter than a straight spirit, even though it can still be strong. If you want a lower-alcohol mule drink, reduce the vodka slightly and top with more ginger beer.
11) How many calories are in a Moscow Mule?
Calories depend mostly on the vodka pour and the sweetness of the ginger beer. For example, a sweeter ginger beer raises calories noticeably, whereas a drier ginger beer keeps them lower. Therefore, if calories matter, pick a less-sweet ginger fizz and avoid added syrup.
12) What is a Mexican mule, and how is it different from a Moscow Mule?
A Mexican mule replaces vodka with tequila while keeping lime and ginger beer. As a result, it tastes brighter and more “agave-citrus” than the classic. If you like the Moscow mule recipe but want a bolder twist, the Mexican mule is usually the easiest upgrade.
13) What is a Kentucky mule recipe?
A Kentucky mule recipe swaps vodka for bourbon. Because bourbon is warmer and sweeter, the drink feels more comforting, while ginger keeps it snappy. Additionally, a dash of bitters can add depth without adding sugar.
14) What is an Irish mule?
An Irish mule uses Irish whiskey instead of vodka. Compared with a bourbon mule, it often tastes lighter and smoother. Consequently, it’s a great option when you want a whiskey mule that still feels bright and refreshing.
15) What is a gin mule recipe?
A gin mule recipe replaces vodka with gin, creating a more aromatic, botanical version. Furthermore, mint or cucumber can fit naturally here, although the core formula—spirit, lime, ginger beer—stays the same.
16) What is an Italian mule cocktail?
An Italian mule cocktail usually adds an aperitivo element (like a light bitter orange spirit) alongside vodka, lime, and ginger beer. Therefore, it often tastes slightly more complex and less sweet, especially when your ginger beer is mild.
17) How do I make a cranberry Moscow mule recipe?
A cranberry Moscow mule recipe adds a small amount of cranberry juice to the classic Moscow mule ingredients. Start with a modest splash so it stays tangy rather than sugary, then top with ginger beer. Similarly, keep lime present; otherwise, cranberry can take over.
18) How do I make an apple mule drink?
An apple mule drink adds apple juice or cider to the Mule template. Next, keep lime in the mix so it remains bright, then top with ginger beer. If you want a cozier version, add a cinnamon stick garnish for a cinnamon-apple mule feel.
19) What is a ginger mule, and how do I make it less sweet?
A ginger mule is simply a Mule where ginger leads. To achieve that, choose a spicier ginger beer, increase lime slightly, and avoid syrup. Additionally, a thin slice of fresh ginger can intensify bite without adding sweetness.
20) Can I make a Moscow mule mix ahead of time?
Yes, but only the still parts. First, combine vodka and lime juice (and optional syrup if needed), then chill. Right before serving, pour over ice and top with ginger beer. Otherwise, if you add ginger beer early, the bubbles fade and the mule drink loses its lift.
21) How do I batch Moscow mules for a party?
For batching, pre-mix vodka and lime, chill the mixture thoroughly, and set up ginger beer separately. Then, when guests are ready, build each Moscow mule recipe over ice and top with ginger beer. Consequently, every glass stays fizzy instead of going flat in a pitcher.
22) What’s the best garnish for a Moscow Mule?
Most commonly, a lime wedge or wheel is ideal, because it reinforces the citrus aroma. Alternatively, mint adds freshness, and orange peel pairs nicely with whiskey or Italian mule variations. Either way, keep garnish simple so it supports the Moscow mule cocktail instead of distracting from it.
23) How do I make a Moscow Mule less sweet without changing the whole recipe?
First, add a bit more lime. Next, reduce the ginger beer pour slightly and choose a drier ginger beer if available. In addition, a tiny pinch of salt can sharpen the drink’s profile, so sweetness feels calmer rather than loud.
24) How do I make a Moscow Mule stronger or lighter?
To make it stronger, reduce ginger beer slightly while keeping lime steady. On the other hand, to make it lighter, add more ginger beer and keep plenty of ice. As a result, you can shift strength without breaking the Moscow mule recipe balance.