From your morning juice to luxurious spa treatments, oranges have long been nature’s citrus gift. Bursting with antioxidants and essential vitamins, this vibrant fruit does more than satisfy your taste buds—it works wonders for your skin too.
In this article, we’ll explore why oranges deserve a spot in your skincare routine, debunk some persistent myths, and share 5 easy, effective DIY recipes that will leave your skin glowing.
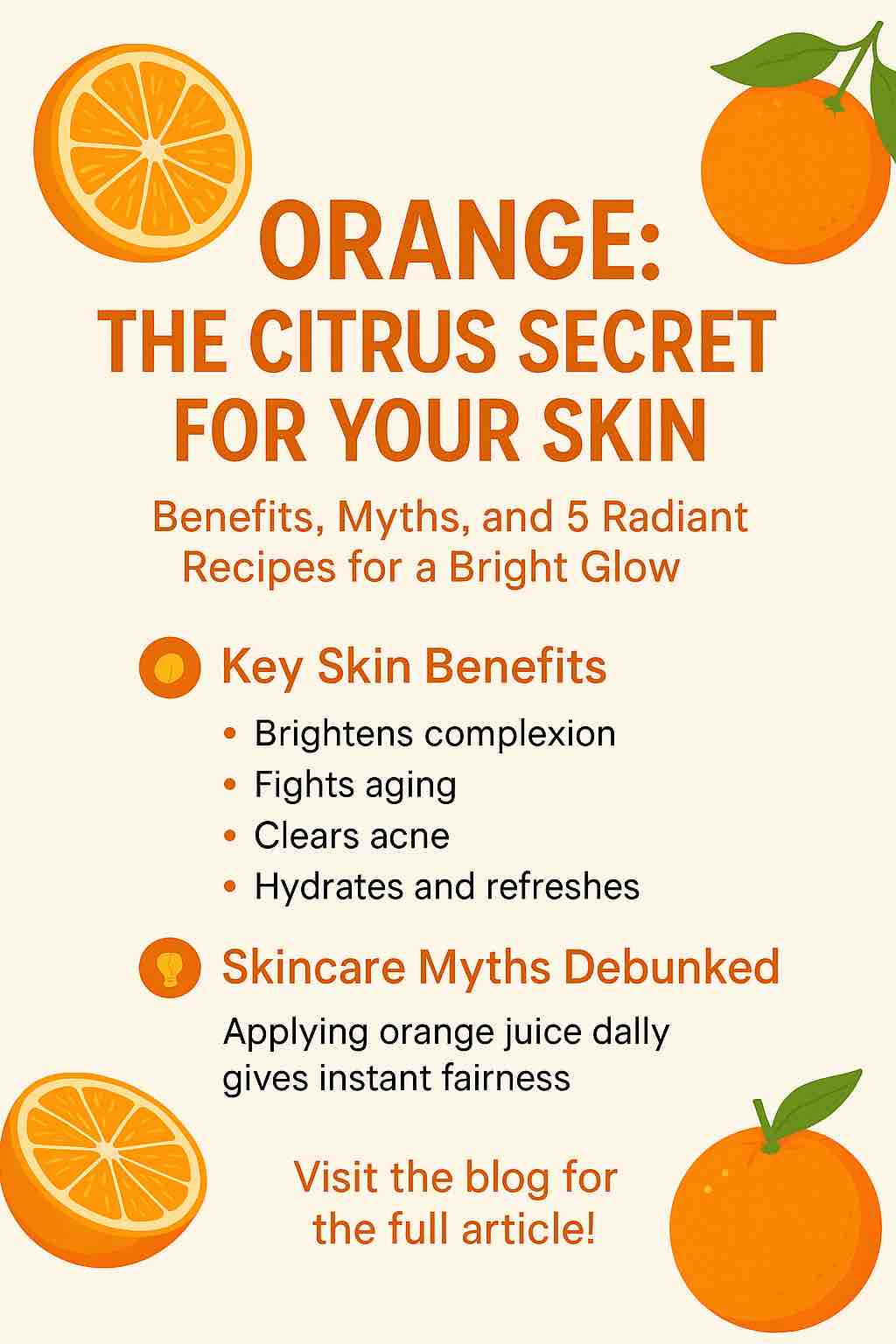
🍊 The Skin-Loving Benefits of Oranges
Oranges are packed with Vitamin C, citric acid, and antioxidants, making them a versatile ingredient for healthy, radiant skin. Here’s how they help:
✨ Brightens and Evens Out Skin Tone
Vitamin C helps inhibit melanin production, reducing dark spots, pigmentation, and dullness. Regular use (both topically and in your diet) can gradually boost skin’s radiance.
✨ Anti-Aging Action
Oranges are rich in flavonoids and beta-carotene, which combat free radicals responsible for premature aging, wrinkles, and sagging skin.
✨ Clears Acne and Blemishes
The citric acid in oranges works as a natural exfoliant, helping to unclog pores and reduce acne-causing bacteria.
✨ Hydration Boost
Orange extracts help refresh and hydrate skin, especially when paired with moisturizing agents like honey or yogurt.
🧪 Skincare Myths About Oranges — Debunked
Despite their many benefits, oranges are also surrounded by misinformation. Let’s clear the air:
| Myth | Reality |
|---|---|
| Applying orange juice daily will make your skin fairer instantly. | Oranges improve brightness over time, but overuse can cause sensitivity or dryness. |
| Orange peels are too harsh for the skin. | When dried and finely ground, orange peel powder is a gentle exfoliant. |
| Oranges can replace sunscreen. | Vitamin C offers antioxidant protection but does not block UV rays. Always wear SPF. |
| Orange essential oil is always safe. | It can be phototoxic. Always dilute and avoid sun exposure after application. |
🍊 5 Radiant Orange-Based Skincare Recipes (DIY)
These simple, natural recipes make the most of orange’s skincare potential. Use them weekly for best results.
1. Brightening Orange Peel Face Mask
What you need:
- 1 tbsp orange peel powder
- 1 tbsp yogurt
- A few drops of honey
How to use:
Mix into a smooth paste. Apply to clean skin and leave on for 15 minutes. Rinse with lukewarm water. This mask helps to reduce pigmentation and restore glow.
2. Citrus + Turmeric Tan Removal Pack
Ingredients:
- 1 tsp fresh orange juice
- A pinch of turmeric
- 2 tsp gram flour (besan)
How to use:
Apply to tanned or uneven skin. Let it dry and scrub off gently using damp fingers. Helps lighten sun damage and even out skin tone.
3. Hydrating Orange Ice Cubes
Ingredients:
- Fresh orange juice
- A few drops of rose water
How to use:
Pour the mix into an ice cube tray. Rub a cube on your face in the morning to tighten pores and energize tired skin.
4. Gentle Orange & Oatmeal Scrub
Ingredients:
- 2 tsp oatmeal
- 1 tsp orange zest or peel powder
- 1 tsp milk or yogurt
How to use:
Massage onto damp skin using circular motions, then rinse. This exfoliant removes dead skin cells and promotes smoother texture.
5. DIY Vitamin C Night Serum
Ingredients:
- Orange peel infused oil (infuse dried peels in jojoba or almond oil for 5–7 days)
- 1 Vitamin E capsule (optional)
How to use:
Apply a few drops to cleansed face at night. Massage gently to improve skin elasticity and brightness.
⚠️ Important Tips When Using Orange-Based Products
- Do a patch test before applying any orange-based product, especially if you have sensitive skin.
- Avoid direct sunlight immediately after using citrus-based masks or oils.
- Always use fresh juice or peel; avoid store-bought juice with additives.
🌟 Final Thoughts
Oranges are more than a refreshing fruit—they’re a skincare ally that can transform your routine naturally. Whether you’re looking to fade blemishes, revitalize dull skin, or fight early signs of aging, orange-based skincare offers a cost-effective and powerful solution. Just remember: consistency, moderation, and sun protection are key.
Want to try these out? Let us know which orange recipe worked best for you—or share your own in the comments below!













