Pregnancy is a time when you’re not just eating for two — you’re nourishing for two. Every nutrient you consume (or don’t) plays a role in how your baby grows and how your own body adapts to this incredible journey. Among all the vitamins and minerals, Vitamin D holds a special place.
It’s often called the sunshine vitamin, but it’s actually more like a hormone that affects bone strength, immunity, muscle function, and possibly even your baby’s brain development. Yet, despite its importance, many expecting mothers around the world — including in sunny countries like India — don’t get enough.
Today, we’ll explore:
- Why Vitamin D matters so much during pregnancy
- What the latest 2024–2025 research really says
- How much you should aim for
- Food, sunlight, and supplement sources
- Practical tips to keep you and your baby healthy
Also Read: What Are the Symptoms of Gestational Diabetes?
☀️ Why Vitamin D Matters in Pregnancy
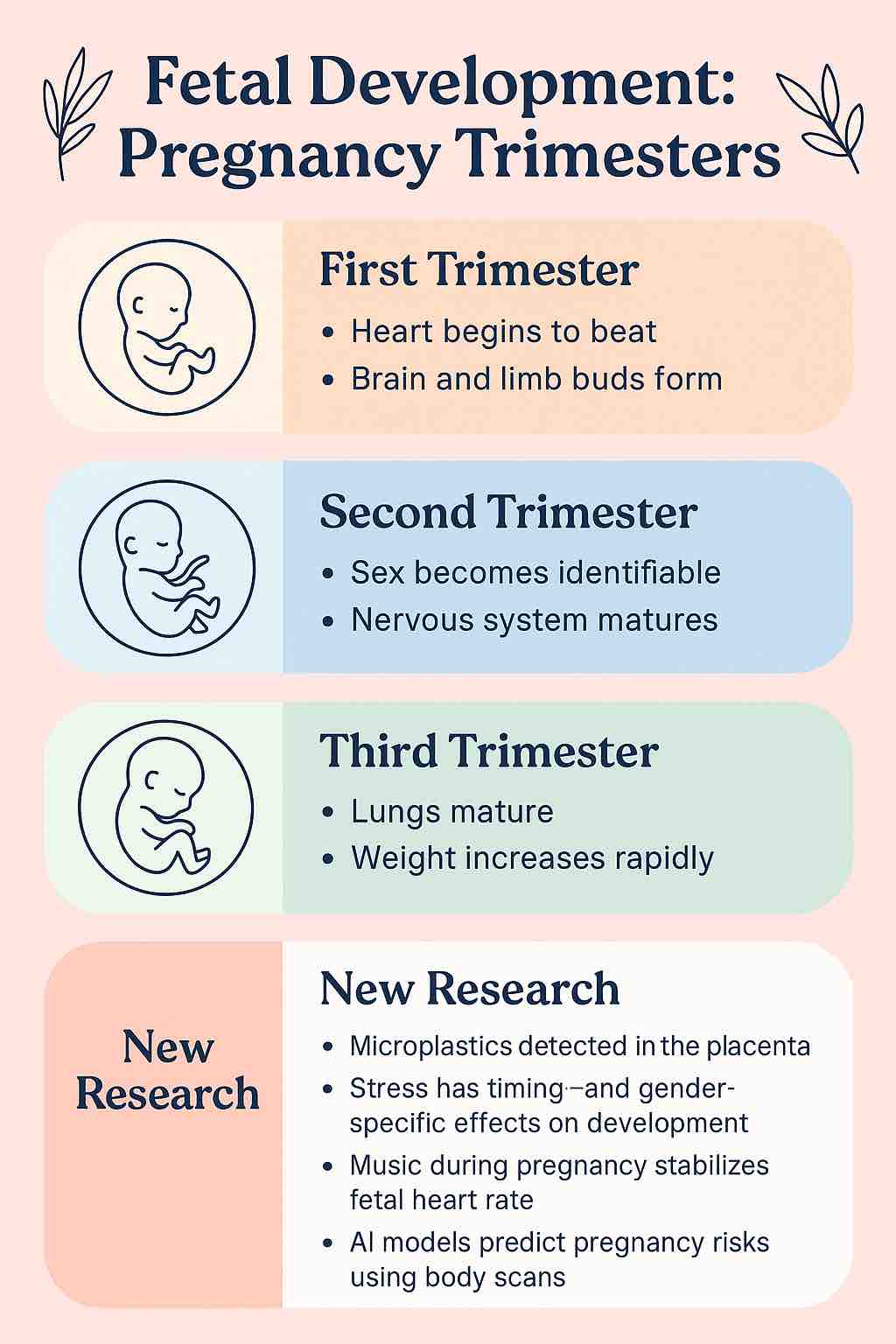
During pregnancy, your body is working overtime to build tiny bones, a developing immune system, and a growing brain — all of which rely on Vitamin D. Without enough of it, your baby may not get the calcium they need for healthy skeletal development, and you might face risks like:
- Preeclampsia – a dangerous rise in blood pressure during pregnancy
- Gestational diabetes – high blood sugar that can affect you and your baby
- Preterm birth – delivering before 37 weeks
- Low birth weight
- Weakened immunity and bone strength
And here’s something fascinating: low Vitamin D levels in pregnancy have been linked in observational studies to higher risks of conditions like ADHD, autism spectrum disorder, and even schizophrenia later in life. The science is still evolving, but it shows just how far-reaching Vitamin D’s role might be.
🥗 Learn how Vitamin D fits into the bigger picture:
Introduction to Pregnancy Nutrition: Empowering Your Journey to Motherhood
📊 What the Latest Research Says (2024–2025)
Science is never static — and Vitamin D research in pregnancy is one of those areas where new studies keep changing the conversation. Let’s break it down.
1. Big Global Analyses — Mixed, but Important
- A 2025 meta-analysis (66 RCTs, over 17,000 women) found no strong evidence that Vitamin D prevents preeclampsia or preterm birth in all women, but it did lower the risk of gestational diabetes and slightly increased average birth weight.
- The 2024 Cochrane Review — known for being strict about evidence — concluded that results are still uncertain for many pregnancy complications, but noted possible benefits for maternal health and newborn outcomes.
2. Positive Signals from Specific Trials
- A 2024 analysis of 33 trials reported a 45% lower risk of preeclampsia and 30% lower risk of preterm labor with Vitamin D supplementation.
- A large RCT in DR Congo (2024) using a monthly 60,000 IU dose reduced rates of preeclampsia, preterm birth, and low birth weight.
3. Sunlight Still Matters
In Scotland, researchers looked at 400,000 pregnancies and found that women with more sunlight exposure in the first trimester had lower risks of preterm birth and pregnancy loss. Even if you take supplements, your skin can make Vitamin D naturally — and it may come with other health perks.
4. Brain Development & Beyond
While low Vitamin D at birth has been linked to higher risks of ADHD, autism, and schizophrenia in observational studies, supplement trials haven’t yet proven prevention. This is one area where more research is definitely needed.
🌱 For trimester-specific tips:
First Trimester Nutrition: Building the Foundation for a Healthy Pregnancy
📏 How Much Vitamin D Do You Actually Need?
Here’s what leading health bodies say:
| Organization / Region | Daily Recommendation | Safe Upper Limit |
|---|---|---|
| US NIH / WHO | 600 IU (15 mcg) | 4,000 IU |
| UK NHS | 400 IU (10 mcg) | 4,000 IU |
| Endocrine Society (2024) | Suggests supplementation (often ~2,000 IU/day in studies) without routine testing in healthy pregnancies | 4,000 IU |
| India-specific advice | 1,000–2,000 IU/day if deficiency suspected; up to 4,000 IU/day for confirmed deficiency | 4,000 IU |
💡 Tip: Most prenatal vitamins contain about 400–800 IU of Vitamin D, so if you’re deficient, your doctor may recommend an extra supplement.
Also Read: 5 Protein-Packed Smoothies for Pregnancy with Peanut Butter and Chia Seeds
🥗 Natural & Food Sources of Vitamin D
Unlike some vitamins, Vitamin D is harder to get from food alone — but every bit counts.
- Fatty fish: salmon, sardines, mackerel, tuna Read: Tuna in Pregnancy – How to Eat It Safely
- Fortified dairy & plant milks: many are enriched with Vitamin D Read: Almond Milk During Pregnancy
- Egg yolks
- Mushrooms (especially UV-exposed varieties)
- Fortified cereals
And of course — sunlight:
- Aim for 15–30 minutes of mid-morning sun a few times a week, arms and face uncovered, without sunscreen (but don’t overdo it to avoid burns).
🍲 Need ideas? Try our Calcium & Vitamin D-Rich Recipes for Expecting Mothers
📝 Practical Tips for Expecting Moms
- Get your levels checked if you have risk factors: darker skin, limited sun exposure, vegetarian/vegan diet, or history of deficiency.
- Start early — bone and brain development begin in the first trimester.
- Combine strategies: sun exposure, diet, and supplements (if needed).
- Don’t mega-dose on your own — very high levels can be harmful.
- Pair with calcium for maximum benefit to bone health.
Also Read: 5 Iron-Rich Snack Ideas for Pregnant Women: Energizing Chicken and Quinoa Combos
🧐 Vitamin D & Pregnancy: Myths vs Facts
Myth 1: “I live in a sunny country, so I can’t be deficient in Vitamin D.”
Fact: Even in sunny places like India, deficiency is very common due to indoor lifestyles, pollution, sunscreen use, and clothing that covers most skin. Sunlight exposure is important, but it’s not always enough.
Myth 2: “If I take a prenatal vitamin, I don’t need extra Vitamin D.”
Fact: Most prenatals contain 400–800 IU of Vitamin D, which may not be enough if you’re starting pregnancy with low levels. Your doctor may recommend an additional supplement.
Myth 3: “More Vitamin D is always better.”
Fact: Mega-dosing without medical supervision can cause toxicity, leading to high calcium levels, kidney problems, and even heart issues. Stick to safe upper limits (4,000 IU/day unless your doctor prescribes more for deficiency).
Myth 4: “Vitamin D is only about bones.”
Fact: It also supports immune function, muscle strength, and possibly brain development — for both you and your baby.
Myth 5: “Supplements can replace sunlight completely.”
Fact: Supplements are great for meeting your needs, but safe sun exposure also helps regulate other body processes and may have benefits beyond Vitamin D.
💡 Tip: Combine sunlight + Vitamin D-rich foods + supplements (if needed) for a balanced approach.
💬 The Bottom Line
Vitamin D is essential during pregnancy — for you and your baby. While not all studies agree on exactly how much it prevents complications, we do know that deficiency is common and safe supplementation can help close the gap.
Think of it like this: you wouldn’t try to build a house without enough bricks. Vitamin D is one of those bricks — and making sure you have enough gives your baby the strongest possible foundation.
🔍 For more on safe prenatal eating:
Safe Eating During Pregnancy: Foods to Eat, Avoid, and Safety Practices
❓ Frequently Asked Questions – Vitamin D & Pregnancy
1. Why is Vitamin D important during pregnancy?
Vitamin D helps your body absorb calcium, which is essential for your baby’s bone and teeth development. It also supports immune health and may lower the risk of pregnancy complications such as preeclampsia and gestational diabetes.
2. How can I tell if I’m deficient in Vitamin D?
Many women have no symptoms, but possible signs include fatigue, muscle weakness, bone pain, and frequent illnesses. A simple blood test (25-hydroxyvitamin D) can confirm deficiency.
3. How much Vitamin D should I take during pregnancy?
Most guidelines recommend 600 IU (15 mcg) daily, but if you are deficient, your doctor may advise up to 4,000 IU/day. Do not exceed this without medical supervision.
4. Can I get enough Vitamin D from sunlight alone?
Possibly, but factors like skin tone, clothing, sunscreen, pollution, and time spent outdoors can reduce Vitamin D production. In many cases, a combination of sunlight, diet, and supplements is needed.
5. Which foods are good sources of Vitamin D?
Fatty fish (salmon, sardines, tuna), fortified dairy or plant milks, eggs, and UV-exposed mushrooms are top sources.
6. Is it safe to take Vitamin D supplements while pregnant?
Yes, when taken in recommended doses. Very high doses without medical supervision can cause toxicity and harm to you and your baby.
7. Does Vitamin D prevent preeclampsia and preterm birth?
Research is mixed. Some studies suggest reduced risk, while others show no significant benefit. It’s clear, however, that maintaining adequate Vitamin D is important for overall health.
8. Can too much Vitamin D harm my baby?
Yes. Excessive intake can lead to high calcium levels, which may cause kidney or heart issues. Stick to safe upper limits unless prescribed otherwise.
9. Should all pregnant women get tested for Vitamin D?
Routine testing isn’t recommended for healthy pregnancies in some guidelines (like the Endocrine Society, 2024). Testing may be advised if you have risk factors such as limited sun exposure, darker skin, or a vegan diet.
10. When should I start Vitamin D supplementation?
Ideally before or early in pregnancy, especially if you have risk factors for deficiency. Bone and brain development begin early, so early supplementation may be most beneficial.