If you’re reading this, you’re likely at a crossroads: A loved one (or maybe you) has just been diagnosed with Alzheimer’s or a related dementia, and the doctor is talking about donepezil—also known by its brand name, Aricept. The pamphlet lists side effects, but what does this actually look like in the real world? Is it worth it? Will it help, hurt, or make no difference at all?
We’ve collected and synthesized hundreds of real-life stories, reviews, and discussions from forums, support groups, and medical communities to paint a true-to-life portrait of what it means to start, stay on, or stop donepezil. If you want honest insights—and practical steps for handling the ups and downs—you’re in the right place.
1. Understanding Donepezil: What It Does and Who Gets It
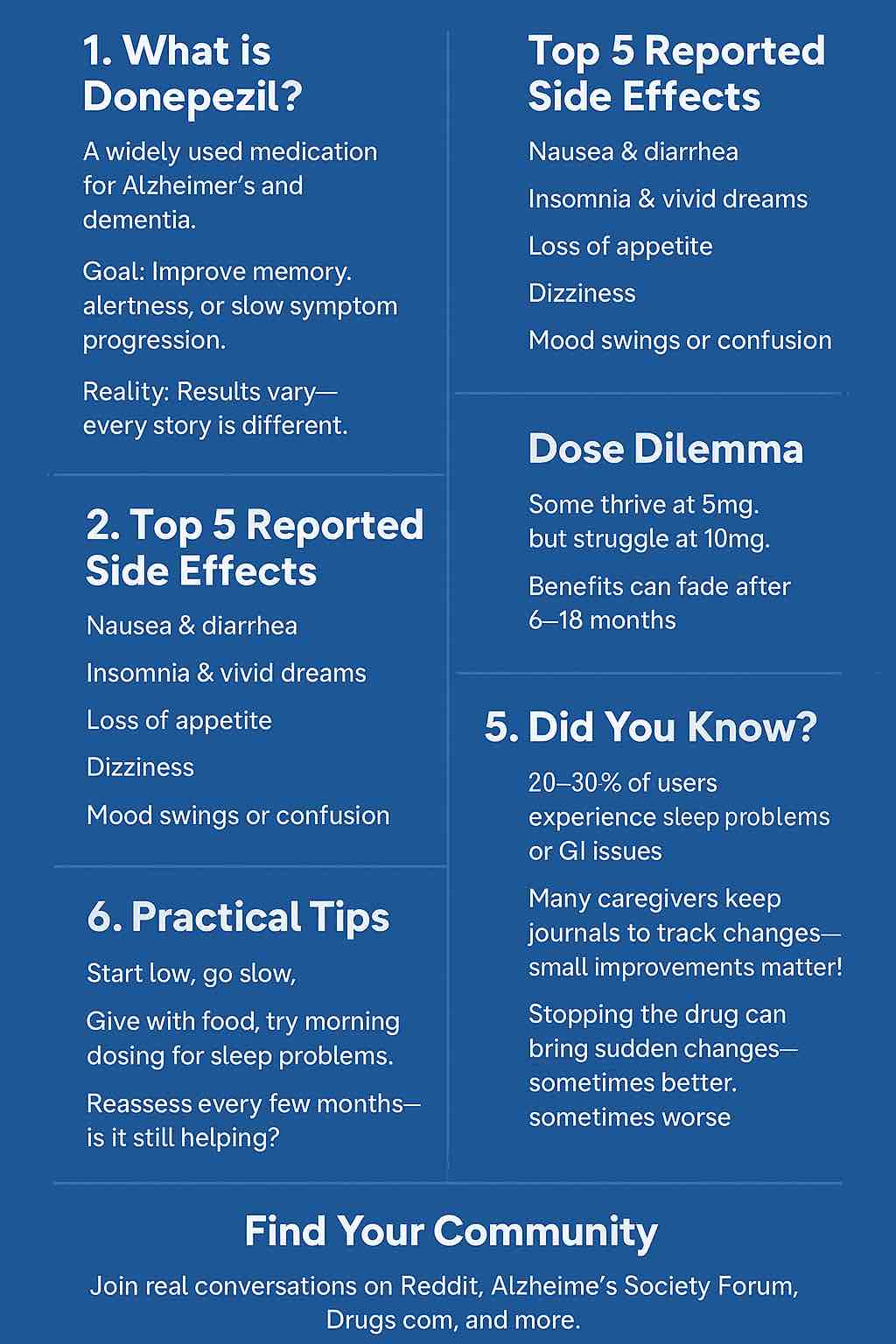
Donepezil is one of the most widely prescribed medications for Alzheimer’s disease and, sometimes, other forms of dementia. Its main goal is to slow down the breakdown of acetylcholine—a chemical messenger involved in learning and memory. It is not a cure. At best, it may temporarily slow the progression of symptoms, improve alertness, or help with certain behaviors.
Who gets prescribed donepezil?
- Most often, people with mild to moderate Alzheimer’s.
- Sometimes, those with Lewy Body Dementia or Vascular Dementia.
- Increasingly, people with early cognitive symptoms or “mild cognitive impairment.”
2. The First Dose: Hope, Hesitation, and First Impressions
What Doctors Say Will Happen
Doctors typically start at 5 mg daily, often at night to minimize early side effects, and may increase to 10 mg after a month if tolerated. Leaflets warn about:
- Nausea
- Diarrhea
- Sleep issues
- Dizziness
But the lived experience is often more complex.
What Caregivers and Patients Actually See
🟢 Success Stories and Small Victories
- Reddit user: “Within two weeks, Mom seemed so much more present… She could finish her sentences, remembered my son’s name, even told a joke at dinner. The whole family noticed.”
- Alzheimer’s Society forum: “Dad became brighter. He started reading again and joined in crossword puzzles, which he hadn’t done in months. He was also less paranoid, which was a relief.”
- Drugs.com review: “My husband on donepezil: Not a miracle, but he could make a cup of tea on his own again. That mattered more than I realized.”
🔴 Early Disappointments and Tough Starts
- Mayo Clinic Connect: “Started on 5 mg. Nausea so bad, my wife stopped eating. She lost 5 pounds in two weeks. Switched to morning dosing and food, but still miserable.”
- Reddit caregiver: “My dad got so agitated—pacing the house, up all night, snapping at everyone. We lasted two weeks before pulling the plug.”
- Drugs.com: “I was hopeful but just got diarrhea, confusion, and more falls.”
⚪ No Change at All
- Alzforum.org: “We saw absolutely no difference, good or bad. Stayed on for six months, then stopped. No change.”
3. The First Month: Navigating Side Effects
Most Common Side Effects (Based on User Reports)
| Symptom | How Often? (est. from reviews/forums) | Typical Onset | Comments |
|---|---|---|---|
| Nausea | ~1 in 4 | First 1-2 weeks | Usually improves, but can be severe |
| Diarrhea | ~1 in 5 | Early | Can lead to stopping |
| Appetite Loss | ~1 in 6 | Early | Weight loss a risk |
| Vivid Dreams | ~1 in 5 | Within days/weeks | Often dose-related |
| Insomnia | ~1 in 4 | Within first week | Dose timing helps |
| Headache | ~1 in 10 | Early | Usually mild |
| Muscle Cramps | ~1 in 10 | Variable | Often manageable |
| Dizziness | ~1 in 10 | Any time | Monitor for falls |
Quotable Experiences:
- “My husband was up every hour at night, dreaming vividly and talking in his sleep.” (Alzheimer’s Forum)
- “No appetite—my mom lost 10 lbs before we realized it was the meds.” (Reddit)
- “We switched to morning dosing; nightmares and insomnia went away.” (Drugs.com)
Less Common but Serious
- Slowed heart rate (bradycardia)
- Fainting or falls
- Black stools or vomiting blood (GI bleeding)
- Worsening confusion or hallucinations, especially in Lewy Body dementia
Tip: Always report new confusion, fainting, severe GI symptoms to your doctor immediately.
4. Dose Increases: The Double-Edged Sword
Moving from 5 mg to 10 mg is where things often change—for better or worse.
What Users Report:
- Some see more improvement (“Another boost, like the fog cleared even more”).
- Others see a return of side effects, especially GI issues and vivid dreams.
- Occasionally, agitation or mood swings emerge at the higher dose.
Caregiver Wisdom:
- “10 mg was too much—mom got mean and suspicious. Went back to 5 mg and she mellowed out.”
- “No difference at all, just more diarrhea. Dropped back to 5 mg per doc’s advice.”
Doctors may say the 10 mg dose is standard, but many families stay at 5 mg due to tolerability. This is absolutely fine—always prioritize quality of life over dose ‘targets’.
5. Months and Years: The Rollercoaster of Long-Term Use
The Honeymoon Period
- Some families describe an initial “lift” that fades over 6-18 months. After that, symptoms return or plateau.
- A minority maintain small but meaningful improvements for years.
User Voices:
- “He stayed more alert for about a year, then slowly declined again. But it gave us more good months together.”
- “I think it helped at the beginning, but after two years we noticed no difference.”
Long-Term Side Effects
- GI issues (nausea, diarrhea) can persist or reappear.
- Sleep disruptions are common—caregivers often adapt by shifting dose to morning.
- Some report urinary incontinence or worsening of existing conditions (especially in men with prostate issues).
6. Stopping Donepezil: Fears, Realities, and Surprises
What Happens When You Stop?
- Some experience no change at all (cognitive status and behavior unchanged).
- Some improve—especially if donepezil was causing agitation or confusion.
- Others report rapid decline in memory or function, which may or may not persist.
Sample Experiences:
- “We stopped cold turkey (per doctor). She was calmer, but memory didn’t change.”
- “When we stopped, he became much more aware of his confusion and was deeply sad. But the aggression vanished.”
- “There was a sharp drop-off in function after stopping, then things leveled out.”
If the medication is stopped for more than a week, restart at the lowest dose—never resume at a higher dose without doctor guidance.
7. Special Populations and Cautions
- Lewy Body Dementia: Higher risk of hallucinations, confusion, and agitation with donepezil.
- People with Heart Issues: Donepezil can slow the heart rate; always monitor for fainting or dizziness.
- Elderly & Frail: More sensitive to side effects; benefits must be weighed against risks of falls and dehydration.
8. Practical Tips from the Trenches
What Families Wish They Knew Sooner
- Start low, go slow. Always give with food. Try morning dosing if sleep is disrupted.
- Track changes. Use a simple journal: appetite, sleep, mood, memory, bowel habits.
- Set realistic expectations. Not everyone benefits, and effects are usually modest and temporary.
- Watch for subtle improvements. Engaging in hobbies, talking more, smiling—these matter, even if big changes aren’t seen.
- Be ready to stop or adjust. Your experience may change over time; revisit the medication’s value every few months.
- Consult with your doctor regularly, especially if new symptoms emerge.
- Seek support. Join forums, local support groups, or counseling—caregiver burnout is real.
9. The Big Picture: Is Donepezil Worth It?
The honest answer: It depends.
- For some, it’s a lifeline—restoring pieces of personality and function.
- For others, it’s a non-starter, causing more harm than good.
- For many, the effects are subtle and temporary.
What’s universal? Every person’s dementia journey is unique. Don’t be afraid to advocate for what feels right for your loved one and your family.
10. Where to Find Real-World Experiences
If you want to read unfiltered stories, these forums are gold:
- Reddit r/dementia
- Alzheimer’s Society UK Forum
- Drugs.com User Reviews for Donepezil
- Mayo Clinic Connect
11. Sample Stories (In Their Own Words)
- Reddit: “The first month on donepezil was rough—nausea, nightmares, confusion. Then she stabilized. The improvement was small but real. Worth it for us.”
- Drugs.com: “I saw my dad go from silent and withdrawn to laughing again. Only lasted a year, but we’d do it again.”
- Alzheimer’s Forum: “I wish we’d been warned about the sleep problems—nobody in the house slept! Now we dose at breakfast, and everyone’s happier.”
- Mayo Clinic Connect: “I felt helpless when my husband became so agitated and suspicious. We stopped the medicine, and he became himself again.”
12. Final Thoughts: Navigating Donepezil in the Real World
Start with hope, but keep expectations realistic. Track what matters most to you, whether it’s memory, mood, engagement, or safety. Don’t be afraid to say “enough” if the negatives outweigh the positives. Your role as an advocate is essential, and there’s no “one size fits all.”
Above all: You are not alone. Every story is unique, but you’ll find echoes of your journey in the voices of others who have walked this path.
13. Invitation: Share Your Experience
Have you tried donepezil for yourself or a loved one? What surprised you? What worked, or didn’t? Share your story below or in one of the linked forums—your insights could help another family facing this difficult decision.
14. Additional Resources
- Alzheimer’s Association
- Lewy Body Dementia Association
- Family Caregiver Alliance
- NHS: Side Effects of Donepezil
10 FAQs on Donepezil (Aricept) Experiences and Side Effects
1. How quickly will we notice any effects from donepezil?
Answer:
Some people notice changes within the first 2–4 weeks, especially improvements in attention or conversation. For others, it can take 6–12 weeks to see the maximum effect—or there may be no noticeable change at all. Monitor daily routines for subtle improvements or new side effects.
2. What are the most common side effects, and how can we manage them?
Answer:
The most common side effects are nausea, diarrhea, loss of appetite, insomnia, vivid dreams, headache, and dizziness. Taking the medication with food, staying hydrated, and dosing in the morning (to reduce sleep issues) can help. If side effects are severe or don’t improve after a couple of weeks, contact your healthcare provider.
3. Is it normal for donepezil’s benefits to fade over time?
Answer:
Yes, for many, the positive effects plateau or decline after 6–18 months. Alzheimer’s is a progressive condition, so ongoing decline is expected. However, even modest improvements can be meaningful for quality of life.
4. Can donepezil make symptoms worse or cause new problems?
Answer:
In some people, donepezil can increase confusion, agitation, aggression, or hallucinations, especially in those with Lewy Body Dementia. Serious effects like fainting or black stools should be reported to a doctor immediately.
5. What should we do if donepezil is causing insomnia or vivid dreams?
Answer:
Try moving the dose to the morning. If symptoms persist, discuss with your doctor whether a lower dose or discontinuation is appropriate.
6. Do we have to increase the dose from 5mg to 10mg?
Answer:
Not necessarily. Some people tolerate 5mg well but experience more side effects at 10mg. If 5mg is helpful and side effects are minimal, it’s reasonable to stay at that dose—always check with your doctor.
7. What happens if we miss a dose or stop the medication suddenly?
Answer:
Missing one dose is usually not harmful—just take the next dose as scheduled. If the medication is stopped for more than a week, consult your doctor before restarting (it’s safest to begin again at the lowest dose). Stopping suddenly can lead to a rapid return of symptoms or, rarely, withdrawal-like effects.
8. Is donepezil safe for people with other health problems?
Answer:
Donepezil can interact with heart problems (like slow heart rate), stomach ulcers, and urinary issues. Always inform your doctor about all health conditions and medications before starting.
9. What are signs that we should stop donepezil?
Answer:
Stop and seek medical advice if there’s severe nausea, vomiting, black stools, fainting, slowed heart rate, uncontrollable agitation, or new hallucinations. If side effects outweigh any benefits, a trial off the medication may be recommended by your doctor.
10. Where can we read more real-world experiences or connect with others?
Answer:
Active online communities include Reddit’s r/dementia, the Alzheimer’s Society UK Forum, Drugs.com user reviews, and Mayo Clinic Connect. These platforms feature unfiltered stories and practical advice from caregivers and patients worldwide.