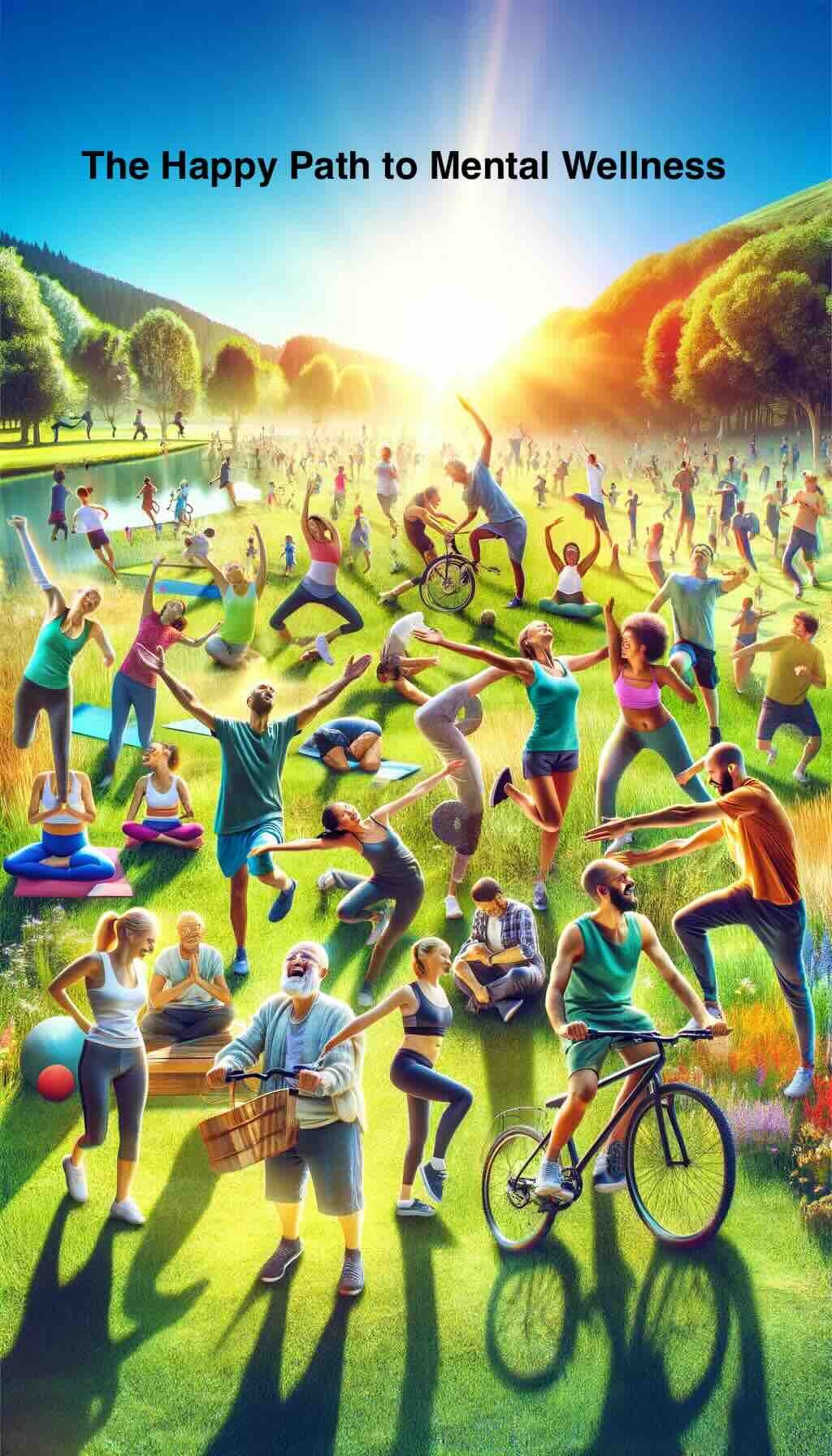
In the realm of mental health, an unexpected hero emerges—not from the shelves of pharmacies or the couches of therapists, but from the very movement of our bodies. The connection between physical activity and mental wellness is a tale as old as time, yet it’s one that’s gaining a fresh, vigorous spotlight in today’s fast-paced world. Let’s dive into this dynamic relationship and uncover practical ways to harness the power of movement for your mental health.
The Science of Movement and Mental Health
At the heart of this exploration is a simple, profound truth: moving your body can dramatically improve your mental state. But why is that? How does something as basic as walking, stretching, or dancing wield such influence over the complex workings of our minds?
Research reveals that physical activity kick-starts a series of biochemical processes in the brain. It’s like hitting the refresh button on your computer; suddenly, everything runs smoother. Exercise releases endorphins, the body’s feel-good neurotransmitters, which act as natural painkillers and mood elevators. It also stimulates the production of brain-derived neurotrophic factor (BDNF), a protein that helps repair brain cells and build new neural connections. Imagine your brain is a garden; physical activity is the rain that nourishes it, encouraging growth and bloom.
But the benefits don’t stop there. Regular movement has been shown to reduce symptoms of anxiety and depression, boost self-esteem, and improve sleep. In a world where mental health issues are on the rise, these findings are not just encouraging; they’re a call to action.
Practical Ways to Move Your Way to Mental Wellness
So, how can you start incorporating more movement into your life to reap these mental health benefits? The beauty lies in the simplicity and accessibility of physical activity. Here are some practical, punchy tips to get you moving:
1. Find Your Joy in Movement
The key to sustainable physical activity is enjoyment. Forget slogging through exercises you hate. Explore different activities until you find the ones that make you feel alive. Whether it’s dancing in your living room, hiking through nature, or practicing yoga, your perfect activity is out there.
2. Integrate Movement into Your Daily Routine
Make physical activity a natural part of your day. Cycle to work, take the stairs, walk while you take calls, or do a 10-minute workout during your lunch break. Small changes can lead to big differences in your mental health.
3. Set Realistic Goals
Start with achievable goals to avoid feeling overwhelmed. Even a 10-minute walk can uplift your mood. As you build confidence and stamina, gradually increase the intensity and duration of your activities.
4. **Connect with Others
Physical activity can be a social affair. Join a class, find a workout buddy, or engage in team sports. The combination of social interaction and exercise can be incredibly beneficial for your mental health.
5. Listen to Your Body
Remember, the goal is mental wellness, not physical exhaustion. Pay attention to your body’s signals and give yourself permission to rest when needed. Balance is key.
The Ripple Effect of Movement on Mental Health
As you incorporate more movement into your life, you may notice a ripple effect. Physical health improvements, increased energy, better focus, and a more positive outlook on life are just the beginning. Movement empowers you to take control of your mental health, one step at a time.
Embracing the Movement Mindset
In conclusion, the path to mental wellness doesn’t have to be complicated. By embracing the movement mindset, you unlock a powerful tool for managing stress, enhancing your mood, and improving overall mental health. Let’s not underestimate the power of our own two feet, the rhythm of our heartbeat, and the agility of our bodies to dance through life’s challenges. Your mental health journey can be a vibrant, moving experience. So lace up your shoes, and let’s get moving towards a happier, healthier mind.
FAQs for “Who Knew Sweating Could Make You Smile? The Happy Path to Mental Wellness”
1. How does physical activity benefit mental health?
Physical activity releases endorphins and stimulates the production of BDNF, improving mood, reducing anxiety and depression symptoms, boosting self-esteem, and enhancing sleep quality.
2. How much exercise do I need to see benefits for my mental health?
Even short bouts of exercise, such as a 10-minute walk, can boost your mood. Aim for at least 150 minutes of moderate aerobic activity or 75 minutes of vigorous activity per week for substantial benefits.
3. What are some simple ways to incorporate more movement into my daily routine?
You can cycle to work, take stairs instead of elevators, walk during phone calls, or engage in short workout sessions during breaks.
4. Can physical activity replace medication or therapy for mental health issues?
While physical activity is beneficial for mental wellness, it should complement, not replace, professional medical advice and treatments for those with serious mental health conditions.
5. Do I need to join a gym to get enough physical activity?
No, many forms of physical activity don’t require a gym, such as walking, dancing, cycling, or yoga. The key is to find activities you enjoy and can do regularly.
6. How can I stay motivated to keep moving?
Set realistic goals, track your progress, vary your activities to keep things interesting, and find a workout buddy or group for social support.
7. Is there a best time of day to exercise for mental health benefits?
While any time of day is beneficial, some people find that exercising in the morning helps set a positive tone for the day or engaging in physical activity during breaks can help relieve stress.
8. Can physical activity help with sleep problems?
Yes, regular physical activity can help regulate your sleep patterns, making it easier to fall asleep and improving the quality of your sleep.
9. What if I don’t feel any improvement in my mental health after starting to exercise?
Benefits can take time to manifest. Consistency is key. If you’re struggling with severe mental health issues, consult a healthcare professional for a comprehensive treatment plan.
10. Are there specific types of exercise that are more beneficial for mental health?
While any form of physical activity is beneficial, aerobic exercises like walking, running, cycling, and swimming have been shown to have a significant positive impact on mental health.
Blog Tags for the Post
mental health, physical activity, wellness, exercise, mood improvement, stress relief, anxiety reduction, depression management, lifestyle change, mental wellness strategy