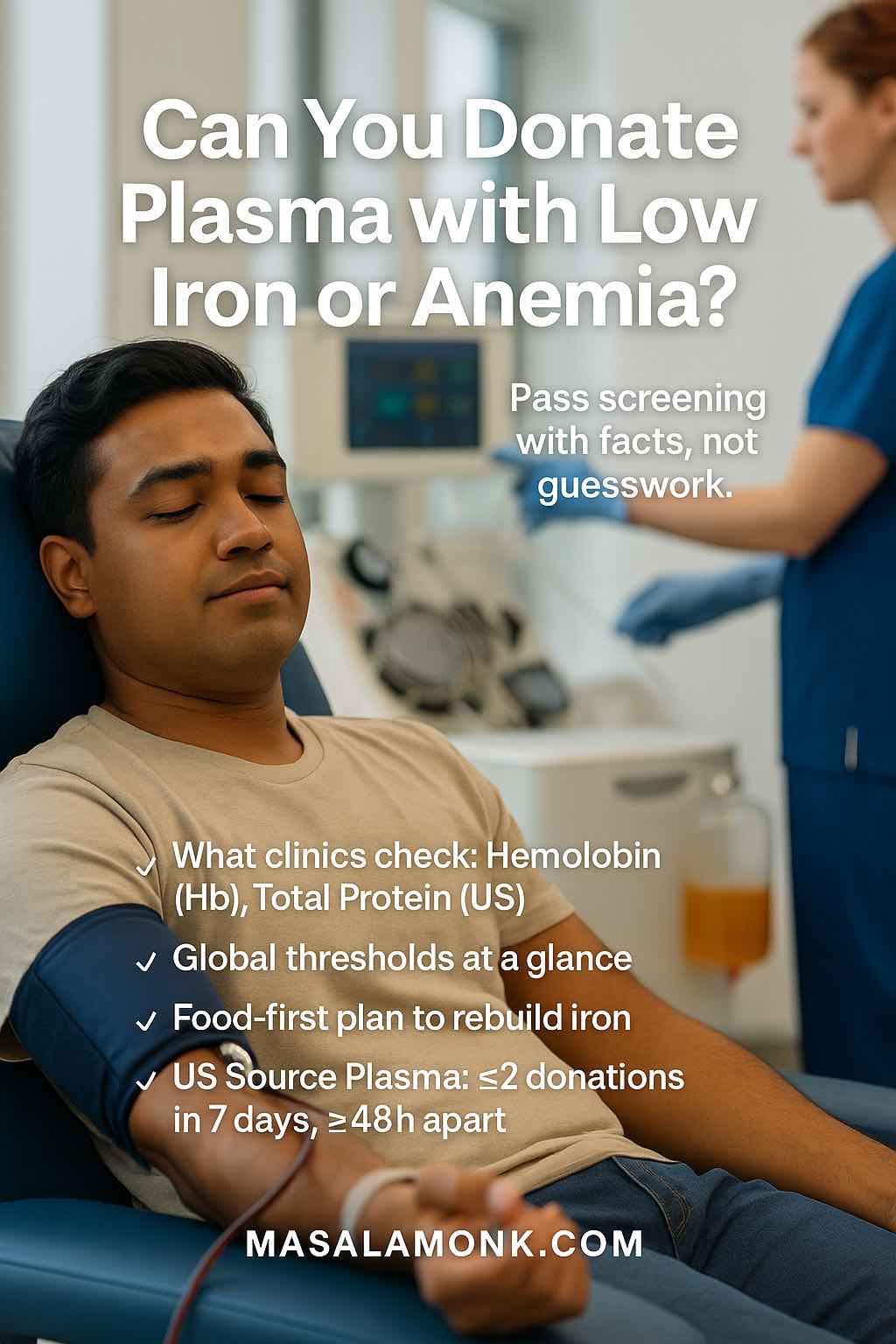
You showed up ready to help. Then a quick inger-prick said “not today.” If you’ve been told your iron is low or you live with anemia, the next question is immediate: can you donate plasma with low iron or anemia, and if not, how do you return safely? This guide answers those questions plainly. It explains what clinics check on the day, how thresholds differ across countries, and—crucially—how to raise your levels in a steady, realistic way so you can pass screening and donate confidently.
A global guide to what clinics check, how to rebuild safely, and where to verify rules.
Also Read: Iron-Rich Foods for Blood Donation: What to Eat Before & After
Disclaimer: This article is general information for donors. It isn’t medical advice, nor does it replace your local blood service’s rules. Always follow your clinician’s guidance and your country’s eligibility criteria.
What Clinics Check Today (Even for Plasma)
Plasma donation returns your red blood cells to you, so the iron hit is smaller than with whole blood. Nevertheless, clinics still must confirm you’re safe that day. Two checks matter most:
- Hemoglobin (or hematocrit). This is a same-day snapshot of your oxygen-carrying capacity. If it’s below your local cut-off, you’ll be deferred to prevent worsening anemia or faintness. For a U.S. reference point, the thresholds used in screening are outlined on the American Red Cross eligibility page.
- Total protein (for Source Plasma in the U.S.). Because plasma is rich in proteins, Source Plasma programs also check total protein before collection and strictly control how often you can donate. The frequency rule—no more than twice in seven days, with at least 48 hours between sessions—is specified in federal regulations; see the CFR text for Source Plasma at §640.65 (PDF) or the live eCFR §640.65. The total protein requirement appears in eCFR §630.15. For an at-a-glance FDA overview, you can also keep the agency’s program manual PDF handy: FDA Compliance Program Guidance Manual (Source Plasma inspections).
If either result is low, that’s a pause, not a verdict. You’ll be invited back after recovery.
Unit tip: Some services use g/L while others use g/dL. 1 g/dL = 10 g/L (so 12.5 g/dL = 125 g/L; 13.0 g/dL = 130 g/L). Apparent differences are often just unit changes.
Table 1 — Same-day screening results: what can defer you, and how to come back
| Screen item | What it measures | If it’s low today | How to return to “yes” |
|---|---|---|---|
| Hemoglobin / Hematocrit | Oxygen-carrying capacity right now | Temporary deferral for safety | 2–4 weeks of iron-forward meals; consider short clinician-guided iron if appropriate; re-screen |
| Total protein (where required) | Protein level in plasma (albumin, antibodies) | Temporary deferral | Increase overall protein intake (meals/snacks) while keeping iron work going; re-screen per program |
| General wellness (hydration, illness, meds) | Day-of readiness to donate | Staff may defer or ask you to wait | Recover, hydrate, bring a current med list; re-book when you feel well |
This table helps readers understand why they might be deferred and exactly how to get back to eligibility to donate plasma with low iron or anemia history.
Global Thresholds at a Glance (So You Can Verify Locally)
The logic is universal—protect the donor first—but numbers and cadence vary slightly by country.
- United States. Day-of hemoglobin thresholds used in screening are shown on the American Red Cross eligibility page. For Source Plasma, the twice-in-7-days, ≥48 hours spacing appears in CFR §640.65 (PDF) (live view: eCFR §640.65), and the total protein requirement is in eCFR §630.15.
- Canada. Canadian Blood Services sets plasma hemoglobin at ≥125 g/L for all donors, while whole blood uses ≥125 g/L (female) and ≥130 g/L (male). See Hemoglobin & iron and the explainer What is hemoglobin?.
- United Kingdom. NHS Blood and Transplant requires ≥125 g/L for women and ≥135 g/L for men before donation; details are on Haemoglobin and iron.
- Australia. Your hemoglobin must be in the acceptable range on the day: whole blood — women 120–165 g/L, men 130–185 g/L; plasma/platelets — women ≥115 g/L, men ≥125 g/L (upper ranges 165–185 g/L). Plasma can be given about every two weeks when eligible. See What is plasma? and Lifeblood’s iron guidance for clinicians here.
- India. National guidance expects hemoglobin ≥12.5 g/dL for donation. See the DGHS/MoHFW document “Guidelines for Voluntary Blood Donation” and the NBTC/NACO donor selection circular (PDF).
Table 2 — Plasma donation at a glance (same-day checks & typical rhythm)
| Country / Service | Same-day hemoglobin minimum* (women / men) | Plasma-specific checks | Typical plasma frequency** |
|---|---|---|---|
| United States (general screening; Source Plasma programs) | ~12.5 g/dL / 13.0 g/dL | Total protein check for Source Plasma; standard wellness screen | Up to 2 donations in 7 days, with ≥48 hours between (Source Plasma) |
| Canada (Canadian Blood Services) | Plasma: ≥125 g/L (single threshold) · Whole blood: ≥125 g/L (F) / ≥130 g/L (M) | Wellness screen; Hb must meet threshold | Program-specific (check your CBS clinic) |
| United Kingdom (NHSBT) | ≥125 g/L / ≥135 g/L | Wellness screen; Hb must meet threshold | Program-specific (check NHSBT) |
| Australia (Lifeblood) | Plasma: ≥115 g/L / ≥125 g/L · Whole blood: 120–165 g/L / 130–185 g/L | Wellness screen; Hb must meet threshold | About every 2 weeks when eligible |
| India (NBTC / NACO guidance) | ≥12.5 g/dL (all donors) | Wellness screen; Hb must meet threshold | Program-specific (check your center) |
*Hemoglobin (Hb) is measured on the day to determine if you can donate plasma with low iron or anemia history safely.
**Donation cadence is set by national services and individual centers. Where a fixed interval isn’t shown, please confirm with your local provider.
Unit tip: 1 g/dL = 10 g/L (12.5 g/dL = 125 g/L; 13.0 g/dL = 130 g/L).
Can You Donate Plasma with Low Iron or Anemia? (The Straight Answer)
Here’s the honest version: you can donate plasma with low iron or anemia only after your hemoglobin is back in range, and—if your program requires it—your total protein is normal. If your iron stores are low but your hemoglobin tests in range that day, many centers will still collect plasma, because your red cells are returned. However, if hemoglobin is below the cut-off (or protein is low where required), you’ll be asked to rebuild first. That pause protects you from feeling unwell and from drifting into deeper deficiency.
How to Raise Iron Levels to Give Blood (and Pass Plasma Screening)
There’s no magic hack; instead, there’s a rhythm that works. Start with food, anchor a few repeatable meals, then—if needed—add a short, clinician-guided supplement. Consequently, your numbers tend to rise in a way that sticks.
1) Confirm What Was Low (Hemoglobin or Total Protein)
Before changing anything, ask the clinic which result triggered the deferral: hemoglobin/hematocrit or total protein. If protein was the issue (more common in U.S. Source Plasma settings), you’ll focus on steady protein as well as iron. If hemoglobin was low, you’ll concentrate on iron and absorption. For the U.S., the protein rule and spacing are documented in eCFR §630.15 and CFR §640.65 (PDF).
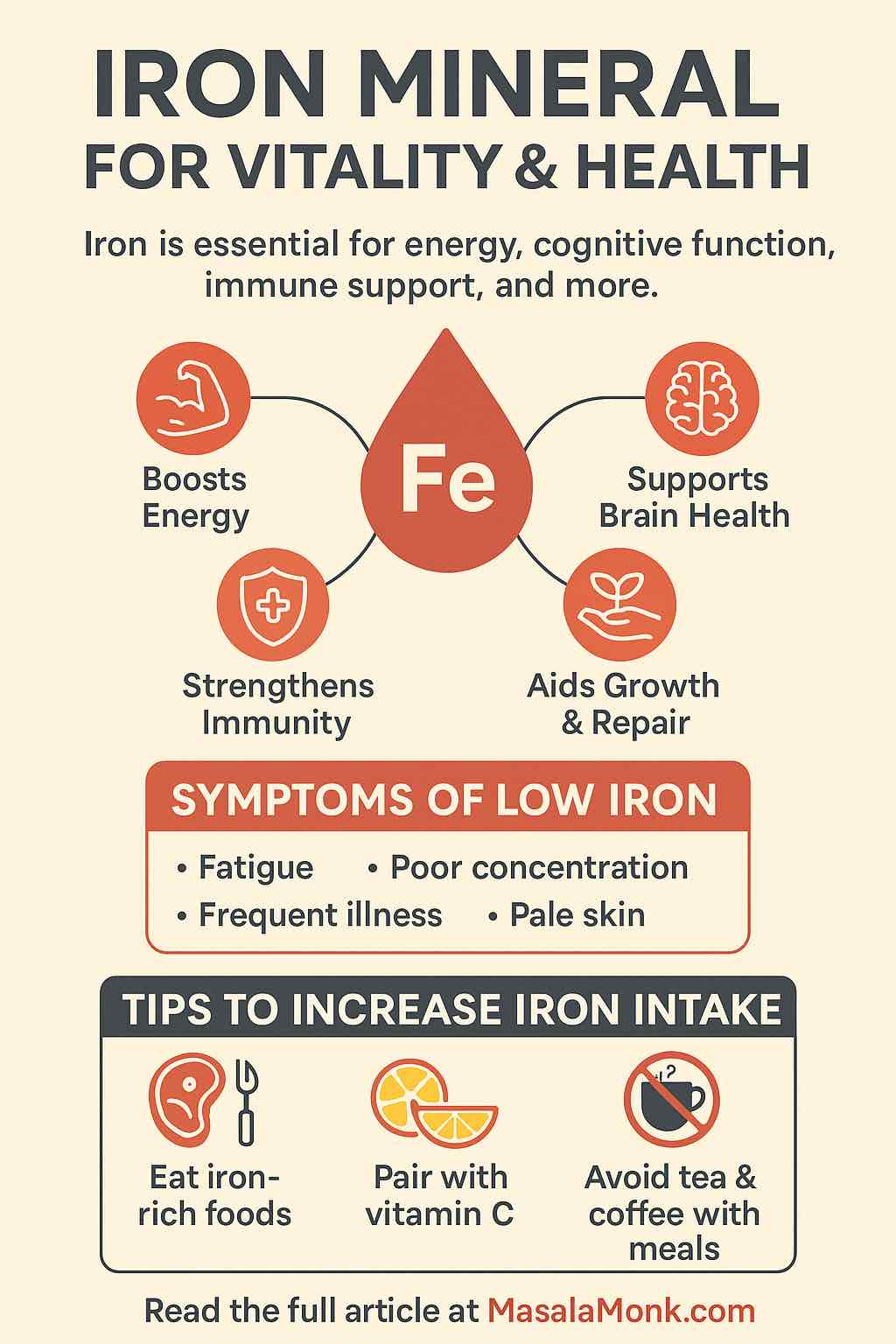
2) Build Iron-Forward Meals First (Then Layer Vitamin C)
Start with staples that genuinely move the needle. Two MasalaMonk primers make this simple:
- Iron-rich vegetables to boost hemoglobin (shop-friendly list)
- Iron: benefits, foods, and how to absorb it better (friendly overview for family buy-in)
What to prioritize, practically:
- Heme iron (absorbs easily): lean beef, chicken, turkey, tuna/salmon; liver if you eat it.
- Non-heme iron (plant & fortified): lentils, beans, chickpeas, tofu/tempeh, pumpkin seeds, spinach, iron-fortified cereals.
- Make room for absorption: keep tea/coffee and large calcium servings (big dairy portions or calcium supplements) away from your iron-focused meal.
Once iron-first habits are in place, add vitamin C to improve plant-iron absorption. For instance, throw tomatoes, citrus, kiwi, strawberries, or peppers into the same meal. To make pairings effortless, skim vitamin C–rich foods and match them to the veg list above.
Do not miss our full post on Iron-Rich Foods for Blood Donation: What to Eat Before & After.
3) Repeat for 2–4 Weeks (Consistency Beats Perfection)
Bodies respond to patterns, not one-offs. Therefore, create a default breakfast and dinner that repeat most days. If drinks are easier, blend a few iron-forward smoothies—see High-iron smoothies to fight anemia for inspiration.
Note: a few MasalaMonk recipes mention pregnancy in the headline. Even though those posts speak to pregnant readers, the food is universal and anyone can borrow the ideas.
4) Consider a Short, Clinician-Guided Iron Supplement
If you donate often, or if your clinician confirms low iron, discuss a time-limited low-dose elemental iron course. Because tolerance and dose are personal, you’ll want to re-check rather than taking iron indefinitely. Meanwhile, keep food doing most of the heavy lifting.
5) Re-Screen and Pace Your Return
When you feel steady, re-screen according to your service’s window. Donation cadence also differs by program. For example, the U.S. Source Plasma rule is two donations in seven days with ≥48 hours between (see CFR §640.65 (PDF) or eCFR §640.65); Lifeblood Australia notes plasma can be given about every two weeks when eligible (What is plasma?). Start with one comfortable session, notice how you feel over the next days, then book the next within your local cadence.
Table 3 — Two-to-four-week food playbook (iron first, absorption smart)
| Meal moment | Iron sources to prioritize | Vitamin-C add-on (boosts absorption) | Timing tip (so iron actually absorbs) |
|---|---|---|---|
| Breakfast | Fortified oats/cereals; eggs; tofu scramble | Citrus, kiwi, strawberries | Keep coffee/tea away from the iron meal; have them mid-morning |
| Lunch | Lentil/bean bowls; chickpea salads; spinach + quinoa | Tomatoes, bell peppers | Avoid large dairy servings with this meal; add yogurt later |
| Snack | Pumpkin seeds; hummus; trail mix with dried apricots | Fresh fruit or cherry tomatoes | If you take calcium supplements, schedule them separately |
| Dinner | Lean beef/chicken/fish; tempeh with legumes | Roast peppers, salsa, lemon/lime squeeze | Leave caffeine for after dinner (or another time) |
| “Drinkable” option | Iron-forward smoothies (spinach + lentils/fortified soy) | Orange/berry base | Sip between meals (not as the only strategy), then re-check Hb |
Consistent meals like these are the fastest, safest way to move hemoglobin up so you can donate plasma with low iron or anemia history without slipping back into a deferral.
Plasma or Whole Blood First? (Choosing the Gentler Way Back)
Whole blood removes red cells; recovery leans harder on iron and usually takes longer. Plasma returns your red cells; the iron impact is smaller. Consequently, many people coming off a borderline result can donate plasma sooner—as long as they pass hemoglobin (and, where used, total protein) checks on the day. If you’re hovering near the threshold, plasma is often the gentler first step back.
Why This Matters for Readers Who Ask “Can You Donate Plasma with Low Iron or Anemia?”
Because the screening is about today’s safety, not just labels. If your hemoglobin is in range, and—where required—your total protein is normal, you may be able to donate plasma with low iron or anemia history as you rebuild. If not, you have a clear, food-first plan; with time, most donors see their numbers rise into the safe zone.
Verify Details for Your Country (One Click Each)
- United States: American Red Cross—eligibility & hemoglobin · CFR §640.65 (PDF)—Source Plasma spacing · eCFR §640.65—live view · eCFR §630.15—donor protein requirement · FDA manual (PDF)
- Canada: Canadian Blood Services—hemoglobin & iron for donors · What is hemoglobin?
- United Kingdom: NHS Blood and Transplant—haemoglobin and iron
- Australia: Lifeblood—What is plasma? · Lifeblood—Iron & donor guidance
- India: DGHS/MoHFW—Guidelines for Voluntary Blood Donation (PDF) · NBTC/NACO—Donor selection circular (PDF)
Helpful MasalaMonk Guides (Internal)
- Iron-Rich Foods for Blood Donation: What to Eat Before & After
- Iron-rich vegetables to boost hemoglobin
- Iron—benefits, foods, and how to absorb it better
- Vitamin C–rich foods
- High-iron smoothies (Food is universal; even if a headline mentions pregnancy, the recipes work for anyone.)
Heads-up: Rules differ by country and can change. This is educational—not medical advice. Check your local blood service and talk to your clinician before donating or taking iron.
FAQs on Donating plasma with low iron or anemia
1) Can you donate plasma with low iron or anemia?
Generally, not today. If your hemoglobin is below the local cut-off, you’ll be deferred. However, once your hemoglobin is back in range—and you feel well—you can usually donate plasma with low iron or anemia history safely.
2) If I’m borderline, when can I donate plasma with low iron or anemia history?
First, rebuild for a few weeks with iron-forward meals and rest. Then, recheck. If your same-day screening meets the threshold, you can move ahead and donate plasma with low iron or anemia history confidently.
3) Can I donate if my iron stores are low but hemoglobin is normal?
Sometimes, yes. Because plasma returns your red cells, centers mainly look at same-day hemoglobin (and sometimes total protein). Nevertheless, if your stores are low, pace donations and focus on rebuilding so you stay eligible.
4) What does “iron levels for plasma donation” actually mean?
Clinics don’t rely on a single “iron number.” Instead, they check hemoglobin/hematocrit (and, in some programs, total protein). Over time, low iron can pull hemoglobin down—so prevention matters.
5) What does my hemoglobin have to be to donate plasma?
It varies by country and program. Even so, the principle is the same: you must be at or above your local minimum on the day of donation. Therefore, aim to sit slightly above the line for comfort.
6) What’s the minimum hemoglobin to give whole blood?
Again, it depends on your country and sometimes on sex. Still, the values are usually close to apheresis screening thresholds. If you’re near the edge, start with plasma once you qualify, then try whole blood later.
7) How can I increase iron levels to give blood (and pass plasma screening)?
Begin with food. Include heme iron (meat/fish/poultry) and non-heme iron (legumes, tofu, greens, fortified cereals). Moreover, pair plant iron with vitamin C, and keep tea/coffee or high-calcium foods away from iron-focused meals.
8) I was deferred—how long before I can donate plasma with low iron or anemia again?
It truly depends on how low you were. Nevertheless, many people improve after 2–4 weeks of consistent iron-forward eating. After that, recheck and, if in range, you can donate plasma with low iron or anemia history safely.
9) Does donating blood cause anemia?
Not by itself, provided you space donations sensibly and replenish iron. However, frequent donations without recovery time can deplete stores and drop hemoglobin.
10) Is donating plasma with low iron or anemia history easier than whole blood?
Often, yes. Plasma returns red cells, so the iron hit is smaller. Consequently, many borderline donors clear plasma screening sooner—provided hemoglobin (and, where used, total protein) is in range that day.
11) Can I donate plasma with low iron if I “feel fine”?
Feeling fine is encouraging; however, donation decisions are based on measurements, not symptoms. If hemoglobin is below the threshold, it’s still “not today.”
12) Can giving blood reduce high iron?
Sometimes, yes—under medical direction. Therapeutic phlebotomy is used for certain iron-overload conditions. Even then, safety thresholds still apply.
13) What should I eat in the weeks before I try to donate plasma with low iron or anemia history?
Prioritize: heme iron sources; legumes and fortified grains; leafy greens; and vitamin-C pairings (citrus, tomatoes, peppers, berries). Meanwhile, hydrate well and keep caffeine or large calcium servings away from iron-centered meals.
14) Do tea and coffee really block iron?
They can blunt non-heme iron absorption when taken with the meal. Therefore, leave a buffer and enjoy them between meals instead.
15) Does calcium affect iron?
Large calcium doses can reduce non-heme iron uptake if taken at the same time. Consequently, separate big dairy portions or calcium supplements from iron-focused meals.
16) Should I take iron pills to increase iron levels to give blood?
Maybe. If you donate frequently or your clinician confirms low iron, a short, low-dose elemental iron course can help. Nevertheless, keep it time-limited and recheck rather than taking iron indefinitely.
17) Can I donate plasma with low iron if my total protein is low?
No. If your program checks total protein and it’s below range, you’ll be deferred. In that case, emphasize overall protein intake while also rebuilding iron.
18) How much does hemoglobin drop after donating?
Expect a modest dip in the days after donation; recovery follows with time, iron-forward meals, and appropriate spacing between sessions.
19) If I was deferred, should I try whole blood or plasma first next time?
If you’re borderline, plasma is usually the gentler first step because red cells are returned. Then, once your numbers are comfortably above the minimum, consider whole blood if you wish.
20) Can you donate plasma with low iron or anemia if you recently had an illness?
It depends on the illness and how you feel now. However, centers will still require that your same-day hemoglobin (and any program-specific tests) are in range, so prioritize recovery first.
21) What daily habits help me get back to donate plasma with low iron or anemia history?
Consistency wins: repeatable iron-forward breakfasts and dinners, vitamin-C pairings, smart timing around tea/coffee and calcium, enough sleep, adequate hydration, and a realistic donation cadence.
22) If I pass screening once, can I donate plasma with low iron or anemia history frequently?
Only if you continue to meet thresholds. Therefore, pace yourself, keep meals iron-positive, and watch for fatigue. If numbers drift down, pause early and rebuild—don’t push through.
23) Do men and women have different cut-offs?
In some countries, yes. Nevertheless, both must meet their local same-day minimum. Thus, verify your jurisdiction’s figure and aim slightly higher for comfort.
24) Does plasma donation affect iron stores at all?
A little. Plasma returns red cells, so the iron impact is smaller than whole blood; even so, multiple sessions without good nutrition can still nudge stores downward over time.
25) Bottom line—how do I get to “yes” and donate plasma with low iron or anemia history?
First, identify what was low. Next, spend a few steady weeks on iron-forward meals (plus vitamin-C pairings and smart timing). Then, if needed, use a short clinician-guided supplement. Finally, recheck; if you’re in range, schedule a plasma session and pace your donations so you stay there.
Important Disclaimer
The information in this article is intended for education only and to help you prepare for donation safely. It does not replace personalized medical advice, examination, or diagnosis. Donation eligibility is set by national services and individual centers, and thresholds (including hemoglobin and total protein) as well as donation frequency differ by country and program. Consequently, always check the current requirements at your local blood/plasma center before booking. Nutrition suggestions here are general; individual needs vary by health status, medications, and life stage. Do not start or stop iron supplements without consulting a qualified healthcare professional. If you experience symptoms such as chest pain, shortness of breath, fainting, or severe fatigue, seek medical care promptly and postpone donation.