Bananas are one of the most widely consumed fruits in the world—and often recommended as a soothing snack for those with digestive issues. But if you’ve ever experienced heartburn or acid reflux after eating a banana, you might be wondering: Are bananas really good for acid reflux, or can they actually make it worse?
In this article, we’ll answer the most common questions people search about bananas and acid reflux, including whether bananas are acidic, why they help some people and hurt others, and what to do if bananas give you heartburn.
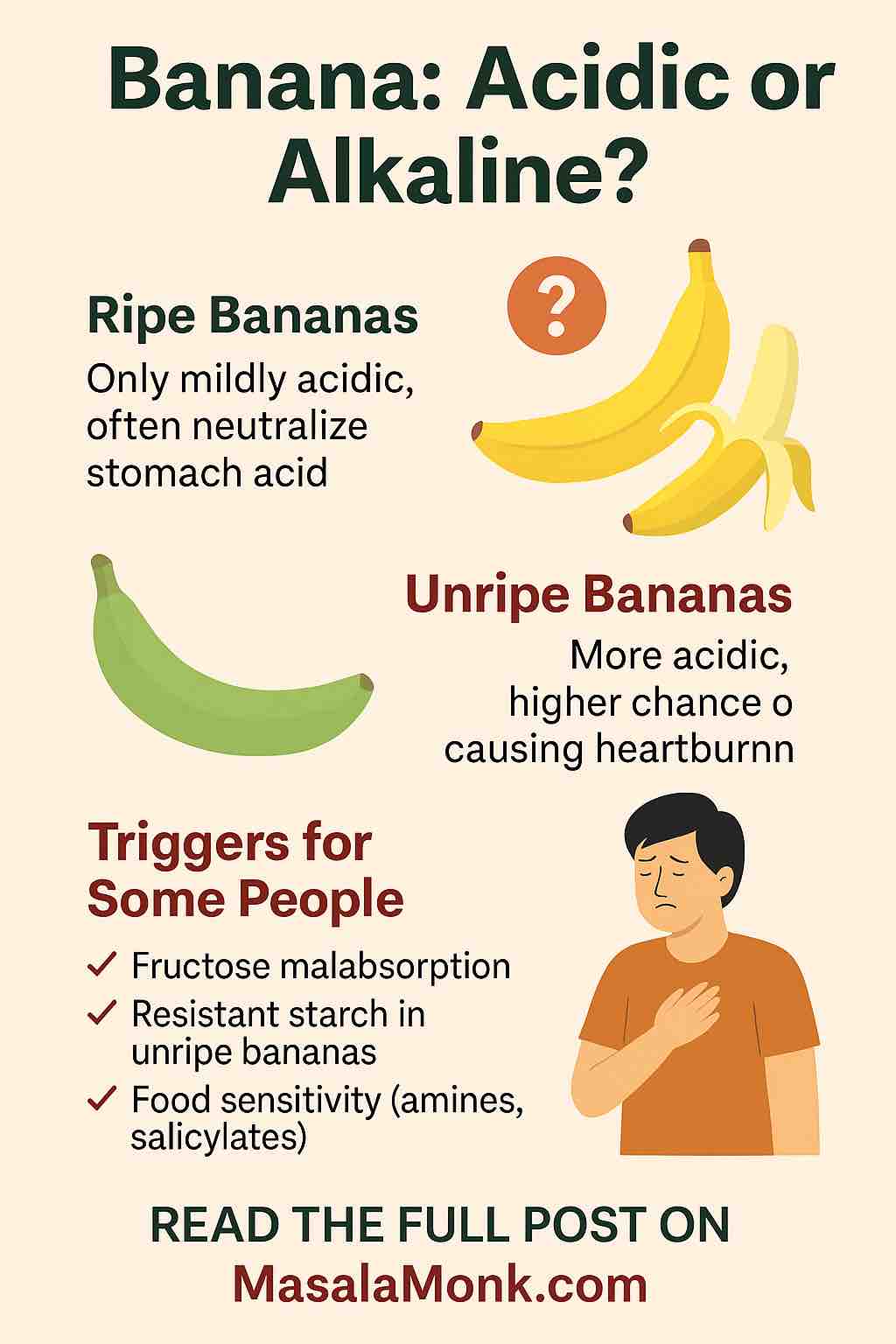
🍌 Are Bananas Acidic or Alkaline?
Despite their taste, ripe bananas are mildly acidic in terms of pH (typically between 5 and 5.5), but they are considered alkaline-forming once digested. This means that while their initial pH is not far from neutral, they help neutralize stomach acid after consumption in many people.
Unripe (green) bananas, however, are more starchy and less digestible, which can sometimes contribute to bloating, gas, and reflux.
✅ Verdict: Ripe bananas are generally low-acid and can be soothing. Unripe bananas may trigger discomfort.
⚖️ Why Bananas Help Some People With Acid Reflux
For many people, bananas act like a natural antacid. Here’s why:
- High Fiber: Bananas contain soluble fiber, especially pectin, which helps food move smoothly through the digestive tract—reducing the risk of acid backing up into the esophagus.
- Natural Mucilage: This gel-like substance coats the stomach lining and esophagus, reducing irritation.
- Prebiotic Properties: Bananas feed beneficial gut bacteria, which can help overall digestion and gut health.
“Bananas are often one of the first fruits recommended for people with GERD.”
🔥 Why Bananas Can Trigger Heartburn in Others
Despite their reputation as a gentle fruit, bananas can cause problems for some people. Here’s why:
- Fructose Malabsorption: Bananas contain natural sugars that may ferment in the gut and cause bloating or reflux in sensitive individuals.
- Unripe Bananas = Resistant Starch: These are harder to digest and can delay gastric emptying, increasing reflux risk.
- Food Sensitivity: A small subset of people may be sensitive to compounds in bananas (such as amines or salicylates), which can trigger symptoms similar to acid reflux or indigestion.
If bananas consistently give you heartburn, it’s not just in your head—there could be a real digestive trigger involved.
❓ Personal Reactions: Why Do You Get Heartburn After Eating Bananas?
If you’re wondering, “Why do bananas give me heartburn?” the answer likely lies in your individual digestive response. Possible reasons include:
- GERD (Gastroesophageal Reflux Disease): Chronic acid reflux means your digestive tract is already sensitive.
- Eating Bananas on an Empty Stomach: For some, bananas increase stomach acid when eaten alone.
- Large Quantities: Overeating bananas (or combining them with other reflux triggers) may worsen symptoms.
✅ How to Eat Bananas for Better Digestion
If you want to keep bananas in your diet without discomfort, try these tips:
- ✅ Eat fully ripe bananas (bright yellow with brown specks).
- ✅ Pair bananas with non-acidic foods like oatmeal, almond butter, or plain yogurt.
- ✅ Avoid bananas on an empty stomach, especially in the morning.
- ✅ Start with half a banana to see how your body reacts.
🚫 When to Avoid Bananas
You may want to avoid bananas—or reduce your intake—if:
- You notice heartburn or reflux after eating them consistently.
- You have active GERD or indigestion symptoms.
- You’re consuming unripe bananas or banana-based processed foods.
Consider alternatives like oatmeal, papaya, or aloe juice—all known for helping acid reflux.
🧪 Science vs. Experience: What Research and Doctors Say
There’s no universal rule about bananas and acid reflux. Most medical sources classify bananas as safe for reflux, but clinical studies are limited.
Doctors often recommend bananas as part of a low-acid, GERD-friendly diet, especially because they don’t relax the lower esophageal sphincter (a common trigger in acidic foods like tomatoes or citrus). But some anecdotal reports—and patients—have noted opposite effects.
📌 Bottom Line: Should You Eat Bananas for Heartburn or Not?
Here’s the simplified answer to all the queries people ask:
| Question | Answer |
|---|---|
| Are bananas acidic? | Slightly, but they are alkalizing in the body. |
| Can bananas cause heartburn? | Yes, in sensitive individuals or when unripe. |
| Are bananas good for acid reflux or GERD? | Often, yes—but not for everyone. |
| Why do bananas give me heartburn? | Possible reasons include unripe bananas, food sensitivity, or gut issues. |
| Should I stop eating bananas? | Not unless you consistently feel worse after eating them. Test and adjust. |
🙋 Frequently Asked Questions (FAQs)
Q: Can bananas cause acid reflux?
A: Yes, in some people—especially if they are unripe or eaten on an empty stomach.
Q: Are bananas good for GERD or heartburn?
A: For many, yes. Ripe bananas are often soothing and non-irritating.
Q: Do bananas have acid?
A: They are slightly acidic (pH ~5), but considered alkaline-forming after digestion.
Q: What fruits are better alternatives for acid reflux?
A: Papaya, melons, and oatmeal are all great, low-acid options.
👍 Final Tip
If bananas work for you, they can be a powerful ally in a reflux-friendly diet. But if they don’t—listen to your body. Diet is not one-size-fits-all.











