Pregnancy is one of the most transformative journeys in a woman’s life — not only emotionally but biologically. Over the course of nine months, a single fertilized cell becomes a full-grown baby with a beating heart, blinking eyes, and tiny fingers and toes. This miraculous transformation unfolds in three distinct trimesters, each marked by unique milestones and critical phases of development.
In this blog post, we will guide you through each trimester, explore the fascinating details of fetal development, and share the latest research that’s reshaping how we understand pregnancy. Whether you’re an expectant parent, healthcare provider, or simply curious about the miracle of life, this post is packed with valuable insights.
🤰 The Three Trimesters of Pregnancy
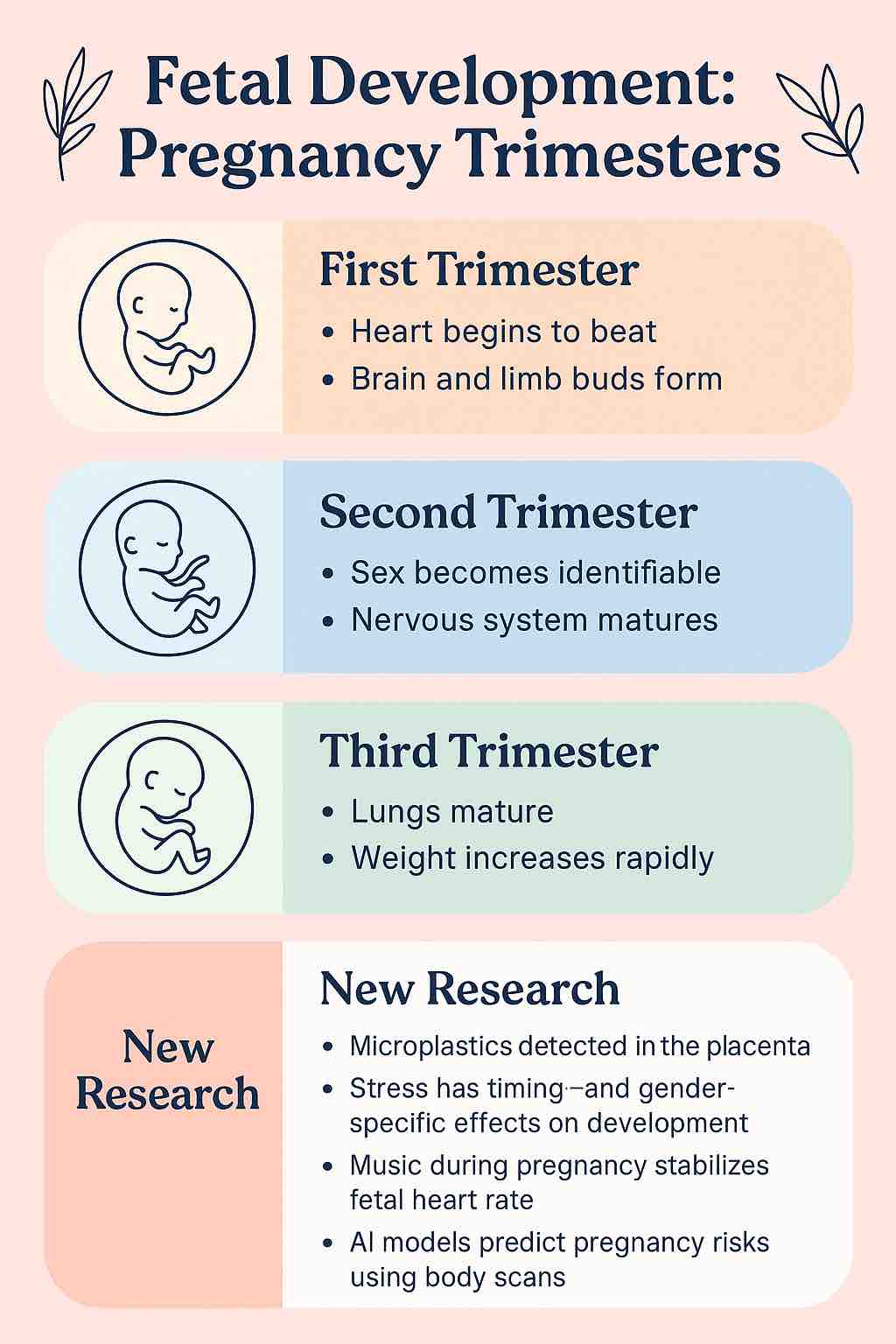
Pregnancy is divided into three trimesters:
- First Trimester: Week 1 to Week 13
- Second Trimester: Week 14 to Week 27
- Third Trimester: Week 28 to Birth (around Week 40)
Let’s explore each trimester in detail.
🌱 First Trimester: The Blueprint of Life (Weeks 1–13)
Highlights:
- Formation of all major organs and systems
- Neural tube, heart, and facial features begin developing
- Baby grows from a zygote to a ~3-inch fetus
🧬 What Happens?
In the first few weeks after conception, cells begin rapidly dividing and forming structures that will eventually become the brain, spinal cord, heart, and limbs. By week 6, the baby’s heart begins to beat — a profound moment for many expectant parents.
🧪 Latest Research:
- Early Biomarkers for Complications: New research has identified that low levels of PAPP‑A and β‑hCG in early blood tests may predict intrauterine growth restriction (IUGR) — giving doctors a chance to intervene early.
- Microplastics Discovered in Placentas: Shocking new findings suggest that microplastics — tiny particles from plastic products — can cross the placental barrier. They’ve even been found in newborns’ first stools, raising concerns about prenatal exposure to environmental toxins.
💡 Tips for This Phase:
- Take prenatal vitamins rich in folate and iron.
- Avoid plastic containers and processed foods to reduce microplastic exposure.
- Get early scans and blood tests to assess fetal health and development.
🌿 Second Trimester: Rapid Growth and First Movements (Weeks 14–27)
Highlights:
- Baby’s sex can often be identified
- Nervous system matures; baby begins to move
- Heartbeat can be heard via Doppler
👶 What Happens?
This is often the most comfortable phase of pregnancy. The baby begins moving around week 18–20 — a sensation known as “quickening.” Eyelids, eyebrows, and fingernails form. The placenta is fully functional, and the baby’s organs continue to mature.
🧠 Latest Research:
- Fetal Brain Development: Using MRI and AI technology, researchers now track brain growth more accurately than ever. The fetal brain doubles in weight and starts forming neural networks for memory and sensory processing.
- Stress Response and Gender: A new study tracking stress weekly from weeks 15–41 found that stress impacts boys and girls differently, depending on when it occurs. This shows how maternal stress timing can shape fetal resilience.
- Music as Therapy: Playing calming classical music like The Swan has been shown to improve fetal heart-rate variability — a sign of healthy autonomic nervous system development.
💡 Tips for This Phase:
- Bond with your baby through music, talking, and gentle belly massages.
- Prioritize mental health — consider yoga, meditation, or therapy to reduce stress.
- Monitor weight and growth via regular ultrasounds.
🌼 Third Trimester: Preparation for Birth (Weeks 28–40)
Highlights:
- Baby gains most of their birth weight
- Lungs and brain mature rapidly
- Baby assumes a head-down position for delivery
🧠 What Happens?
In the final trimester, your baby undergoes finishing touches. The brain develops folds and complexity. The lungs prepare for breathing. Fat accumulates under the skin, and movements become stronger and more coordinated.
🧬 Latest Research:
- Amniotic-Fluid Stem Cells: Scientists can now grow fetal “organoids” (tiny replicas of organs) from amniotic fluid—paving the way for advanced prenatal diagnostics and future regenerative medicine.
- Maternal Chronodisruption: Disruption of sleep patterns and circadian rhythms in pregnant women has been shown to alter fetal metabolic programming, possibly increasing future obesity and diabetes risk.
- AI in Pregnancy Monitoring: Machine learning models now analyze 3D scans of the pregnant belly to predict fetal weight, risk of preeclampsia, and even the possibility of gestational diabetes with remarkable accuracy.
💡 Tips for This Phase:
- Prioritize quality sleep and exposure to natural light.
- Prepare your birth plan and hospital bag.
- Discuss final scans and birth scenarios with your doctor.
🌟 The Role of Nutrition and Epigenetics
Recent breakthroughs in nutriepigenomics reveal that what a mother eats can alter her baby’s gene expression — even before birth.
Key Nutrients:
- Folate: Supports brain and spinal cord development.
- Choline: Critical for cognitive function.
- Calcium: Builds bones and regulates heartbeat.
- Iron: Prevents anemia and supports oxygen supply.
A balanced diet with whole grains, fresh fruits, leafy greens, and protein-rich foods is now seen not just as sustenance — but as a genetic blueprint for lifelong health.
⚠️ Red Flags Across Trimesters
Watch for these warning signs at any point:
- Persistent severe headaches
- Bleeding or leaking fluid
- Sudden swelling in hands/face
- Painful contractions before 37 weeks
- Decreased fetal movement (especially in the third trimester)
Contact your healthcare provider immediately if you notice any of the above.
🧠 Bonus: How Technology is Transforming Prenatal Care
The future of pregnancy care is being shaped by AI, wearable technology, and genetic screening:
- AI-Powered Ultrasound Interpretation
- Non-Invasive Genetic Tests
- Fetal Organ Modeling for Early Diagnosis
- Predictive Algorithms for Preterm Birth
These innovations mean earlier interventions, safer deliveries, and healthier babies.
💬 Final Thoughts
The journey from conception to birth is one of nature’s most intricate and awe-inspiring creations. Understanding the stages of fetal development across trimesters empowers parents to provide the best care and embrace the experience fully.
As science reveals more about what goes on inside the womb, we’re reminded just how interconnected life, health, and the environment truly are.
📚 Ready to Dive Deeper?
Explore more insights, wellness tips, and expert-backed advice on pregnancy and maternal health at MasalaMonk.com.
🤰 Frequently Asked Questions (FAQs)
1. What are the three trimesters of pregnancy and how long do they last?
Answer:
Pregnancy is divided into three trimesters:
- First Trimester: Weeks 1–13
- Second Trimester: Weeks 14–27
- Third Trimester: Weeks 28–40 (or until birth)
Each phase marks key milestones in fetal growth and maternal changes.
2. When does the baby’s heart start beating?
Answer:
The baby’s heart typically starts beating around week 6 of pregnancy, though it may be visible via ultrasound around week 7 or 8.
3. How early can you feel the baby move?
Answer:
Most women feel quickening (the first fetal movements) between weeks 18 and 22, though it may occur earlier in second or third pregnancies.
4. What nutrients are most important during pregnancy for fetal development?
Answer:
Key nutrients include:
- Folic acid – prevents neural tube defects
- Iron – supports oxygen supply
- Calcium – aids bone development
- Choline & DHA – support brain development
5. Can stress during pregnancy affect the baby?
Answer:
Yes. Chronic or severe stress, especially during the second trimester, may affect fetal brain development and stress response, with impacts varying by the baby’s gender and timing.
6. Is it safe to listen to music during pregnancy, and can it help the baby?
Answer:
Yes. Gentle, classical music may calm the fetus, improve heart rate variability, and support autonomic nervous system development — especially in the second trimester.
7. How does sleep affect pregnancy and fetal development?
Answer:
Poor sleep and circadian rhythm disruption in the mother can interfere with fetal organ development, metabolic programming, and increase future health risks for the baby.
8. What are microplastics and why are they a concern in pregnancy?
Answer:
Microplastics are tiny plastic particles found in food, water, and packaging. Studies now show they can accumulate in the placenta and newborn’s body, potentially affecting fetal health.
9. When can you determine the baby’s sex?
Answer:
The baby’s sex can often be seen during the mid-pregnancy ultrasound (anomaly scan), typically done between 18 and 22 weeks.
10. How is AI changing prenatal care?
Answer:
AI helps in early risk prediction (e.g., preeclampsia, gestational diabetes), enhances ultrasound interpretation, and supports 3D fetal imaging, making prenatal care more accurate and personalized.













