If you’re exploring a low histamine diet, you’re likely looking for calm, clear direction—not another rabbit hole of contradicting charts. To make this practical, let’s anchor the essentials in simple cooking habits, walk through a flexible meal pattern, and, importantly, call out where evidence sits today. For balance and credibility, you can skim neutral overviews from the American Academy of Allergy, Asthma & Immunology, check the clinician handout from Johns Hopkins Medicine, and review patient-friendly pages from Allergy UK and the British Dietetic Association as you go. Meanwhile, when you want a concise consumer explainer, the Cleveland Clinic overview is a solid quick read.
Low Histamine Diet Basics: What It Is—and What It Isn’t
To begin with, a low histamine diet is a short-term elimination and re-challenge strategy that reduces foods high in histamine (and some that may liberate histamine) while you observe your own symptoms. Crucially, this approach is not the same as a classic IgE-mediated food allergy. Instead, you’re aiming to lower dietary histamine intake, tighten up food handling, and separate triggers from safe choices by testing them one at a time. In short, you create a peaceful baseline for two to four weeks and then, step by step, you bring foods back.
Furthermore, because histamine levels fluctuate with time and storage, freshness matters as much as the ingredient list. Consequently, simple habits—buying smaller amounts more often, cooking promptly, rapid-chilling leftovers, and rotating meals—do much of the heavy lifting. On balance, you may find the diet less about restriction and more about logistics.
Download the Low Histamine Diet Interactive Tracker (free PDF)—7-day meal plan, fillable shopping list, daily log, and re-intro worksheet—right here.
What to Eat on a Low Histamine Diet (Core “Yes” List)
Proteins (fresh is everything). Choose fresh chicken, turkey, lamb, and eggs; likewise, opt for very fresh white fish cooked the day you buy it. Even so, individual tolerance varies, so you’ll still reintroduce cautiously later.
Carbs & grains (gentle, steady energy). Reach for rice, quinoa, buckwheat, oats, rice noodles, and rice cakes. If you want context about buckwheat’s versatility, scan this short primer on buckwheat benefits—it’s naturally gluten-free and easy to slot into bowls or breakfast porridge.
Vegetables (crisp, quick-cooking choices). Lean on zucchini, carrots, green beans, cucumbers, bok choy, lettuce, and other mild greens (many people sidestep spinach during the elimination phase). Because quick heat helps you avoid long simmer times, sautéing or steaming works beautifully.
Fruit (light and predictable). Apples, pears, and blueberries usually fit early; nevertheless, trial citrus later since it can act as a liberator for some.
Fats (simple and stable). Olive oil is your everyday staple; avocado oil is fine for many, although some people prefer to test avocado itself later.
Drinks (keep it calm). Plain water and gentle herbal teas—ginger, rooibos, peppermint if tolerated—keep hydration easy without complicating the elimination phase.
For a concise, public-facing cross-check, compare your cart with the Histamine Intolerance Food List; and for a helpful “what to expect” overview, see Cleveland Clinic’s guide as well. Meanwhile, if you want a mainstream media digest that echoes many of these items, BBC Good Food’s low-histamine picks are straightforward.
What to Limit First (and Why)
Fermented or aged foods. Soy sauce, vinegar, kombucha, sauerkraut/kimchi, aged cheeses, and cured meats rise to the top of the “hold for later” list.
Alcohol. Wine and beer are frequent irritants during the elimination window.
Seafood that’s canned, smoked, or not cooked promptly. Since histamine can accumulate post-harvest, storage becomes a major factor; fish kept too long, even when cooked later, is a common issue.
Produce commonly flagged as potential liberators. Tomatoes, spinach, eggplant, avocado, and citrus often move into mid-to-late reintroduction instead of day one.
Long-simmered dishes and bone broth. Because amines build with time and temperature, short, bright cooking methods generally suit the elimination phase better than all-day simmering.
All told, the idea is not to demonize foods forever; rather, you’re reducing confounders temporarily. Afterwards, you’ll add items back with intention.
Low Histamine Diet Breakfasts: Fast, Cozy, and Repeatable
To set the tone, start mornings with warm, simple textures and minimal ingredients. In particular:
- Oats with pear and chia. Cook rolled oats in water or a mild non-dairy base; top with diced pear and a spoon of chia. When you want more control over ingredients, consider making your own non-dairy options—this quick explainer on coconut milk nutrition and glycemic impact gives you a sense of how it fits.
- Eggs with sautéed zucchini on toast. Keep the pan hot, cook fast, and season with herbs.
- Chia pudding with apple. For an adaptable method, peek at this chia pudding how-to and simply swap the fruit for something you tolerate early on (e.g., apple or pear).
- Puffed rice “cereal.” Use coconut milk and a sprinkle of pumpkin seeds for crunch without leaning on additives.
Moreover, you’ll notice how often breakfast success comes from short cooking times and rapid cooling. That’s not accidental; those mechanics help you keep amine accumulation low while still eating familiar food.
Snacks, Sweets & “Fun Food” on a Low Histamine Diet
Because snacks can derail plans quickly, it helps to pre-commit to two or three options you actually enjoy:
- Rice cakes with pumpkin-seed butter. Smooth and salty works; add sliced pear if you want contrast.
- DIY oat bars you fully control. This template for healthy oat protein bars is easy to adapt, and when you’re in a rush, these oat bars in 5 minutes keep ingredients tight.
- Light granola. Combine rolled oats, coconut flakes, and pumpkin seeds; toast lightly; store briefly.
- Simple desserts. Baked apples, pears with a hint of olive oil and cinnamon, or a coconut-rice pudding when you want comfort without complexity.
Incidentally, chocolate tends to split audiences during reintroduction, so if you trial it later, do so in tiny amounts and document how you feel.
Low Histamine Diet Cooking & Storage: Tiny Tweaks, Big Wins
Now for the logistics that quietly make the diet work:
Buy smaller amounts more often. Instead of massive shops, pick up just enough meat or fish for a day or two. That way, you’ll naturally cook promptly rather than parking proteins for days.
Cook promptly and cool rapidly. Transfer cooked food into shallow containers and move it into the refrigerator as soon as steam subsides; then, ideally, eat within 24 hours or freeze.
Favor quick methods. Searing, steaming, sautéing, roasting en papillote, and short simmering keep both time and ingredient lists short.
Label and rotate. Even when you’re meticulous, unlabeled containers sabotage the plan. A marker and a roll of tape keep you honest.
Why so fussy? Because histamine is a small, heat-stable molecule—cooking doesn’t reliably destroy it—so your best lever is handling. For a plain-language reminder about storage and histamine formation (especially relevant to fish), skim histamine toxicity basics and you’ll see why these habits matter.
Low Histamine Diet: 7-Day Meal Plan (Mix & Match)
Although individual tolerance differs, this pattern keeps flavors bright and prep times short. Feel free to swap proteins and vegetables across days, and, of course, keep portions aligned to your energy needs.
Day 1
Breakfast: Oats with pear and chia.
Lunch: Poached chicken, quinoa, zucchini and carrot bowl.
Dinner: Pan-seared fresh cod, sweet potato mash, green beans.
Snack ideas: Rice cakes with pumpkin-seed butter; apple slices.
Day 2
Breakfast: Buckwheat porridge with blueberries.
Lunch: Turkey lettuce wraps with cucumber and herbs.
Dinner: Baked lamb meatballs with rice and roasted carrots.
Snack ideas: Coconut yogurt alternative; oat bar square.
Day 3
Breakfast: Scrambled eggs with sautéed courgette; slice of toast (gluten-free if needed).
Lunch: Rice-noodle chicken soup (short simmer; add bok choy at the end).
Dinner: Stir-fried chicken or very fresh prawns with rice and pak choi.
Snack ideas: Pear; rice crackers.
Day 4
Breakfast: Chia pudding (coconut milk) with diced apple.
Lunch: Chicken and rice salad with zucchini ribbons and fresh herbs.
Dinner: Herb-rubbed chicken thighs, quinoa, steamed greens (avoid spinach for now).
Snack ideas: Blueberries; pumpkin seeds.
Day 5
Breakfast: Puffed rice with coconut milk and pumpkin seeds.
Lunch: Lamb and sweet potato bowl with green beans.
Dinner: White fish en papillote with rice and carrot coins.
Snack ideas: Rice cakes; cucumber slices with olive oil and salt.
Day 6
Breakfast: Oat pancakes (trial banana later if you suspect it’s a trigger).
Lunch: Egg fried rice with finely diced zucchini (use day-old rice that was chilled promptly).
Dinner: Roast turkey breast, buckwheat, and a leafy salad (choose non-spinach greens).
Snack ideas: Baked apple; small oat bar.
Day 7
Breakfast: Eggs, rice cakes, and cucumber.
Lunch: Quinoa “tabbouleh-style” (skip tomato for now), plus sliced chicken.
Dinner: Quick chicken stew (short simmer), sweet potato, tender carrots.
Snack ideas: Pear; a few pumpkin seeds.
Naturally, you’ll adjust seasoning to taste—think fresh parsley, chives, dill, or a squeeze of non-citrus brightness (e.g., a splash of mild vinegar only during reintroduction if tolerated). Until then, rely on herbs, garlic-infused oil if whole garlic bothers you, and a confident hand with salt.
Grab the Low Histamine Diet Interactive Tracker (free PDF) with a 7-day meal plan, fillable shopping list, and re-introduction log – Download Here.
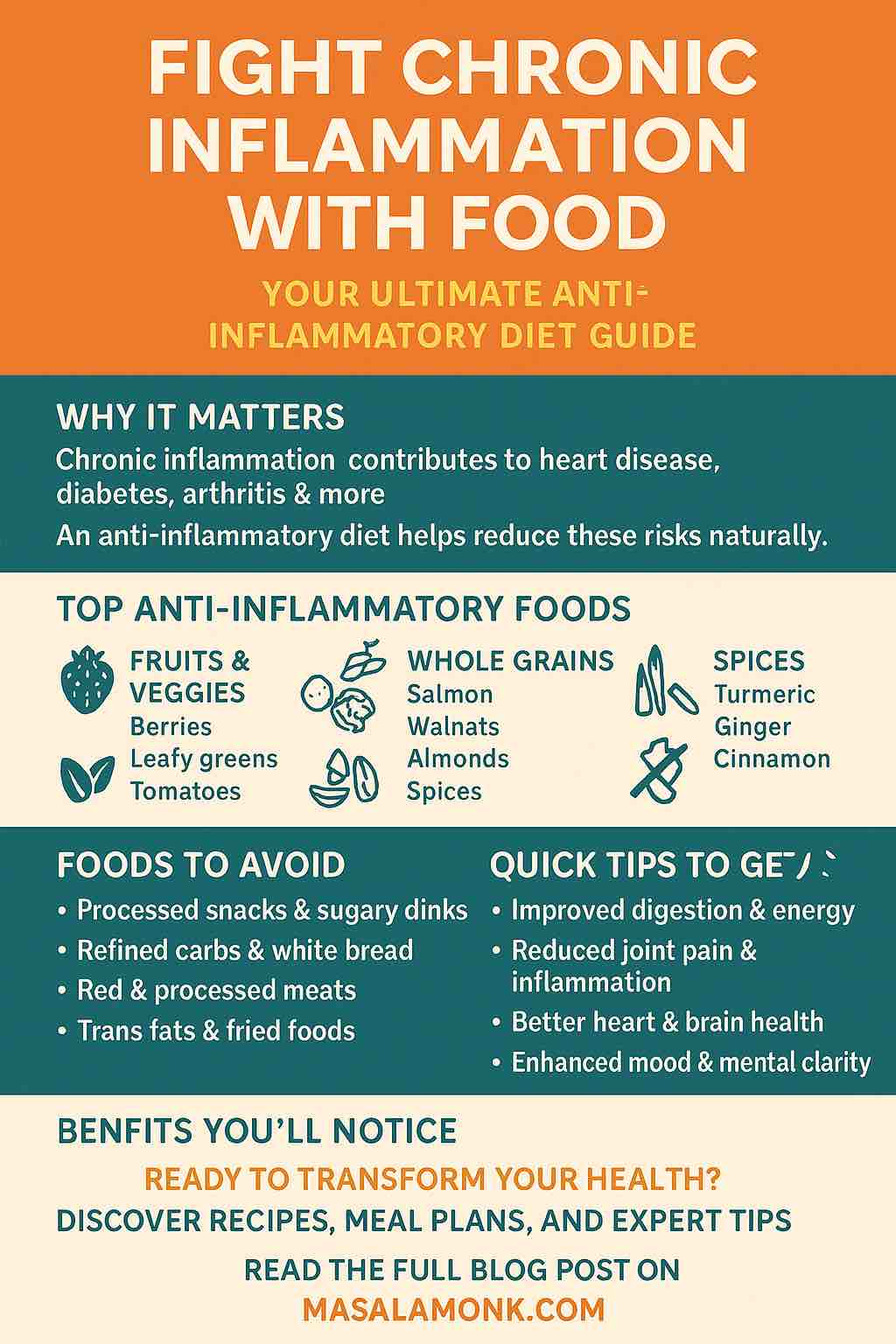
Low Histamine Diet × Anti-Inflammatory Eating: How to Blend Without Stress
Because many readers are also trying to reduce background inflammation, it helps to build plates around lean protein + colorful vegetables + gentle carbs + olive oil. Beyond that, consider polyphenol-rich fruit such as blueberries if you tolerate them. Notably, while fermentation can improve nutrient availability in some contexts, the early days of a low histamine diet emphasize unfermented choices first. Later—once you’ve stabilized—you’ll reintroduce candidates gradually and keep what loves you back.
For newcomers who want a conventional medical voice alongside this plan, the Cleveland Clinic introduction is a handy companion; and for a concise checklist you can cross-verify, the Histamine Intolerance UK food list is easy to scan. Meanwhile, keep your own notes—what you ate, when you stored it, how you felt—since your tolerance is the final referee.
Low Histamine Diet Breakfast Variations (So You Never Get Bored)
Even with a tight ingredient set, breakfast can feel fresh day after day. Consider these rotations:
- Oats three ways. Classic porridge; oven-baked oat squares; or overnight oats in a non-dairy base. For a controlled approach to snacks that double as breakfast, tweak healthy oat protein bars to your tolerance.
- Eggs beyond scrambled. Poached on quick-sautéed greens; omelettes with fine-diced zucchini; or frittata cups baked for 12–15 minutes for fast weekday reheats.
- Buckwheat porridge and pancakes. Soft, nutty, and easy to digest, buckwheat performs well in both sweet and savory directions; for background, skim this buckwheat overview and adapt freely.
- Chia pudding two ingredients at a time. A spoon of chia plus a mild base and a small fruit portion—this chia method is a template you can strip down and rebuild without fuss.
Meanwhile, remember that repetition in structure doesn’t mean monotony in taste; herbs, textures, and plating can carry variety even before you reintroduce more adventurous items.
Low Histamine Diet: Smart Flavor Without Ferments
At first glance, removing ferments looks like removing flavor. Nevertheless, you can still cook boldly:
- Fresh herb pastes. Blend parsley, dill, or cilantro with olive oil and a pinch of salt; freeze in small portions for instant brightness.
- Allium strategy. If whole garlic or onion bothers you, use garlic-infused oil for aroma without the same compounds that trouble some people.
- Crunch and contrast. Pair soft grains with crisp vegetables; add pumpkin seeds or cucumber ribbons to keep each bite interesting.
- Heat control. Sear meats quickly for browning, then finish gently to avoid extended cook times.
In practice, these techniques make “simple” food taste restaurant-level, which makes adherence easier while you figure out your unique tolerance.
Low Histamine Diet: How to Re-Introduce Foods Confidently
Once you’ve had a quiet baseline for two to four weeks, reintroduce foods one by one. To that end:
- Pick one candidate (e.g., tomato). Eat a small portion at one meal.
- Wait 48–72 hours, noting symptoms as well as sleep, stress, and storage variables.
- Increase portion if day one went well.
- Decide: keep, limit, or postpone.
To stay grounded in cautious, evidence-aware advice while you test, a neutral synthesis from the British Dietetic Association helps temper expectations, and the Allergy UK explainer offers practical reminders. Notably, divergent opinions in the literature are normal; your day-to-day response trumps theory.
DAO, Supplements & “Foods That Help”: A Balanced View
Your small intestinal enzyme diamine oxidase (DAO) degrades dietary histamine; thus, you’ll see supplements marketed as a quick fix. However, while some people report benefits, formal evidence and testing standards are still evolving. Accordingly, treat supplements as adjuncts, not anchors. If you want to read an allergy specialist’s cautionary note in plain language, try this DAO Q&A from AAAAI; then, if you experiment, change only one variable at a time so you can tell what helped.
As for “antihistamine foods,” nutrients like vitamin C and polyphenols are interesting, and yet, the basics still win: fresh food, tidy storage, short cooking times, and consistent meal patterns. Consequently, the plan above does more good than hunting for a magic ingredient.
Low Histamine Diet Troubleshooting: When Something Feels Off
Despite best efforts, you may hit snags. If symptoms persist, widen the lens:
- Check storage and timing. Even a “safe” food can feel unsafe if it lingered too long.
- Evaluate stress and sleep. Mast-cell behavior isn’t isolated from the rest of your life.
- Consider overlap with other GI patterns. Some people run a low histamine diet alongside low-FODMAP for a short, supervised window; if that’s you, a cautious, clinician-guided approach is wise.
- Rule out mimickers. True food allergy, celiac disease, and inflammatory bowel disease deserve medical evaluation when symptoms are significant.
Parallel to this, precise, trustworthy resources keep you grounded. Keep Cleveland Clinic’s overview and the BDA guidance bookmarked for readers who want a conventional lens.
Closing Thoughts: Calm Food, Clear Decisions
Ultimately, a low histamine diet is less about memorizing an encyclopedic list and more about running a clean, fair experiment. First, simplify meals and tighten storage. Next, listen to your body for two to four quiet weeks. Finally, bring foods back systematically and keep the ones that love you back. Meanwhile—and this is the part many people skip—stay flexible. Your goal isn’t a permanent cage; it’s a personal map.
If you keep that spirit, you’ll find this way of eating not only tolerable but surprisingly freeing: fewer variables, fewer surprises, and more breakfasts, lunches, and dinners that feel like you—steady, satisfying, and refreshingly uncomplicated.
Ready to use? Download the Low Histamine Diet Interactive Tracker (free PDF)—7-day meal plan, fillable shopping list, daily log, and re-intro worksheet—right here.
FAQs
1) What is a low histamine diet?
A low histamine diet is a short-term elimination and re-challenge approach that reduces high-histamine foods and potential “liberators,” then gradually reintroduces them to identify personal tolerance.
2) How long should I follow a low histamine diet before reintroducing foods?
Typically 2–4 weeks of a calm baseline works well; subsequently reintroduce one item every 2–3 days while tracking symptoms, sleep, stress, and storage habits.
3) Which foods are best to eat on a low histamine diet?
Emphasize fresh chicken or turkey, eggs, very fresh white fish, rice, quinoa, buckwheat, oats, zucchini, carrots, green beans, lettuce, apples, pears, blueberries, and olive oil.
4) Which foods should I avoid at first on a low histamine diet?
Initially sidestep fermented and aged items (soy sauce, vinegar, sauerkraut, aged cheese, cured meats), alcohol, canned or smoked fish, long-simmered stews, and common liberators like tomato, spinach, eggplant, avocado, and citrus.
5) What are histamine liberating foods?
They’re foods that may prompt your body to release histamine even if the food itself isn’t high in histamine; examples often include citrus, tomato, spinach, eggplant, and avocado.
6) What does a simple low histamine diet meal plan look like?
Build each plate with fresh protein, a gentle carb (rice, quinoa, buckwheat, oats), half a plate of mild vegetables, and olive oil; rotate options through seven days to keep variety.
7) What are easy low histamine breakfast ideas?
Think warm oats with pear, eggs with sautéed zucchini, chia pudding with apple, and puffed rice with a non-dairy base and pumpkin seeds.
8) Are bone broth and long-simmered soups okay on a low histamine diet?
Generally not during elimination; as cooking time lengthens, biogenic amines tend to rise. Prefer quick soups or short simmers, then test longer cooks later.
9) Can I have yogurt, cereal, crackers, granola, or protein bars?
Fermented dairy yogurts are usually high; consider non-dairy alternatives first. Choose plain oats or puffed rice for cereal, simple rice/oat crackers, light DIY granola, and homemade bars with minimal additives.
10) How should I handle leftovers to keep histamine lower?
Cook promptly, cool rapidly in shallow containers, refrigerate early, and eat within 24 hours or freeze. Moreover, label dates so rotation stays tight.
11) Can a low histamine diet be combined with low FODMAP?
Yes, for a short, guided window. Select overlapping “safe” foods from both patterns, keep recipes simple, and stage reintroductions to avoid confounding results.
12) Do DAO supplements or “DAO foods” help on a low histamine diet?
They might assist some people, though evidence is mixed. Treat them as optional adjuncts; first optimize freshness, storage, and structured reintroductions.
13) Are there “antihistamine foods” that reduce symptoms?
Nutrients like vitamin C and polyphenols are discussed, yet no single food is a cure. Consistently low-histamine patterns plus careful prep tend to matter more.
14) What about chocolate, coffee, and tea?
Chocolate often triggers people and is best tested later in tiny amounts. Coffee and tea vary by individual; trial cautiously and note dose, timing, and any symptoms.
15) How do I reintroduce foods on a low histamine diet without confusion?
Select one food, try a small portion once, wait 48–72 hours, then increase if tolerated. Keep notes, avoid adding two new items together, and decide to keep, limit, or pause.
16) What are good low histamine snacks and sweets?
Rice cakes with pumpkin-seed spread, fruit like apples or pears, light oat bars you control, simple granola, baked apples, and coconut-rice pudding are reliable starters.
17) Is fish allowed, and if so, which types?
Yes—choose very fresh white fish and cook the same day. Conversely, avoid canned, smoked, or long-stored fish during elimination.
18) Can I follow a vegetarian or vegan low histamine diet?
Absolutely, though protein variety requires planning. Center plates on eggs (if included), quinoa, buckwheat, oats, rice, and tolerated seeds; then stage legumes later if needed.
19) Will a low histamine diet help mast-cell–related symptoms?
It may help some people by reducing dietary triggers; nevertheless, consider it supportive, not curative, and coordinate with your clinician for comprehensive care.
20) What’s the single most important success tip for a low histamine diet?
Prioritize freshness over perfection: buy smaller quantities, cook quickly, cool fast, and reintroduce foods with intention so your long-term pattern fits your life.