Intermittent fasting (IF) has exploded in popularity, promising everything from sharper mental focus to rapid fat loss. But for millions, its most life-changing benefit might be improved blood sugar regulation—the key to preventing diabetes, boosting energy, and enjoying more stable moods throughout the day. If you’re navigating prediabetes, diabetes, or simply aiming to optimize your metabolism, this is a topic that matters.
But does the hype live up to the reality? What do real people—beyond the clinical studies—experience when they use IF for blood sugar control? And what practical strategies make IF work (and stick) in daily life?
This blog post is your deep dive into both the latest science and the voices from the frontlines: people like you, sharing their struggles and successes on forums and social media. Whether you’re a seasoned faster or just IF-curious, you’ll find a roadmap for safer, smarter, and more sustainable blood sugar management.
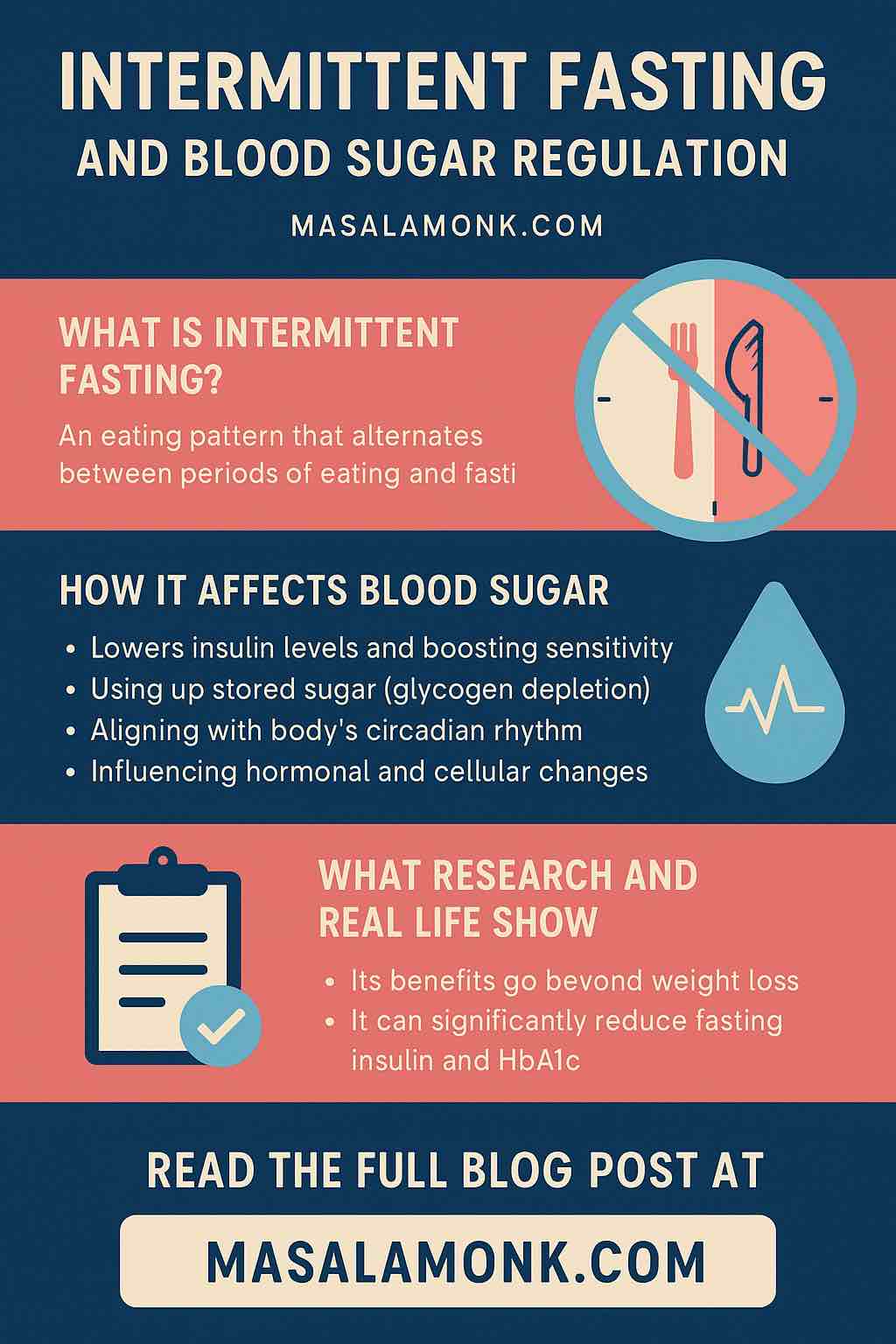
What Is Intermittent Fasting? A Quick Recap
At its core, intermittent fasting is not about “what” you eat, but “when.” Instead of spreading food evenly over 16 waking hours, IF alternates periods of eating with longer periods of fasting—ranging from a few hours to a few days, depending on the method. The most common IF styles include:
- 16:8: Fast for 16 hours (typically overnight), eat all meals within an 8-hour window.
- 5:2: Five days of normal eating, two non-consecutive days with caloric intake around 500–600 calories.
- Alternate-Day Fasting (ADF): Fast every other day, or alternate low-calorie and normal days.
- Time-Restricted Eating (TRE): Eat all meals within a 6–12-hour window, with variants such as early TRE (all food before 5pm).
- One Meal a Day (OMAD): A single meal within a 1–2 hour window, fasting the rest of the day.
What draws many to IF isn’t just weight loss. It’s the hope that by giving the body regular breaks from food, we can “reset” insulin sensitivity, lower blood sugar, and protect long-term metabolic health.
Why Blood Sugar Regulation Is Essential (for Everyone)
Blood sugar—the amount of glucose in your blood—is your body’s core energy currency. Every cell, from your brain to your muscles, depends on a steady supply. If your blood sugar yo-yos too much or stays high for too long, it can result in:
- Fatigue, brain fog, and irritability
- Weight gain and cravings
- Inflammation and cellular stress
- Progression to insulin resistance, prediabetes, and eventually Type 2 diabetes
- Increased risks for heart, eye, and kidney disease
Whether or not you’ve been diagnosed with a blood sugar disorder, almost everyone can benefit from a more stable glucose profile. That’s where IF comes in—not as a magic bullet, but as a tool to help your metabolism work with you, not against you.
How Intermittent Fasting Impacts Blood Sugar: The Science Explained
1. Lowering Insulin Levels and Boosting Sensitivity
Insulin is the hormone that helps cells absorb glucose from the blood. Constant eating—especially processed carbs and sugary snacks—forces your body to release insulin over and over. Over time, this can make cells less sensitive, causing your body to pump out even more insulin and leading to chronically high blood sugar.
Fasting gives your body a much-needed break. During a fasting window, insulin drops, and your cells become more receptive—helping to restore normal blood sugar and even “reset” metabolic pathways.
2. Using Up Stored Sugar (Glycogen Depletion)
Between meals and during overnight fasts, your body switches from burning fresh dietary sugar to tapping into stored glucose (glycogen) in the liver and muscles. IF extends this window, forcing your body to use more stored energy. When glycogen runs low, your body may turn to fat for fuel, which can also improve insulin sensitivity over time.
3. Circadian Rhythm Synergy
Mounting research suggests that aligning food intake with your body’s natural clock (circadian rhythm) enhances benefits. Insulin sensitivity peaks in the morning and tapers off by evening. Eating earlier in the day and avoiding late-night meals (e.g., with early TRE) can help keep blood sugar more stable.
4. Hormonal and Cellular Changes
Beyond insulin, IF influences hormones like leptin (which tells your brain you’re full), ghrelin (hunger hormone), and adiponectin (which improves insulin sensitivity). Cellular “autophagy”—the process of cleaning out damaged cells—also ramps up during fasts, supporting better metabolic health and glucose control.
The Latest Research: What We Know in 2025
Clinical Trials and Meta-Analyses:
- A 2025 clinical trial of people with Type 2 diabetes found that all forms of IF (including 5:2, 16:8 TRE, and alternate-day fasting) led to significant reductions in fasting blood glucose and HbA1c—a key long-term blood sugar marker.
- 5:2 intermittent fasting produced the largest improvements in insulin sensitivity and adherence, even outperforming standard calorie-restricted diets in real-world settings.
- Six-month interventions saw A1c drops of 0.8 percentage points (a major change for diabetes management), and average fasting glucose reductions of 20–30 mg/dL.
- Early time-restricted eating (e.g., 8am–4pm) showed especially strong overnight glucose reductions, helping to control the “dawn phenomenon” (early morning blood sugar spike).
Mechanisms Confirmed in the Lab:
- IF improves insulin sensitivity not only by weight loss, but by directly affecting how your body processes sugar and fat.
- Fasting periods modulate the gut microbiome and reinforce natural daily hormone rhythms, both of which contribute to more predictable blood sugar.
Real-Life Successes and Struggles: Stories from Reddit & Forums
Scientific trials offer averages—but your mileage may vary. Real people’s stories provide a nuanced, practical look at IF’s effects on blood sugar. Here’s a collection from Reddit, diabetes forums, and health communities:
1. Life-Changing Remission and A1c Drops
“I did alternate day 24 hour fasts…The longest I got was an 88 hour fast, which I broke because my sugar dropped below 70. …I am currently down 130 lb…My A1C has been in the 4.7–5.0 range for the last 2½ years. …My diabetes is essentially gone.”
— r/intermittentfasting
Another member of r/diabetes_t2 writes:
“I started with an A1C of 10.7 and hover around 5 now…pair this with a low-carb diet or keto and you will be fine. It has kept me off all medications and HbA1c below 5 for two years and counting.”
2. Struggles and Adjustments
“My blood sugar is ALWAYS higher when doing IF. …I stopped doing it because my body rejected it and I did not see any benefits.”
— r/prediabetes
Another shares:
“When I’m eating 4 small meals a day my sugar comes back down FAST…If I do IF focused eating later… I’ve seen spikes at 2 am!!”
A common concern is the “dawn effect”—your liver releases sugar in the early morning, sometimes causing higher fasting blood glucose, especially if fasting windows are long or poorly timed.
3. Adaptation, Dawn Effect, and CGM Use
A user explains:
“Dr told me…after 12 hours fasting glucose goes up. Liver releases glucose. Survival mode. Try again 8 or 10 hours…you might be fine.”
Another user notes:
“When I’m well into a fast (16 hours) my sugar can get into the mid-60s…and I don’t have symptoms.”
Takeaway: Most successful IF practitioners experiment with fasting lengths, monitor their blood sugar with a meter or CGM, and adjust windows/timing to fit their unique physiology.
Building Your Personal IF Plan for Blood Sugar Success
1. Choose a Protocol That Fits Your Life
Start simple—perhaps with a 12:12 schedule (12 hours fasting, 12 hours eating), then progress to 14:10 or 16:8. If you’re motivated and medically supervised, experiment with the 5:2 or alternate-day approaches.
2. Time Your Eating Window for Maximum Benefit
Aim to eat your meals earlier in the day, when your body is naturally more insulin sensitive. For most, an eating window between 7am and 5pm works well—avoid eating late at night.
3. Focus on Food Quality During Eating Windows
IF is not a license for junk food. Focus on lean proteins, healthy fats, whole grains, and lots of fiber-rich veggies. Minimize processed carbs and sugary drinks, which can spike blood sugar.
4. Hydrate Generously
Drink water, herbal teas, or black coffee during your fasting period. Proper hydration reduces hunger and helps your body manage metabolic shifts.
5. Monitor Your Blood Sugar (Especially If Diabetic or Prediabetic)
Track how different fasting windows affect your fasting, post-meal, and overnight glucose. If you use insulin or medication, consult your healthcare provider before starting IF.
6. Adjust Based on Your Results
If you notice high morning glucose (dawn effect), try a shorter fast, move your eating window earlier, or add a small protein-based snack before bed. If you feel weak or dizzy, break your fast gently and reassess.
7. Prioritize Sleep and Stress Management
Poor sleep or chronic stress can spike blood sugar regardless of your diet. Pair IF with a regular sleep routine and stress-reducing habits.
Realistic Day-in-the-Life: IF for Blood Sugar Control
Meet “Maya,” age 45, diagnosed with prediabetes after years of erratic eating.
- Phase 1: Starts with a gentle 12:12 fast, eating breakfast at 7:30am and dinner at 7:30pm. Tracks fasting and post-meal glucose.
- Phase 2: Moves to 14:10 (8:30am–6:30pm) after two weeks, feeling less hungry in the mornings.
- Phase 3: After a month, shifts to 16:8, eating from 10am–6pm. She plans all meals to be protein and fiber-rich, avoids nighttime snacking, and walks after dinner.
Results after 3 months:
- Fasting glucose drops from 118 mg/dL to 100 mg/dL
- A1c falls from 6.0% to 5.5%
- Sleep and energy improve; cravings decrease
Troubleshooting: Common Challenges & Solutions
Hunger Pangs Early On:
Normal for the first week or two. Hydrate, stay busy, and don’t over-restrict calories during eating windows.
High Morning Blood Sugar:
Shorten the fasting window or shift it earlier. Try a small, protein-rich bedtime snack.
Plateauing Results:
Assess whether hidden sugars or snacks have crept in. Try a different IF protocol or adjust meal composition.
Social & Family Pressure:
Plan meals with family inside your window, bring fasting-friendly snacks, or practice flexible fasting on special occasions.
Medication Use:
Never start IF if you’re on glucose-lowering medication without consulting your healthcare provider. Monitor closely and adjust medication as needed.
Lessons from Real People
- IF can deliver dramatic results—weight loss, lower A1c, diabetes remission—but it’s not always a smooth ride.
- Some struggle with hunger, morning glucose spikes, or plateaus. Others breeze through with only minor adjustments.
- The key is customization: The “best” fasting window is the one that fits your schedule, biology, and goals.
Final Thoughts
Intermittent fasting is a powerful, flexible tool for blood sugar control. Backed by strong science and the lived experience of thousands, IF offers a pathway to better health that doesn’t require constant calorie counting or complicated rules. Yet, it’s not a “one size fits all” strategy—success means experimenting, monitoring, and personalizing your approach.
If you’re ready to try IF, start slow, pay attention to your body, and use blood sugar as your most honest feedback tool. Over time, you might find yourself with more energy, clearer thinking, and—most importantly—a much healthier metabolic future.
Share your own IF experiences or questions in the comments! Your journey could inspire others who are just starting out.
FAQs: Intermittent Fasting and Blood Sugar
1. Can I do intermittent fasting if I have Type 2 diabetes?
Yes, but you must consult your healthcare provider first, especially if you take insulin or blood sugar–lowering medications. IF can improve blood sugar, but medication doses may need to be adjusted to prevent low blood sugar (hypoglycemia).
2. Will intermittent fasting cause my blood sugar to drop too low?
Some people—especially those on certain diabetes medications—can experience hypoglycemia during fasting. It’s important to monitor blood glucose closely and break your fast if you feel weak, dizzy, or have other symptoms of low blood sugar.
3. What is the best intermittent fasting schedule for blood sugar control?
Early time-restricted eating (e.g., 8 am–4 pm or 9 am–5 pm) often works best for stable blood sugar, but the ideal window varies by individual. Many benefit from a 14:10 or 16:8 approach.
4. Can I drink coffee or tea while fasting?
Yes, plain black coffee, unsweetened tea, and water are allowed during fasting periods. Avoid adding sugar or high-calorie creamers.
5. What should I eat during my eating window to support blood sugar control?
Focus on fiber-rich veggies, lean protein, healthy fats, and whole grains. Limit processed carbs, added sugars, and sugary drinks.
6. Why is my morning blood sugar sometimes higher after fasting?
This is called the “dawn phenomenon”—your liver releases glucose in the early morning. If it persists, try a shorter fasting window or shift your eating period earlier in the day.
7. Do I have to count calories while doing intermittent fasting?
Not necessarily. Many people naturally eat less with IF, but if your blood sugar isn’t improving or you’re not seeing results, tracking intake for a week or two may help identify hidden calories.
8. Will I lose muscle while intermittent fasting?
If you consume enough protein and maintain strength-based exercise, you can preserve (or even gain) muscle mass while fasting.
9. How quickly will I see improvements in my blood sugar?
Some see improvements within 2–4 weeks, but meaningful reductions in HbA1c (a 3-month average of blood sugar) may take 2–3 months or longer.
10. Is intermittent fasting safe long-term?
For most healthy adults, yes—especially if it’s flexible and not extreme. However, pregnant women, children, and people with a history of eating disorders should avoid IF unless advised by a physician.









