When it comes to natural skincare, garlic might not be the first ingredient that comes to mind. Yet for centuries, this humble kitchen staple has been celebrated not just for its robust flavor and medicinal value, but also for its profound impact on skin health. Whether you’re dealing with acne, dullness, pigmentation, or early signs of aging, garlic offers a host of topical benefits that modern science is just beginning to explore.
In this detailed guide, we reveal how garlic works wonders on your skin, how to use it safely, and why it’s becoming a cult-favorite among natural skincare enthusiasts.
🔬 Why Garlic Deserves a Spot in Your Skincare Routine
Garlic (Allium sativum) is rich in bioactive compounds and essential nutrients that provide anti-inflammatory, antimicrobial, antioxidant, and detoxifying effects on the skin.
Nutritional Powerhouse in Garlic:
- Allicin: A sulfur-rich compound known for its antibacterial, antiviral, antifungal, and anti-inflammatory properties. It’s the main player in garlic’s topical effectiveness.
- Selenium: A trace mineral that plays a vital role in skin elasticity and reduces oxidative stress.
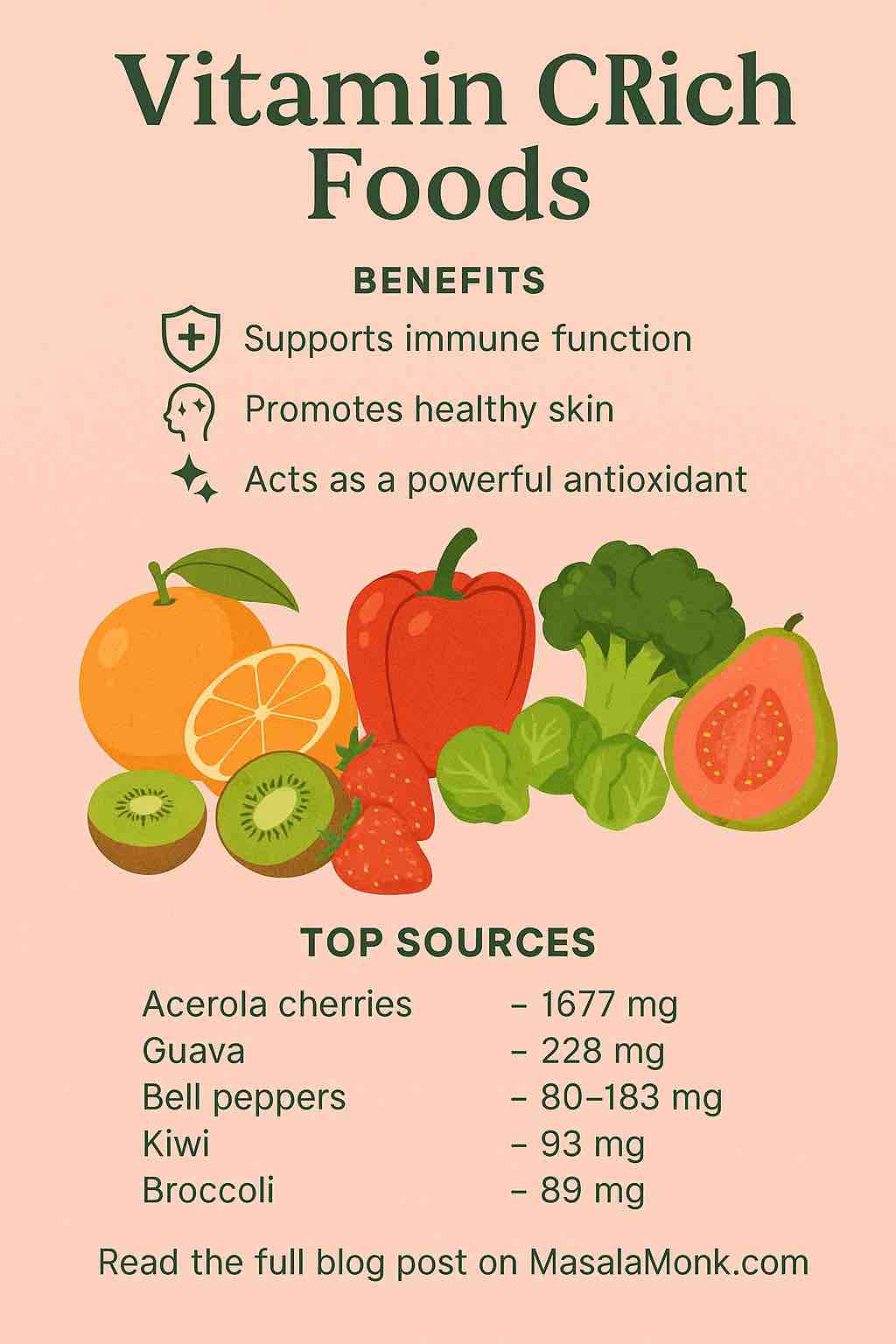
- Vitamin C: Supports collagen synthesis, helping maintain skin firmness and texture.
- Zinc & Copper: Assist in wound healing and improve skin clarity.
- Polyphenols: Combat oxidative damage and delay signs of aging like wrinkles and sagging.
✨ What Garlic Can Do for Your Skin
✅ 1. Acne and Blemish Control
Garlic’s antimicrobial effects target acne-causing bacteria such as Propionibacterium acnes. Allicin, along with garlic’s natural anti-inflammatory properties, helps reduce redness, swelling, and pus formation. Its ability to control oil secretion also contributes to fewer breakouts.
Pro Tip: Mix one crushed garlic clove with aloe vera gel and apply it directly to acne spots. Leave on for 10 minutes, then rinse with lukewarm water. Repeat 2–3 times a week.
✅ 2. Skin Brightening and Complexion Enhancement
If you’re wondering how to use garlic for skin whitening, the answer lies in its detoxifying effect. Garlic improves blood circulation and removes toxins, which naturally leads to a brighter, healthier-looking complexion. Over time, it can help reduce pigmentation and uneven skin tone.
DIY Brightening Mask: Blend garlic juice with honey and a pinch of turmeric. Apply to face for 15 minutes, then rinse. Use once a week.
✅ 3. Reduces Inflammation and Skin Sensitivity
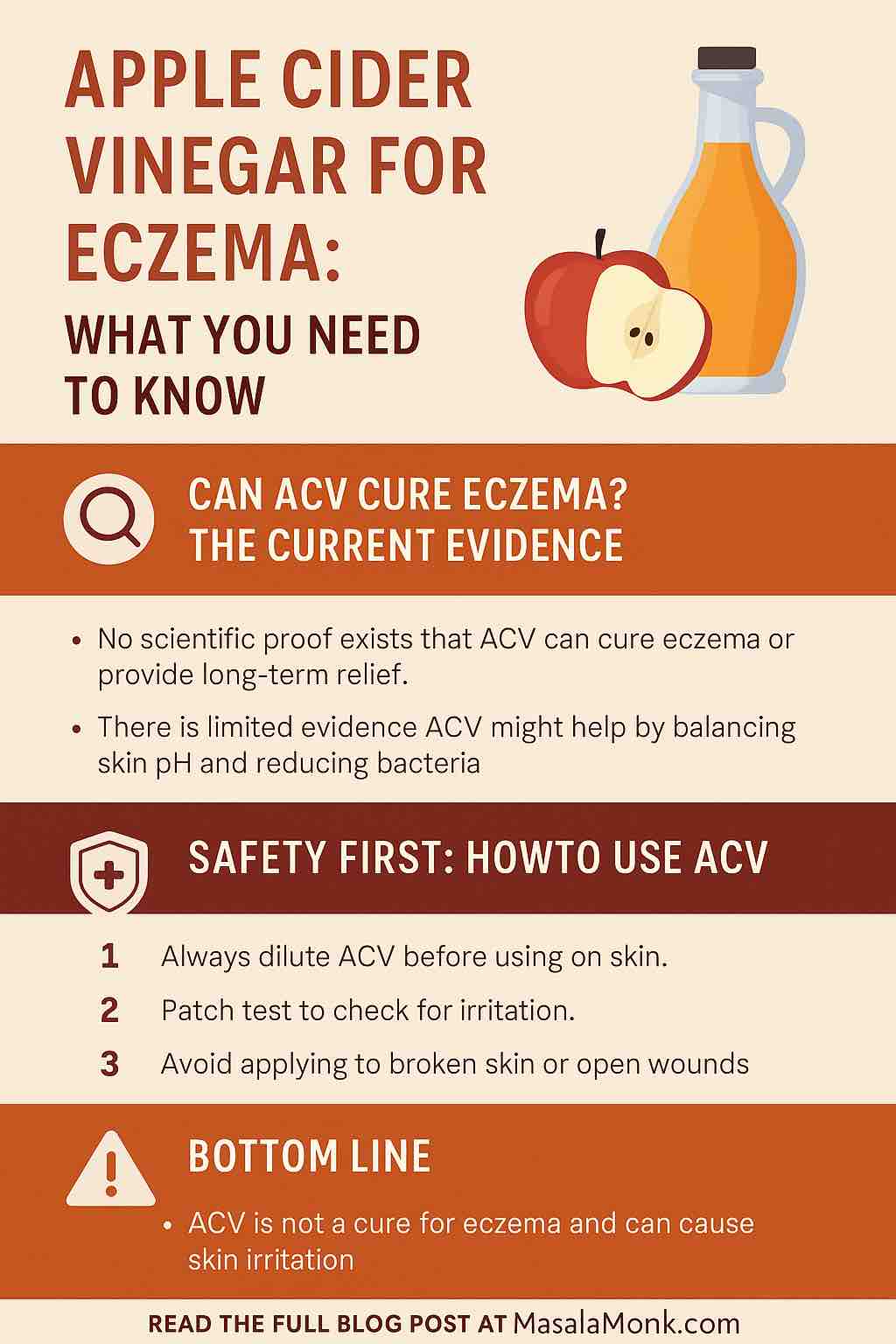
For those suffering from skin irritations like eczema, rosacea, or dermatitis, garlic can offer natural relief. It inhibits the release of inflammatory enzymes and soothes reactive skin.
Note: Always use diluted preparations. Combine garlic with calming ingredients like oatmeal or chamomile-infused water.
✅ 4. Heals Wounds, Cuts, and Fungal Infections
Garlic’s antibacterial and antifungal properties accelerate the healing of small wounds, cuts, or fungal skin infections like ringworm and athlete’s foot.
Spot Treatment: Dab diluted garlic juice (1:3 with water) on minor infections. Let it dry and then rinse. Apply 1–2 times daily.
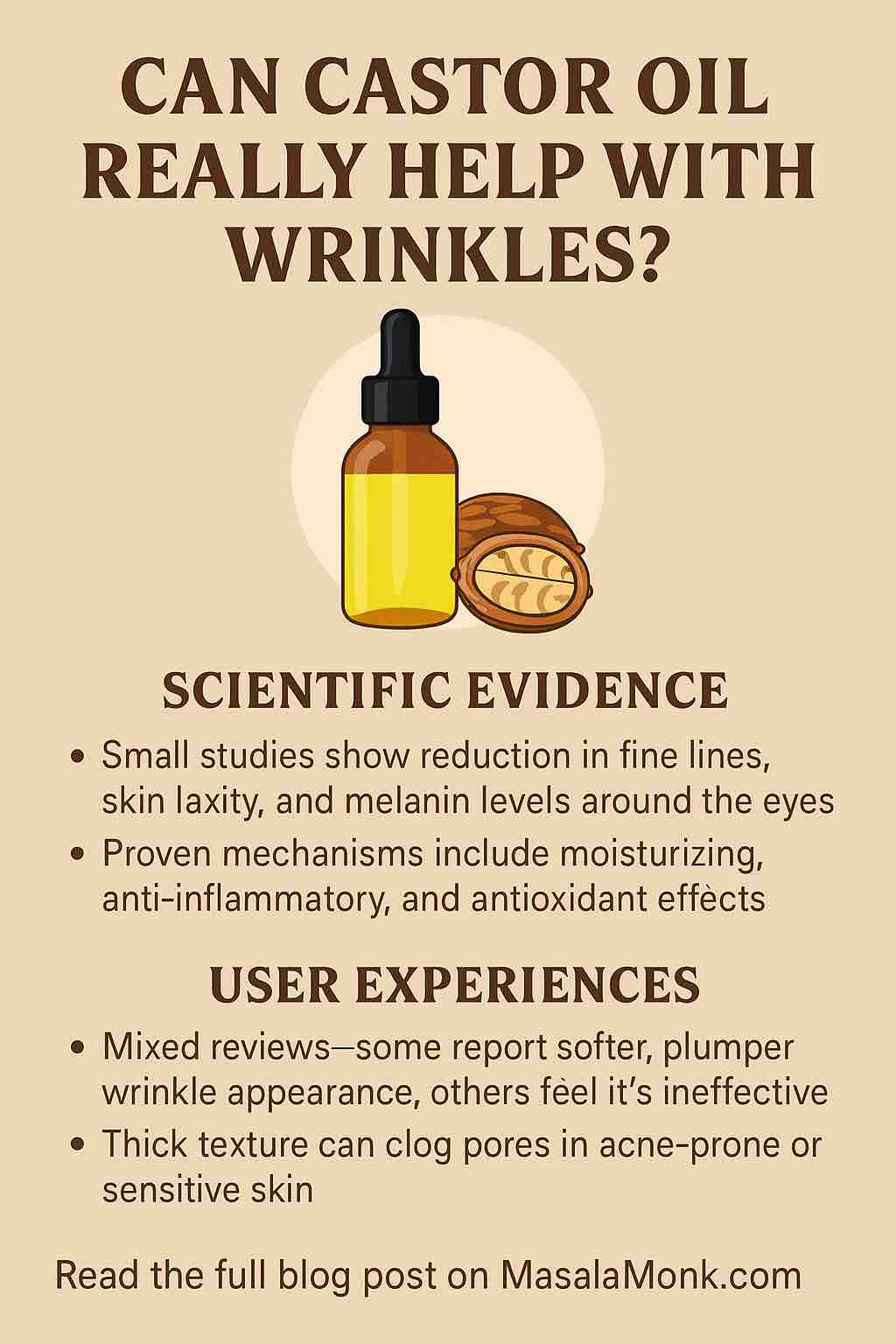
✅ 5. Delays Signs of Aging
Garlic is rich in antioxidants that protect skin cells from free radical damage—one of the major causes of premature aging. Regular topical use can improve skin elasticity, soften fine lines, and improve overall skin tone.
Anti-Aging Serum: Infuse garlic in jojoba or almond oil for 5–7 days. Apply a few drops at night to boost cell repair and hydration.
🦤 How to Use Garlic on Skin Safely
Garlic is powerful—and that means it must be used with care to avoid irritation or burns. Here are safe, effective ways to incorporate it into your skincare routine:
🧼 1. Garlic Face Mask
- Crushed garlic (1 clove)
- Rose water (1 tbsp)
- Chickpea flour (1 tsp)
- Mix well and apply for 10 minutes. Rinse with cool water.
💄 2. Garlic-Infused Oil
- Soak peeled garlic cloves in coconut or olive oil for a week.
- Strain and store in a dark glass bottle.
- Use as a massage oil or night-time spot treatment.
🤾 3. Garlic Spot Corrector
- Mix 1 part garlic juice with 3 parts aloe vera gel or water.
- Apply only to spots, not the entire face.
- Avoid contact with eyes, nostrils, or broken skin.
⚠️ Important Safety Tips
- Always do a patch test before applying garlic preparations to the face.
- Use only 1–2 times a week to prevent irritation.
- Never apply raw garlic directly for prolonged periods.
- Dilute garlic with water, aloe, or oils.
- Discontinue use if irritation or burning occurs.
🔮 What the Research Says
While more human clinical trials are needed, laboratory studies and traditional medicine have long recognized garlic’s anti-inflammatory, antimicrobial, and healing effects on skin. These findings support its role in:
- Reducing acne bacteria
- Healing wounds faster
- Treating fungal infections
- Fighting oxidative damage
🌿 Natural, Accessible, Effective: Garlic Deserves Your Attention
In the age of synthetic serums and expensive treatments, garlic offers a natural, affordable, and highly effective alternative. Its unique combination of compounds makes it a standout ingredient for those seeking:
- Acne-free skin
- Brighter complexion
- Reduced signs of aging
- Healthier, more resilient skin barrier
Whether used in homemade masks, spot treatments, or infused oils, garlic’s potential is hard to ignore. This isn’t just folklore—it’s nature’s skincare powerhouse, right in your kitchen.
👉 Want to Know the Best Ways to Use Garlic for Your Skin Type?
Explore full recipes, tips, and expert insights in the complete post on MasalaMonk.com. Your radiant skin journey starts here.
FAQs
1. Can garlic cause skin irritation?
Yes, garlic is potent and can cause irritation or burns if applied raw or for too long. Always dilute garlic with aloe vera, oils, or water, and do a patch test before full use. Limit applications to 1–2 times a week.
2. How often should I use garlic treatments on my skin?
It’s best to use garlic-based skincare products 1 to 3 times per week. Overuse may lead to redness, dryness, or irritation.
3. Can garlic help with acne scars?
Garlic has anti-inflammatory and healing properties that may help reduce acne scars over time by promoting skin repair and reducing pigmentation, but results vary by individual.
4. Is garlic safe for all skin types?
While garlic benefits many skin types, sensitive or allergy-prone skin should use it cautiously and always patch test. Diluting garlic and combining it with soothing ingredients is recommended.
5. How do I make garlic-infused oil for skincare?
Peel garlic cloves and soak them in coconut or olive oil for 5–7 days in a dark, cool place. Strain and store in a dark bottle. Use as a spot treatment or massage oil.
6. Can I use garlic directly on my face?
Direct raw garlic can be too harsh and cause burns or irritation. Always crush and dilute it with aloe vera, oils, or other gentle ingredients before applying.
7. Does garlic help with skin brightening?
Yes, garlic improves blood circulation and detoxifies the skin, which can lead to a brighter, more even complexion with regular use.
8. Can garlic treat fungal skin infections?
Garlic’s antifungal properties make it effective for minor fungal infections like athlete’s foot or ringworm when applied diluted and consistently.
9. Are there any risks of using garlic oil on the skin?
Garlic oil is generally safe if made and stored properly, but using homemade infused oil can carry a risk of contamination if not stored well. Use within a reasonable time and avoid if irritation occurs.
10. How does garlic delay signs of aging?
Garlic contains antioxidants that neutralize free radicals, protecting skin cells from damage, which helps reduce wrinkles, fine lines, and sagging when used regularly.