Understanding the Role of Ozempic
Ozempic, or semaglutide, is not just another medication on the shelf. It’s a groundbreaking treatment primarily designed for type 2 diabetes management. But its benefits don’t stop there. Many individuals have reported a noticeable weight loss while on Ozempic, making it a multifaceted medication that addresses both diabetes and obesity.
The Symbiotic Relationship Between Ozempic and Diet
Every medication interacts with our body, and our diet can influence this interaction. With Ozempic, the foods you consume can:
- Amplify the drug’s effectiveness.
- Help in reducing or managing potential side effects.
- Contribute to overall health, complementing the drug’s benefits.
The Aim of This Guide
Navigating the world of dietary choices while on medication can be daunting. This guide is crafted to simplify that journey. By marrying the specifics of Ozempic with a tailored meal plan, we aim to provide a roadmap for those seeking to optimize their health while on this medication.
Day 1 – Embarking on Your Ozempic Dietary Journey
🍳 Breakfast: Setting the Tone for the Day
- Green Power Smoothie Bowl: A creamy blend of spinach, avocado, and blueberries, enriched with chia seeds and almond milk. Garnish with a handful of granola and freshly sliced bananas for that extra crunch and natural sweetness.
- Dietary Insight: This breakfast option is fiber-rich, ensuring a gradual release of sugars, which is harmonious with Ozempic’s function.
🥗 Lunch: Balancing Nutrition and Flavor
- Mediterranean Grilled Chicken Salad: Tender slices of grilled chicken breast paired with mixed greens, cherry tomatoes, cucumber, olives, and a sprinkle of feta cheese. Drizzle with a dressing made from olive oil, lemon zest, and a hint of oregano.
- Dietary Insight: The protein from the chicken aids muscle health, while the greens and veggies offer a spectrum of vitamins and minerals.
🍞 Snack: Sustained Energy Release
- Creamy Almond Butter on Whole Grain Toast: A generous spread of almond butter on a toasted slice of whole grain bread, perhaps with a drizzle of honey for those with a sweet tooth.
- Dietary Insight: The combination of healthy fats from the almond butter and complex carbs from the bread ensures energy without abrupt blood sugar spikes.
🍲 Dinner: A Wholesome End to the Day
- Asian-inspired Quinoa and Vegetable Stir-Fry: A colorful mix of bell peppers, broccoli, and snap peas sautéed with fluffy quinoa in a light olive oil base. Season with fresh garlic, ginger, and a splash of low-sodium soy sauce for that authentic Asian flavor.
- Dietary Insight: Quinoa, being a complete protein and rich in fiber, is an excellent grain choice, especially for those on Ozempic.
🍵 Nightcap: Tranquility in a Cup
- Golden Chamomile Tea: Steep a chamomile tea bag with a pinch of turmeric for a warm, calming beverage to conclude the day.
- Dietary Insight: Chamomile is renowned for its soothing properties, promoting relaxation and aiding sleep.
The above chapters provide a foundational understanding of Ozempic’s role and how diet intertwines with its functionality. The detailed Day 1 meal plan offers a balanced approach to eating while on the medication. The subsequent chapters will further explore meal plans for the upcoming days, interspersed with insights and tips to enhance the Ozempic experience through mindful eating.
📥 Get Your PDF Guide – Ozempic Diet Plan PDF – here’s the link to download this guide as a PDF.
Day 2 – Diversifying Your Diet
🍳 Breakfast: A Fresh Start
- Tropical Fruit Parfait: Layer Greek yogurt with slices of mango, pineapple, and kiwi. Top with a sprinkle of coconut flakes and a handful of walnuts.
- Dietary Insight: The probiotics in Greek yogurt promote gut health, while the tropical fruits offer a burst of vitamins and antioxidants.
🥗 Lunch: A Trip to the Mediterranean
- Falafel Wrap with Tzatziki: Homemade falafels wrapped in a whole grain tortilla with lettuce, tomatoes, and a generous dollop of tzatziki sauce.
- Dietary Insight: Chickpeas, the primary ingredient in falafels, are rich in protein and fiber, ensuring a steady energy release.
🍞 Snack: Crunch and Munch
- Veggie Sticks with Hummus: Sliced cucumber, bell peppers, and carrots paired with a tangy roasted red pepper hummus.
- Dietary Insight: This snack is low in calories but high in nutrients, making it perfect for those mid-day hunger pangs.
🍲 Dinner: Comfort in a Bowl
- Lentil and Vegetable Soup: A hearty mix of lentils, carrots, celery, and onions simmered in a tomato-based broth with a hint of rosemary and thyme.
- Dietary Insight: Lentils are a powerhouse of protein and fiber, making this soup both filling and nutritious.
🍵 Nightcap: Soothing Warmth
- Lavender Infused Green Tea: A calming blend of green tea leaves with a hint of lavender.
- Dietary Insight: Green tea is rich in antioxidants, while lavender is known for its relaxation properties.
📥 Get Your PDF Guide – Ozempic Diet Plan PDF – here’s the link to download this guide as a PDF.
Day 3 – Exploring New Flavors
🍳 Breakfast: A Berry Good Morning
- Mixed Berry Oatmeal: Slow-cooked oats with a medley of strawberries, blueberries, and raspberries. Drizzle with a touch of maple syrup or honey.
- Dietary Insight: Oats are a fantastic source of soluble fiber, which can help stabilize blood sugar levels.
🥗 Lunch: An Italian Affair
- Spinach and Ricotta Stuffed Pasta Shells: Jumbo pasta shells filled with a creamy blend of spinach and ricotta cheese, baked in a rich marinara sauce.
- Dietary Insight: Spinach is packed with iron and calcium, while ricotta offers a dose of protein.
🍞 Snack: Sweet Indulgence
- Dark Chocolate and Almond Clusters: Melted dark chocolate mixed with whole almonds, then cooled to form bite-sized clusters.
- Dietary Insight: Dark chocolate is rich in antioxidants, and almonds provide healthy fats and protein.
🍲 Dinner: A Taste of the Sea
- Grilled Salmon with Asparagus and Quinoa: A fillet of salmon grilled to perfection, served with steamed asparagus and fluffy quinoa.
- Dietary Insight: Salmon is a great source of omega-3 fatty acids, which can help reduce inflammation.
🍵 Nightcap: A Classic Choice
- Chamomile and Mint Tea: A blend of chamomile flowers and fresh mint leaves steeped to create a refreshing beverage.
- Dietary Insight: Mint aids digestion, making this a perfect drink to wind down the day.
📥 Get Your PDF Guide – Ozempic Diet Plan PDF – here’s the link to download this guide as a PDF.
Day 4 – Embracing Plant Power
🍳 Breakfast:
Avocado Toast with Poached Eggs: Whole grain toast topped with mashed avocado and a perfectly poached egg. Sprinkle with some chia seeds for an added crunch.
- Dietary Insight: Avocado is rich in healthy fats that can help stabilize blood sugar levels, while eggs provide a protein boost.
🥗 Lunch:
Quinoa and Roasted Veggie Salad: A medley of roasted bell peppers, zucchini, and cherry tomatoes mixed with cooked quinoa. Drizzle with a lemon vinaigrette.
- Dietary Insight: Quinoa is a complete protein and a great source of fiber, making it an excellent choice for sustained energy.
🍞 Snack:
Edamame Beans: Steamed and lightly salted, these are a protein-packed snack.
- Dietary Insight: Edamame beans are rich in protein and can help keep you full between meals.
🍲 Dinner:
Stuffed Bell Peppers: Bell peppers filled with a mixture of brown rice, black beans, corn, and diced tomatoes. Baked to perfection.
- Dietary Insight: This meal is a balanced combination of complex carbs, protein, and veggies.
📥 Get Your PDF Guide – Ozempic Diet Plan PDF – here’s the link to download this guide as a PDF.
Day 5 – Going Global
🍳 Breakfast:
Chia Seed Pudding with Tropical Fruits: Overnight chia seed pudding topped with slices of kiwi, mango, and a sprinkle of shredded coconut.
- Dietary Insight: Chia seeds are rich in omega-3 fatty acids and fiber, promoting heart and gut health.
🥗 Lunch:
Thai Basil Stir Fry: A mix of chicken, bell peppers, green beans, and onions stir-fried in a tangy Thai basil sauce. Serve with jasmine rice.
- Dietary Insight: This dish offers a balance of protein, veggies, and carbs, ensuring a steady release of energy.
🍞 Snack:
Dried Seaweed Sheets: A crunchy, salty snack that’s low in calories.
- Dietary Insight: Seaweed is rich in iodine, which supports thyroid function.
🍲 Dinner:
Moroccan Chickpea Stew: A hearty stew made with chickpeas, tomatoes, carrots, and a blend of Moroccan spices.
- Dietary Insight: Chickpeas are a great source of protein and fiber, making this dish both nutritious and filling.
📥 Get Your PDF Guide – Ozempic Diet Plan PDF – here’s the link to download this guide as a PDF.
Day 6 – Comfort Foods Made Healthy
🍳 Breakfast:
Banana Pancakes: Fluffy pancakes made with mashed bananas and whole wheat flour. Top with a drizzle of honey and fresh berries.
- Dietary Insight: Using bananas adds natural sweetness, reducing the need for added sugars.
🥗 Lunch:
Zucchini Noodles with Pesto: Spiralized zucchini noodles tossed in a fresh basil pesto sauce. Top with grilled chicken or tofu for added protein.
- Dietary Insight: Zucchini noodles are a low-carb alternative to traditional pasta, making them a great choice for those watching their blood sugar levels.
🍞 Snack:
Cottage Cheese with Pineapple Chunks: A creamy, tangy snack that’s rich in protein.
- Dietary Insight: Cottage cheese is a slow-digesting protein source, making it an excellent snack to keep you full.
🍲 Dinner:
Lentil Shepherd’s Pie: A twist on the classic, using lentils as the base and topped with a creamy mashed cauliflower crust.
- Dietary Insight: Lentils provide a protein and fiber boost, while cauliflower is a low-carb alternative to traditional mashed potatoes.
📥 Get Your PDF Guide – Ozempic Diet Plan PDF – here’s the link to download this guide as a PDF.
Day 7 – A Fresh Start
🍳 Breakfast:
Berry Smoothie Bowl: A thick blend of mixed berries, Greek yogurt, and a splash of almond milk. Top with granola, sliced almonds, and a drizzle of honey.
- Dietary Insight: Berries are packed with antioxidants, and Greek yogurt provides a protein punch to kickstart your day.
🥗 Lunch:
Mediterranean Chickpea Salad: A refreshing mix of chickpeas, cucumbers, cherry tomatoes, olives, and feta cheese. Toss with olive oil, lemon juice, and fresh herbs.
- Dietary Insight: This salad is a fiber powerhouse, ensuring steady blood sugar levels and prolonged satiety.
🍞 Snack:
Hummus and Veggie Sticks: Creamy hummus served with sliced cucumbers, bell peppers, and carrot sticks.
- Dietary Insight: Hummus, made from chickpeas, is a protein-rich snack that pairs perfectly with crunchy veggies.
🍲 Dinner:
Grilled Salmon with Asparagus: A fillet of salmon grilled to perfection, served with a side of roasted asparagus and a lemon-herb sauce.
- Dietary Insight: Salmon is rich in omega-3 fatty acids, which are beneficial for heart health and reducing inflammation.
📥 Get Your PDF Guide – Ozempic Diet Plan PDF – here’s the link to download this guide as a PDF.
Understanding the Importance of Diet with Ozempic
The Ozempic-Diet Connection:
Ozempic, while a revolutionary drug for managing type 2 diabetes and promoting weight loss, works best when paired with a balanced diet. The food choices you make can either amplify or diminish the drug’s effectiveness.
Balancing Carbs and Protein:
For those on Ozempic, it’s crucial to balance carbohydrate intake with protein. This ensures steady blood sugar levels and helps manage potential side effects like diarrhea or stomach issues.
Hydration is Key:
Staying hydrated can alleviate some of the gastrointestinal side effects associated with Ozempic. Aim for at least 8 glasses of water a day, and consider adding hydrating foods like cucumbers and watermelon to your diet.
Listening to Your Body:
Every individual’s reaction to Ozempic can vary. It’s essential to listen to your body and adjust your diet accordingly. If certain foods exacerbate side effects, consider eliminating or reducing them.
Seeking Professional Guidance:
If you’re unsure about the best diet to pair with Ozempic, consider consulting with a nutritionist or dietitian. They can provide personalized advice tailored to your needs and health goals.
Tips for Managing Side Effects Through Diet
1. Combatting Nausea:
🍏 Opt for Bland Foods: Foods like toast, rice, and applesauce can be easier on the stomach when feeling nauseous.
🍵 Ginger Tea: Ginger has natural properties that can help soothe an upset stomach.
2. Addressing Diarrhea:
🍌 Bananas: Rich in pectin, they can help absorb excess water in the intestines.
🍚 White Rice: It acts as a binding food and can provide relief.
3. Alleviating Constipation:
🥦 Increase Fiber Intake: Foods like broccoli, beans, and whole grains can promote regular bowel movements.
💧 Stay Hydrated: Drinking plenty of water can help soften stools.
4. Reducing Heartburn and Acid Reflux:
🍅 Limit Acidic Foods: Tomatoes, citrus fruits, and spicy foods can exacerbate heartburn.
🥛 Almond Milk: A soothing alternative to regular milk, which can sometimes trigger acid reflux.
Conclusion – The Synergy of Ozempic and Diet
The Power of Combination:
Ozempic, when combined with a balanced diet, can be a potent tool in managing type 2 diabetes and facilitating weight loss. It’s not just about the medication but also about the lifestyle choices that accompany it.
Individualized Approach:
Remember, everyone’s body is unique. What works for one person might not work for another. It’s essential to listen to your body, monitor how it reacts, and adjust your diet accordingly.
Seeking Continuous Guidance:
As you continue your journey with Ozempic, regular check-ins with your healthcare provider are crucial. They can provide insights, adjust dosages, and offer guidance on dietary changes.
Frequently Asked Questions (FAQs) about Ozempic and Diet
Q: Can I drink alcohol while on Ozempic?
While occasional moderate drinking might be acceptable, it’s essential to consult with your healthcare provider. Alcohol can affect blood sugar levels and might interfere with the medication’s effectiveness.
Q: Are there any specific foods I should avoid entirely?
There’s no strict “no” list, but it’s recommended to limit foods that can spike blood sugar levels, such as sugary snacks and beverages. Also, if you notice any food-exacerbating side effects, it’s best to avoid them.
Q: Can I follow a keto or low-carb diet with Ozempic?
Many patients on Ozempic find success with low-carb diets. However, it’s crucial to ensure you’re getting all necessary nutrients. Always consult with a nutritionist or doctor before starting any strict diet.
Q: How does caffeine affect Ozempic?
There’s no direct interaction between caffeine and Ozempic. However, excessive caffeine can impact blood sugar levels, so it’s best to consume in moderation.
Q: I’ve heard about the “Ozempic weight loss plateau.” What is it?
Some users report a period where weight loss slows down or stops after initial success. This plateau can be due to various reasons, including dietary choices. It’s essential to maintain a balanced diet and consult with your healthcare provider if you experience this.
Resources and Further Reading
📚 Comprehensive Guide to Ozempic
For those who want a deep dive into the world of Ozempic, beyond just the dietary aspects, we recommend our comprehensive guide. It covers everything from the science behind the medication to personal stories and expert opinions.
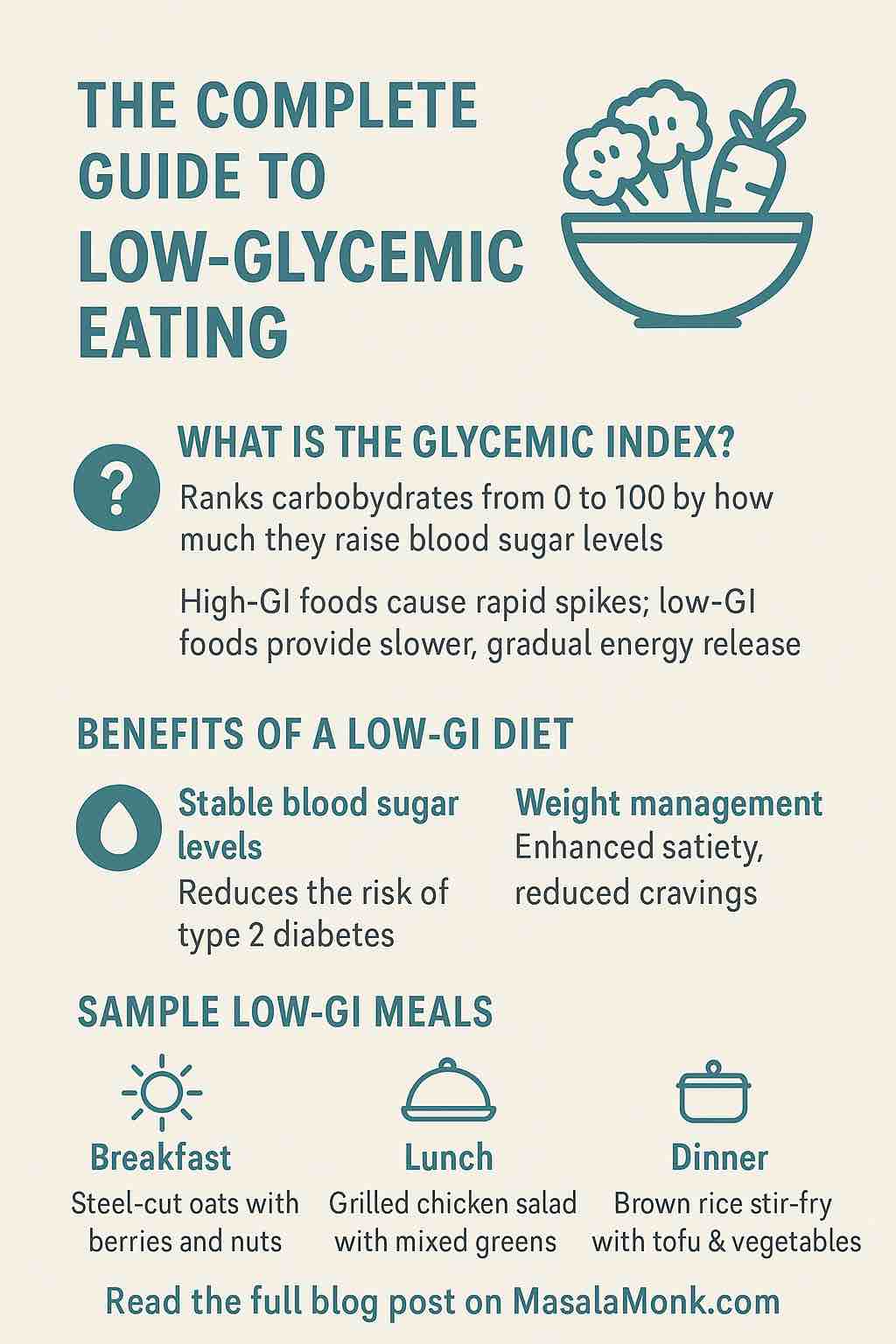
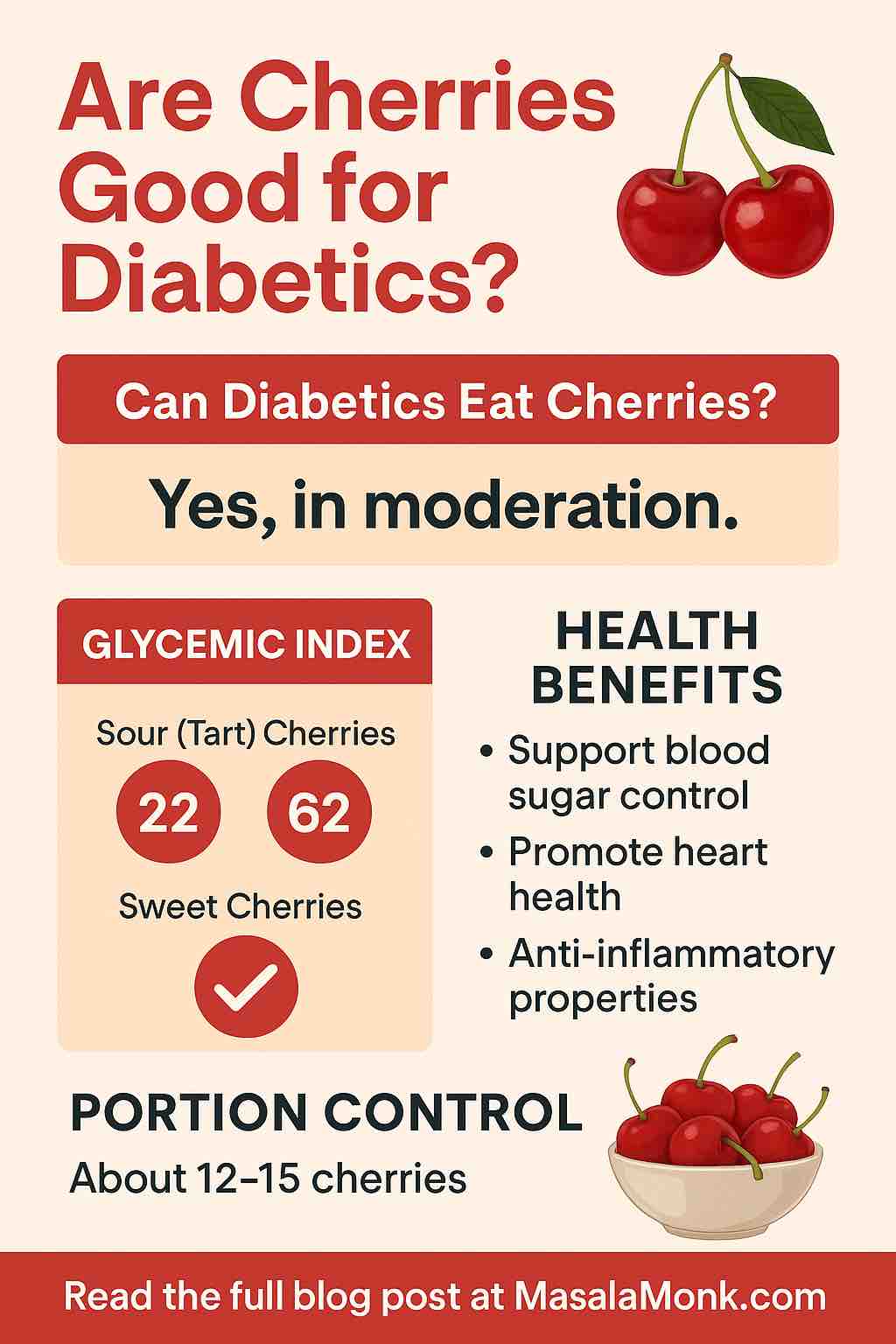
🍏 Diet and Diabetes
Understanding the intricate relationship between what you eat and how it affects your blood sugar is crucial. This recommended reading provides insights into the glycemic index, carb counting, and more.
🔗 Useful Links
📖 Personal Stories and Blogs
Hearing from others can be both enlightening and comforting. Check out these blogs and personal accounts from individuals navigating their journey with diabetes and Ozempic.
Download and Share
📥 Get Your PDF Guide – Ozempic Diet Plan PDF
As promised, here’s the link to download this guide as a PDF. It’s designed for easy reading, with clickable links and a layout optimized for both mobile and desktop.
🌍 Share the Knowledge
If you found this guide helpful, please consider sharing it with friends, family, or anyone you think might benefit. Every share helps us reach more people and spread valuable information.
💌 Stay Updated
For the latest updates, articles, and resources related to Ozempic, diabetes, and diet, consider subscribing to our newsletter. We promise to keep our content relevant and spam-free.
Conclusion and Key Takeaways
🌟 A Holistic Approach to Health with Ozempic
While Ozempic offers a promising solution for many with type 2 diabetes, it’s essential to remember that medication is just one piece of the puzzle. A balanced diet, regular exercise, and consistent monitoring are equally crucial. This guide has provided a roadmap for those on Ozempic to navigate their dietary choices, but it’s essential to tailor these suggestions to individual needs and preferences.
🍽️ Diet is Personal
What works for one person might not work for another. It’s essential to listen to your body, monitor your blood sugar levels, and adjust your diet accordingly. If certain foods cause spikes or drops in your blood sugar, it’s crucial to take note and modify your intake.
🤝 Seek Support
Managing diabetes and adjusting to medications like Ozempic can be challenging. But remember, you’re not alone. Reach out to support groups, healthcare professionals, and loved ones for guidance and encouragement.
📈 Stay Informed
The world of medicine and nutrition is ever-evolving. Stay updated with the latest research, findings, and recommendations related to Ozempic and diabetes management.
Your Journey Ahead
🚀 Embrace the Journey
Starting on Ozempic and adapting to a new diet plan can feel overwhelming. But view it as an opportunity—a chance to learn more about your body, make healthier choices, and improve your overall well-being.
📝 Track Your Progress
Consider maintaining a food and symptom diary. It can help you identify patterns, understand how different foods affect you, and make necessary adjustments.
🌱 Growth Mindset
Challenges and setbacks might occur, but they’re all part of the journey. Embrace a growth mindset, learn from every experience, and remember that every step, no matter how small, is progress.
💌 We’re Here for You
At MasalaMonk, we’re committed to providing valuable resources and support. Whether you have questions, feedback, or just need someone to talk to, our community is here for you.
With this, we wrap up our comprehensive guide on the Ozempic eating plan. Remember, the journey to health is a marathon, not a sprint. Take it one day at a time, stay informed, seek support, and believe in yourself. You’ve got this! 🌟
📋 Frequently Asked Questions (FAQs) – Ozempic and Diet
💊 About the Medication
Q1: What is Ozempic, and how does it work?
Ozempic (semaglutide) is a GLP-1 receptor agonist used primarily to manage type 2 diabetes. It works by increasing insulin secretion, decreasing glucagon secretion, slowing gastric emptying, and promoting a sense of fullness—often leading to weight loss.
Q2: Is Ozempic only for people with diabetes?
While it’s FDA-approved for type 2 diabetes, Ozempic is also prescribed off-label for weight management in individuals with or without diabetes. However, any use should be under medical supervision.
🥗 Diet and Nutrition
Q3: Do I need to follow a special diet while on Ozempic?
There’s no strict diet required, but following a balanced, nutrient-rich meal plan helps enhance the effectiveness of Ozempic and minimizes side effects like nausea, bloating, or diarrhea.
Q4: Can I eat carbohydrates while taking Ozempic?
Yes, but focus on complex carbs with a low glycemic index (like whole grains, lentils, and vegetables). Pairing carbs with protein and fiber helps maintain stable blood sugar levels.
Q5: Is a low-carb or keto diet safe with Ozempic?
Many find success with a low-carb or moderate-carb diet. However, extreme keto diets should only be followed under professional guidance to ensure nutritional adequacy and safety.
Q6: How important is hydration?
Very. Staying hydrated can help reduce common side effects like nausea and constipation. Aim for at least 8 cups of water daily, and include water-rich foods like cucumbers, berries, and watermelon.
😌 Managing Side Effects with Diet
Q7: What should I eat to reduce nausea?
Stick to bland, low-fat foods such as toast, bananas, or applesauce. Ginger tea or ginger chews may help ease nausea naturally.
Q8: How can I manage constipation?
Increase fiber intake (leafy greens, lentils, chia seeds), hydrate well, and consider adding fermented foods like yogurt or kefir to support digestion.
Q9: What foods worsen Ozempic side effects?
Greasy, fried, or highly processed foods may worsen nausea or cause bloating. Spicy or acidic foods can increase the risk of heartburn.
🍷 Lifestyle Considerations
Q10: Can I drink alcohol while taking Ozempic?
Alcohol should be consumed in moderation and only if approved by your healthcare provider. It can affect blood sugar and may exacerbate gastrointestinal side effects.
Q11: Does caffeine interfere with Ozempic?
There’s no known direct interaction, but excess caffeine can cause dehydration or stomach irritation, so moderation is key.
Q12: Will I stop losing weight after a while?
Yes, a weight loss plateau is common. If this happens, review your diet, increase physical activity, and consult your provider for possible dosage adjustments or behavioral strategies.
🧭 General Guidance
Q13: Do I need to exercise while on Ozempic?
Exercise isn’t mandatory but strongly recommended. Physical activity helps manage blood sugar, improves cardiovascular health, and supports weight loss goals.
Q14: Should I count calories while using Ozempic?
Calorie tracking can be helpful but isn’t required. Prioritize nutrient density and portion control. Listen to your body’s natural hunger cues—Ozempic often helps regulate appetite.
Q15: Is this guide a substitute for medical advice?
No. This guide is informational and should complement, not replace, personalized medical or nutritional advice. Always consult your healthcare provider for tailored recommendations.