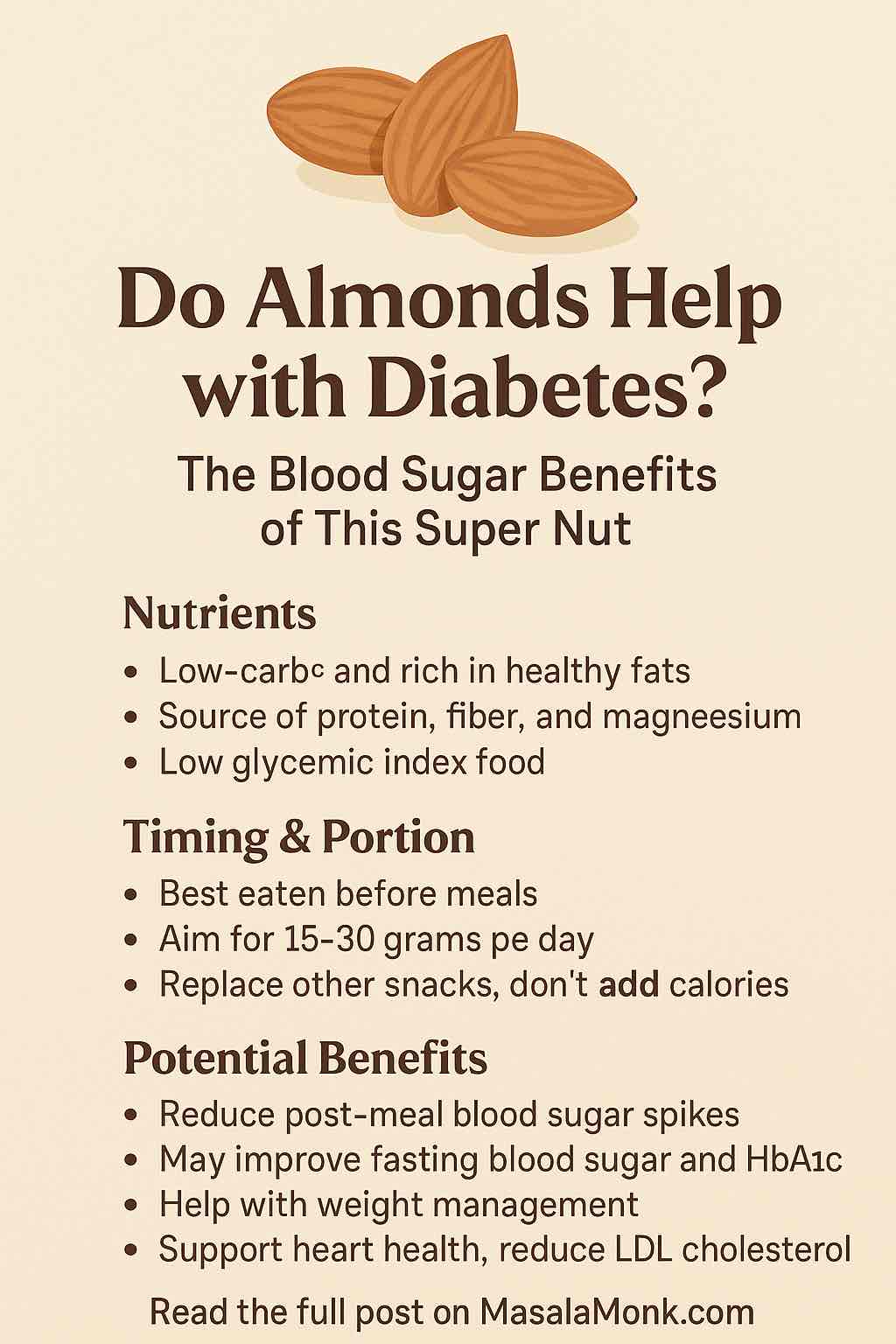
Managing blood sugar can feel like walking a tightrope—but what if a simple, delicious snack could make the balance easier?
Enter almonds: the crunchy little nuts that are making a big impact in diabetes management. From controlling post-meal sugar spikes to improving heart health, almonds might just be the super snack every diabetic and prediabetic person should consider.
But is it hype or hard science?
In this deep dive, we’ll unpack the latest clinical research, how almonds affect blood sugar, and the right way to incorporate them into your diet.
🧬 What Makes Almonds Special?
Almonds are not just low-carb—they’re nutrient powerhouses. A 28-gram serving (about 23 almonds) offers:
- 6g protein
- 3.5g fiber
- 14g fat (mostly monounsaturated)
- 75mg magnesium (helps insulin sensitivity)
- 0g sugar
They also have a low glycemic index, meaning they won’t cause major blood sugar spikes like refined carbs do.
🔬 The Science: What Studies Really Say
Let’s look at the evidence—both encouraging and nuanced.
✅ Short-Term Wins: Lower Post-Meal Spikes
Several studies confirm that almonds blunt the rise in blood sugar after eating a carbohydrate-rich meal:
- A 2022 study showed that eating just 15g of almonds before a meal reduced post-meal glucose by 14%.
- Another study from India (2024) found that a daily almond intake in prediabetics significantly improved fasting blood sugar and HbA1c.
These effects are likely due to the fat, fiber, and protein content in almonds, which slow digestion and buffer carb absorption.
⚠️ Long-Term Results: Not Always Straightforward
A 5-month trial in prediabetics (2023) revealed worsened insulin sensitivity and higher fasting glucose when participants added almonds without adjusting other foods—meaning they consumed more calories overall.
💡 Lesson: Almonds work best when they replace less healthy options—not when simply added on top.
🧠 How Almonds Work Their Magic
Here’s what makes almonds effective:
| Mechanism | Benefit for Diabetics |
|---|---|
| Slow gastric emptying | Reduces speed of glucose absorption |
| Increased satiety hormones | Triggers GLP‑1 and peptide YY (appetite control) |
| Magnesium & healthy fats | Improve insulin function |
| Low glycemic load | Minimal direct impact on blood sugar |
🕒 Timing is Everything: When to Eat Almonds
Studies show the timing of almond consumption significantly affects blood sugar:
- ✅ Before Meals: Eating almonds 30 minutes before a high-carb meal reduces glucose spikes.
- ✅ With Breakfast: May help reduce morning hyperglycemia.
- ⚠️ Mindless Snacking: Can lead to weight gain if not accounted for in total calorie intake.
Suggested Dosage:
Start with 15–20 grams (10–15 almonds) before lunch or dinner. This delivers benefits without adding too many extra calories.
🥗 Smart Ways to Add Almonds to Your Diet
Here are practical, diabetes-friendly ways to use almonds:
🍽️ As a Snack
- 15 raw almonds + 1 boiled egg
- Almonds + a small apple (for fiber and balance)
🥣 In Meals
- Crushed almonds on salads or sautéed vegetables
- Blend into oats with cinnamon (no sugar!)
🍵 In Smoothies
- Add almond butter (unsweetened!) to your morning smoothie for a protein-fat boost
🚫 Watch Out For…
Not all almond products are created equal. Avoid:
| Product | Why to Avoid |
|---|---|
| Sweetened almond milk | High added sugar can spike blood glucose |
| Almond snacks with salt/honey | Adds sodium and simple carbs |
| Overeating | Excess calories can increase insulin resistance |
❤️ Bonus Benefits: More Than Just Blood Sugar
Adding almonds to your diabetes plan also supports:
- ✅ Heart health: Lowers LDL cholesterol
- ✅ Weight management: Increases satiety
- ✅ Inflammation control: Rich in antioxidants and vitamin E
These are all critical factors for long-term diabetes management.
🧾 Real-Life Almond Plan for a Day
| Time | Almond Use |
|---|---|
| 7:30 AM | Almond butter in chia smoothie (1 tbsp) |
| 11:30 AM | 10 raw almonds 30 min before lunch |
| 4:00 PM | Handful of almonds + sliced cucumber |
| 7:00 PM | Crushed almonds over stir-fried veggies |
🧠 TL;DR — Should You Eat Almonds If You Have Diabetes?
Yes—with strategy.
Almonds can help reduce blood sugar spikes, especially when eaten before meals and in place of other snacks. But overconsumption or just “adding them in” can backfire.
Follow these principles:
- ✅ Keep it to 15–30g/day
- ✅ Replace—not stack—your snacks
- ✅ Eat before meals for best results
- ❌ Avoid sweetened or flavored almond products
📣 Final Thoughts
Almonds aren’t a magic bullet—but they are a smart, tasty, and scientifically supported ally in your fight against high blood sugar. Like all powerful tools, it’s about how you use them.
Ready to make almonds a regular part of your diabetes plan? Start with 10–15 almonds before your next carb-rich meal and feel the difference.
🔍 Frequently Asked Questions (FAQs)
1. Can almonds help control blood sugar levels?
Yes. Almonds can reduce post-meal glucose spikes when consumed before or with carbohydrate-rich meals. Their fiber, fat, and protein content slows glucose absorption.
2. How many almonds should a diabetic eat per day?
A typical recommendation is 15–30 grams per day (about 10–23 almonds), ideally spread across meals or snacks. Portion control is key to avoid excess calories.
3. Should I eat almonds before or after a meal?
For blood sugar benefits, eat almonds 30 minutes before a high-carb meal. This timing has been shown to reduce post-meal glucose spikes.
4. Are raw almonds better than roasted or salted ones?
Raw or dry-roasted unsalted almonds are best. Salted almonds may raise blood pressure, and flavored varieties may contain added sugars.
5. Can eating too many almonds raise blood sugar?
Not directly, but excessive almond consumption can lead to weight gain, which may worsen insulin resistance over time. Stick to recommended portions.
6. Is almond butter good for diabetics?
Yes, unsweetened almond butter retains the same benefits as whole almonds. Just ensure it contains no added sugars or hydrogenated oils.
7. What about almond milk—is it safe for diabetics?
Yes, but choose unsweetened almond milk only. Sweetened versions can contain enough sugar to spike blood glucose.
8. Can almonds replace carbs in my meal plan?
Almonds can be a low-carb replacement for snacks like chips or cookies. However, they should not replace essential carbs like whole grains or vegetables entirely.
9. Do almonds help with type 2 diabetes specifically?
Yes. Some studies show improved fasting blood sugar, HbA1c, and insulin sensitivity in people with type 2 diabetes who consumed almonds regularly as part of a calorie-balanced diet.
10. Can prediabetics benefit from eating almonds?
Yes, though results are mixed. When used to replace other foods, almonds may improve glucose and insulin levels. Simply adding them to the diet without calorie adjustment may not help.