Pregnancy is the perfect time to get creative with your drinks. Not the boozy kind — we’re talking fresh, colorful, nutrient-packed mocktails that deliver one of the most important nutrients your growing baby needs: folate.
Folate (or its synthetic form, folic acid) is vital for your baby’s neural tube development, especially in the first 12 weeks. The CDC recommends 400 mcg folic acid daily before conception and in early pregnancy to prevent serious birth defects like spina bifida and anencephaly. Beyond that, your body still needs folate throughout pregnancy — around 600 mcg DFE per day — to support cell growth, red blood cell production, and healthy development.
But here’s the twist: folate doesn’t have to come from tablets alone. You can sip it, savor it, and enjoy it in beautiful, alcohol-free mocktails made from folate-rich fruits, greens, and fortified juices.
🍹 Folate Needs at Each Stage of Pregnancy
| Stage | Folate Goal | Why It Matters | Drink Tip |
|---|---|---|---|
| Pre-conception & 1st trimester | 400 mcg folic acid (from prenatal or fortified sources) | Neural tube closure & early organ development | Choose fortified juices + whole fruit blends |
| 2nd trimester | 600 mcg DFE total | Supports rapid fetal growth & placenta health | Use leafy greens + citrus + berries |
| 3rd trimester | 600 mcg DFE total | Prepares for birth, supports increased blood volume | Mix hydrating bases with folate-rich fruits |
💡 Learn more about folate-rich foods in
Boosting Folate in Pregnancy: Top 5 Lentil and Bean Dishes
✅ Folate-Rich Ingredients to Stock Up On
- Pasteurized orange juice – naturally high in folate and often fortified
- Pomegranate juice – ~60 mcg folate per cup + antioxidants
- Spinach (fresh) – ~58 mcg per cup; blends well in smoothies
- Strawberries – ~40 mcg per cup; add sweetness without excess sugar
- Mango – ~18% DV per cup; creamy, tropical body
- Fortified cereals – 100–400 mcg per serving; can be blended into smoothies
- Legumes (chickpeas, lentils) – folate-rich base for savory sips
🥤 5 Non-Alcoholic Folate-Fortified Mocktails
Pregnancy hydration doesn’t have to be boring. These folate-packed drinks are refreshing, nutrient-dense, and Instagram-worthy — perfect for sipping while giving your body (and baby) the nutrients it needs. Each recipe is easy to prepare, safe for pregnancy (when using pasteurized juices), and bursting with flavor.
1. Sunrise Citrus Spritzer
Folate per serving: ~120 mcg
You’ll need:
- ½ cup pasteurized orange juice (freshly squeezed is fine if pasteurized)
- ½ cup pasteurized pomegranate juice
- Sparkling water to top
- Ice & fresh mint leaves for garnish

How to make it:
Fill a tall glass with ice. Pour in the orange juice and pomegranate juice for a vibrant two-tone effect. Top with sparkling water for a bubbly finish, and tuck a sprig of mint on top.
Pregnancy tip: Vitamin C in this drink helps your body absorb iron from other foods you eat.
2. Berry Green Glow Smoothie
Folate per serving: ~160 mcg
You’ll need:
- 1 cup spinach (washed well)
- 1 cup strawberries (washed & hulled)
- ½ banana
- ½ cup pasteurized orange juice
- ½ cup water
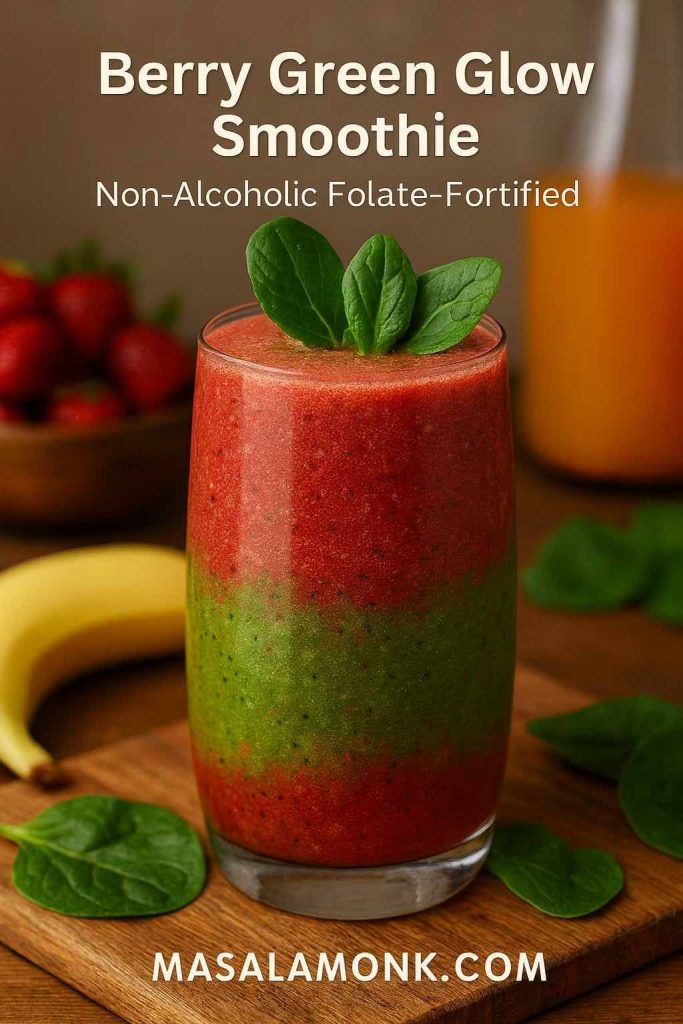
How to make it:
Add all ingredients to a blender and whiz until silky smooth. The spinach gives a gentle earthiness balanced by the natural sweetness of banana and strawberries.
Pregnancy tip: Spinach delivers folate and iron, while strawberries offer antioxidants for immune support.
3. Tropical Folate Fizz
Folate per serving: ~110 mcg
You’ll need:
- 1 cup ripe mango chunks
- ½ cup pasteurized pineapple juice
- ½ cup coconut water
- A squeeze of fresh lime

How to make it:
Blend the mango with pineapple juice until smooth, stir in coconut water, and add a splash of lime. Serve over ice for a beachy mocktail moment.
Pregnancy tip: Coconut water helps with hydration and replenishes electrolytes — perfect for hot days or post-morning sickness recovery.
4. Pomegranate Beet Refresher
Folate per serving: ~140 mcg
You’ll need:
- ½ cup pasteurized pomegranate juice
- ½ cup cooked beetroot (cooled & peeled)
- ½ cup sparkling water
- Squeeze of lemon
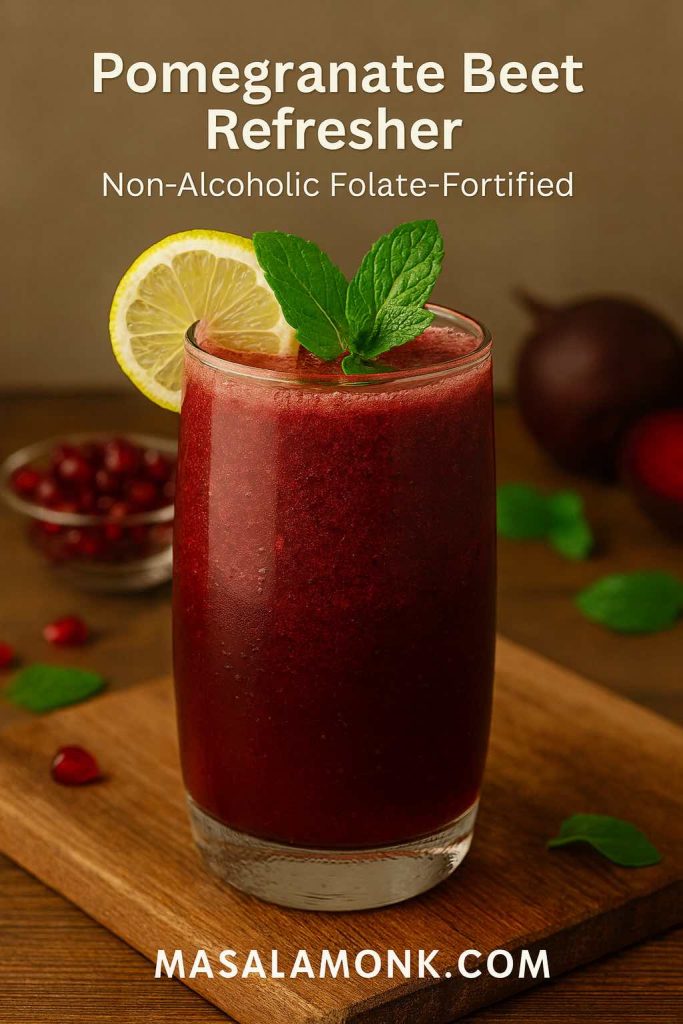
How to make it:
Blend beetroot with pomegranate juice until smooth. Strain for a clear liquid if desired. Pour over ice, top with sparkling water, and add a hint of lemon.
Pregnancy tip: Beets support healthy blood flow and hemoglobin production, which can help combat pregnancy fatigue.
5. Cereal Sunrise Shake
Folate per serving: ~250 mcg (varies by cereal choice)
You’ll need:
- ½ cup fortified breakfast cereal (choose one with added folic acid)
- 1 cup low-fat milk or fortified plant-based milk
- ½ banana
- Pinch of cinnamon

How to make it:
Combine cereal, milk, banana, and cinnamon in a blender until creamy. Enjoy as a quick breakfast or an afternoon energy boost.
Pregnancy tip: This is a great folate-rich option for mornings when you can’t face solid food.
⚠️ Pregnancy Drink Safety Tips
- Pasteurization is key — Avoid unpasteurized juices to reduce the risk of foodborne illness.
Learn more in Safe Eating During Pregnancy: Foods to Eat, Avoid, and Safety Practices - Watch sugar intake — Balance fruit juices with whole fruits, greens, and sparkling water.
- Mind herbal add-ins — Stick to culinary herbs (mint, basil) rather than medicinal doses.
💡 Why Mocktails Work for Folate
Mocktails make it easy to:
- Pair natural folate sources with fortified beverages
- Boost hydration without caffeine or alcohol
- Enjoy pregnancy-safe flavors that still feel festive
For more pregnancy drink inspiration, check out
Iron-Enriched Smoothies for Expecting Moms
🍋 Final Sip
Folate is one of the simplest, most effective nutrients to get right during pregnancy — and mocktails make it fun. With the right ingredients, you’re not just toasting to taste, but to your baby’s healthy development.
🍼 10 FAQs About Folate-Fortified Drinks in Pregnancy
1. Why is folate important during pregnancy?
Folate helps prevent neural tube defects, supports cell growth, and aids in forming red blood cells for both mother and baby.
2. How much folate do I need while pregnant?
The CDC recommends 400 mcg folic acid daily before and during early pregnancy, and 600 mcg DFE per day for the rest of pregnancy.
3. Can I get enough folate from food and drinks alone?
It’s possible if you eat a varied diet with folate-rich foods, but most women still need a prenatal supplement to meet daily needs.
4. Are folate-fortified drinks safe during pregnancy?
Yes, as long as they use pasteurized juices and safe ingredients. Always avoid unpasteurized products.
5. What fruits are highest in folate for mocktails?
Orange juice, pomegranate, strawberries, mango, and leafy greens like spinach are top folate sources.
6. Can I drink green smoothies during pregnancy?
Yes, if the greens are washed thoroughly and the ingredients are safe. Spinach-based smoothies are excellent folate sources.
7. Is there a difference between folate and folic acid in drinks?
Folate is the natural form in foods; folic acid is synthetic, found in fortified products and supplements.
8. Are there any risks of too much folic acid?
Excessive amounts may lead to unmetabolized folic acid (UMFA) in the body; follow your healthcare provider’s guidance, especially after the first trimester.
9. Can I use fortified plant milks in mocktails?
Yes. Many plant milks are fortified with folate and other key nutrients like calcium and vitamin D.
10. Are mocktails a good alternative to sugary sodas?
Definitely. Mocktails can be naturally sweet, nutrient-rich, and hydrating — without the excess sugar and empty calories.