Introduction
Craving a tuna melt or a refreshing tuna salad during your pregnancy, but feeling tangled in a sea of conflicting dietary advice? You’re not alone! For many expectant mothers, figuring out what’s safe to eat can feel like navigating uncharted waters, especially when it comes to seafood. Tuna, a staple in many diets due to its taste and nutritional benefits, often lands in a gray area for pregnant women. This guide is your compass to understanding the ins and outs of consuming tuna during pregnancy. From unpacking the health benefits of this popular fish to demystifying concerns about mercury content, we’re here to clear the waters. Plus, we’ll provide you with essential tips on choosing the right types of tuna and the safest ways to include it in your pregnancy diet. So, let’s set sail into the world of tuna, where we’ll balance the scales between nutrition and safety, ensuring you and your little one embark on a healthy pregnancy journey!
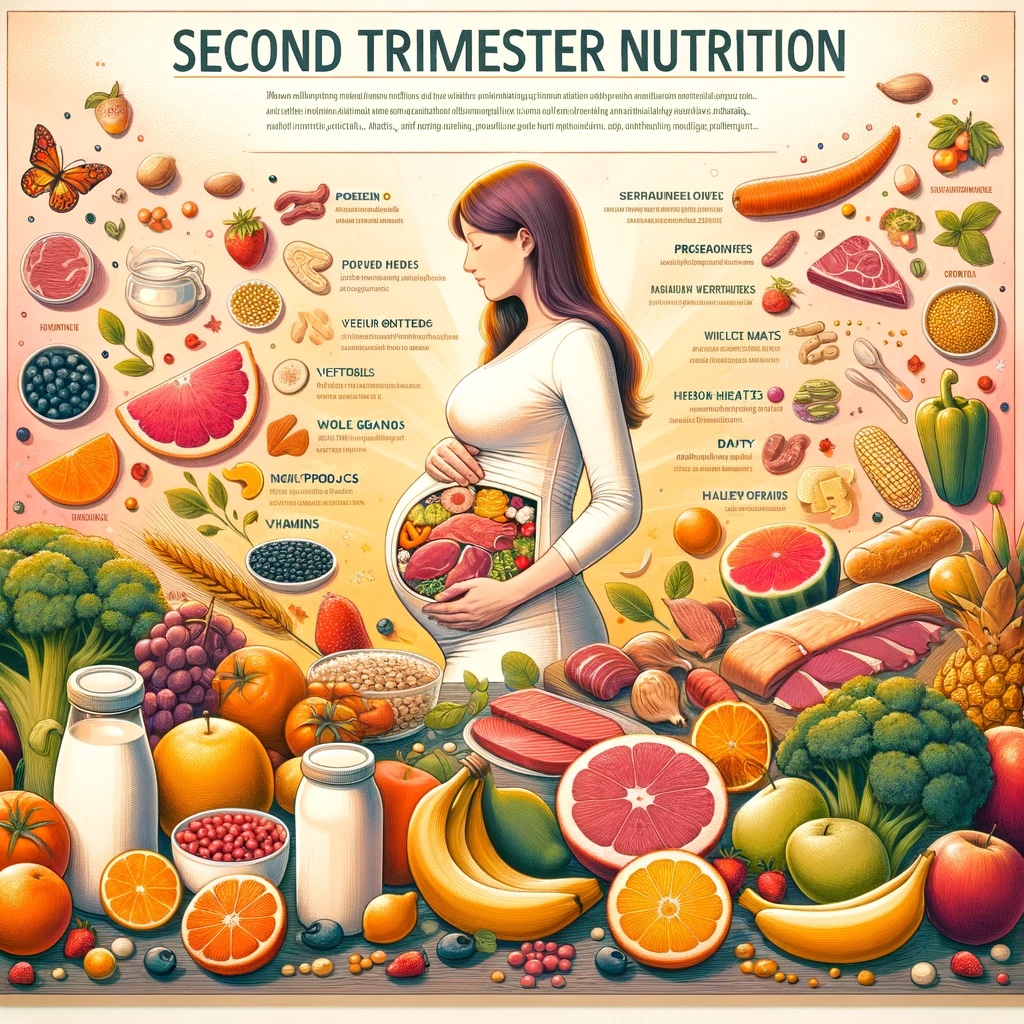
The Nutritional Benefits of Tuna for You and Your Baby
Before we dive into the deep end of safety concerns, let’s first explore why tuna is often a go-to fish for many, including expectant mothers. Tuna isn’t just delicious; it’s packed with nutrients essential for both you and your growing baby.
1. Rich in Omega-3 Fatty Acids:
- Brain Development: Omega-3s, particularly DHA, play a crucial role in your baby’s brain development. Including omega-3-rich foods like tuna in your diet can contribute positively to your child’s cognitive development.
- Heart Health: These fatty acids aren’t just good for the baby; they also support your cardiovascular health, a vital aspect during pregnancy.
2. High-Quality Protein Source:
- Building Blocks: Protein is a building block for the body. During pregnancy, you need more protein to support the growing fetus and your own bodily changes.
- Satiety and Energy: Tuna provides a satisfying and energy-boosting meal option, helping you manage pregnancy cravings and maintain energy levels.
3. Packed with Vitamins and Minerals:
- Vitamin D and Calcium: Essential for bone health, both for you and your baby. Tuna is one of the few food sources rich in Vitamin D.
- Iron and B Vitamins: These nutrients are crucial for energy production and preventing anemia, a common concern in pregnancy.
As tantalizing as these benefits are, it’s important to weigh them against the risks associated with mercury in tuna. In the next section, we’ll navigate these waters to help you make informed and safe dietary choices.
Understanding the Risks: Mercury in Tuna
While tuna is a nutrient-rich choice for expectant mothers, it’s crucial to discuss the elephant in the room – or rather, the mercury in the ocean. Understanding the risks associated with mercury in tuna is key to making informed dietary choices during your pregnancy.
The Concern with Mercury:
- Mercury Accumulation: Tuna, especially certain types, can contain higher levels of mercury due to their position in the food chain. Mercury accumulates in fish over time, and larger, longer-living species tend to have higher amounts.
- Effects on Development: The primary concern with mercury exposure during pregnancy is its potential impact on the developing brain and nervous system of the fetus. Even low levels of mercury can pose risks, making it essential to be cautious.
How to Mitigate the Risks:
- Choosing the Right Tuna: Not all tuna is created equal in terms of mercury content. Opting for varieties lower in mercury, such as canned light tuna, can reduce risk while still providing nutritional benefits.
- Limiting Consumption: Moderation is key. Adhering to recommended serving sizes and frequency can help minimize mercury exposure while still allowing you to enjoy tuna.
Being Informed Is Being Empowered:
- Staying Updated: Recommendations on fish consumption during pregnancy can change as new research emerges. Staying informed through reliable sources ensures you’re making the best choices based on current knowledge.
- Consulting Healthcare Providers: When in doubt, your healthcare provider is your best resource. They can offer guidance tailored to your health history and dietary needs.
In the next section, we’ll dive deeper into the types of tuna that are safest for pregnant women and how much you can safely eat to enjoy its benefits without worry.
Safe Types and Amounts of Tuna for Pregnant Women
Navigating the world of seafood during pregnancy can be complex, especially when it comes to tuna. Let’s simplify it by focusing on the safest types of tuna for you and your baby, and how much of it you can enjoy without worry.
1. Types of Tuna: Light vs. Albacore:
- Canned Light Tuna: Generally lower in mercury, this type of tuna is a safer choice. It includes varieties like skipjack.
- Albacore or White Tuna: Contains higher levels of mercury compared to light tuna. If you prefer albacore, it’s crucial to consume it in smaller amounts.
2. Recommended Consumption Limits:
- For Canned Light Tuna: Up to 12 ounces (about 340 grams) per week is considered safe. This amount equates to roughly 2-3 medium-sized cans.
- For Albacore Tuna: Limit your intake to less than 4 ounces (about 112 grams) per week. This is about one average-sized can.
3. Fresh Tuna Considerations:
- Fresh Tuna Steaks: While a nutritious option, fresh tuna steaks often have higher mercury levels. Limit your consumption and prefer smaller portions.
- Sushi and Raw Tuna: Pregnant women should avoid raw tuna, commonly found in sushi, due to the risk of bacterial contamination and higher mercury levels.
4. Balancing Safety and Nutrition:
- Variety is Key: Incorporate a variety of seafood into your diet to enjoy the benefits while minimizing risks. Alternating tuna with other low-mercury fish like salmon or sardines can provide diversity in nutrients and flavors.
- Preparation Matters: When preparing tuna, opt for healthier cooking methods like grilling or baking, and avoid high-calorie dressings or sauces.
Navigating tuna consumption during pregnancy doesn’t have to be a daunting task. By understanding the types and adhering to recommended limits, you can safely include this nutritious fish in your diet. Up next, we’ll explore some tuna alternatives that are rich in omega-3s, offering you more options for a balanced pregnancy diet.
Alternatives to Tuna for Omega-3 Intake During Pregnancy
For those who prefer to err on the side of caution or simply want to vary their diet, there are plenty of other ways to ensure you’re getting enough omega-3 fatty acids during your pregnancy. Let’s explore some tuna alternatives that are both safe and nutritious for you and your growing baby.
1. Other Low-Mercury Fish:
- Salmon: A fantastic alternative, salmon is not only lower in mercury but also rich in omega-3s.
- Sardines and Anchovies: These smaller fish are low in mercury and high in essential nutrients, making them a great option for pregnant women.
2. Plant-Based Omega-3 Sources:
- Flaxseeds and Chia Seeds: Add these to your yogurt, smoothies, or oatmeal for a plant-based omega-3 boost.
- Walnuts: A handful of walnuts can be a great snack, offering a good amount of omega-3s.
3. Omega-3 Enriched Foods and Supplements:
- Fortified Eggs: Some eggs are enriched with omega-3s, providing a convenient way to include these fatty acids in your diet.
- Supplements: If you find it challenging to include enough omega-3s in your diet, speak to your healthcare provider about supplements like fish oil capsules.
4. Incorporating Variety Into Your Diet:
- Recipe Ideas: Try recipes that incorporate these alternatives, like grilled salmon, walnut salads, or chia pudding.
- Balanced Nutrition: Remember, a varied diet not only helps in providing all necessary nutrients but also keeps mealtime interesting during pregnancy.
By exploring these alternatives to tuna, you can enjoy the benefits of omega-3 fatty acids without the concerns related to mercury. In the next section, we’ll answer some frequently asked questions to further clarify any doubts about consuming tuna and its alternatives during pregnancy.
Frequently Asked Questions (FAQs) About Eating Tuna During Pregnancy
Pregnancy comes with its share of questions, especially regarding diet. To help clear up any confusion, here are answers to some of the most commonly asked questions about eating tuna during pregnancy.
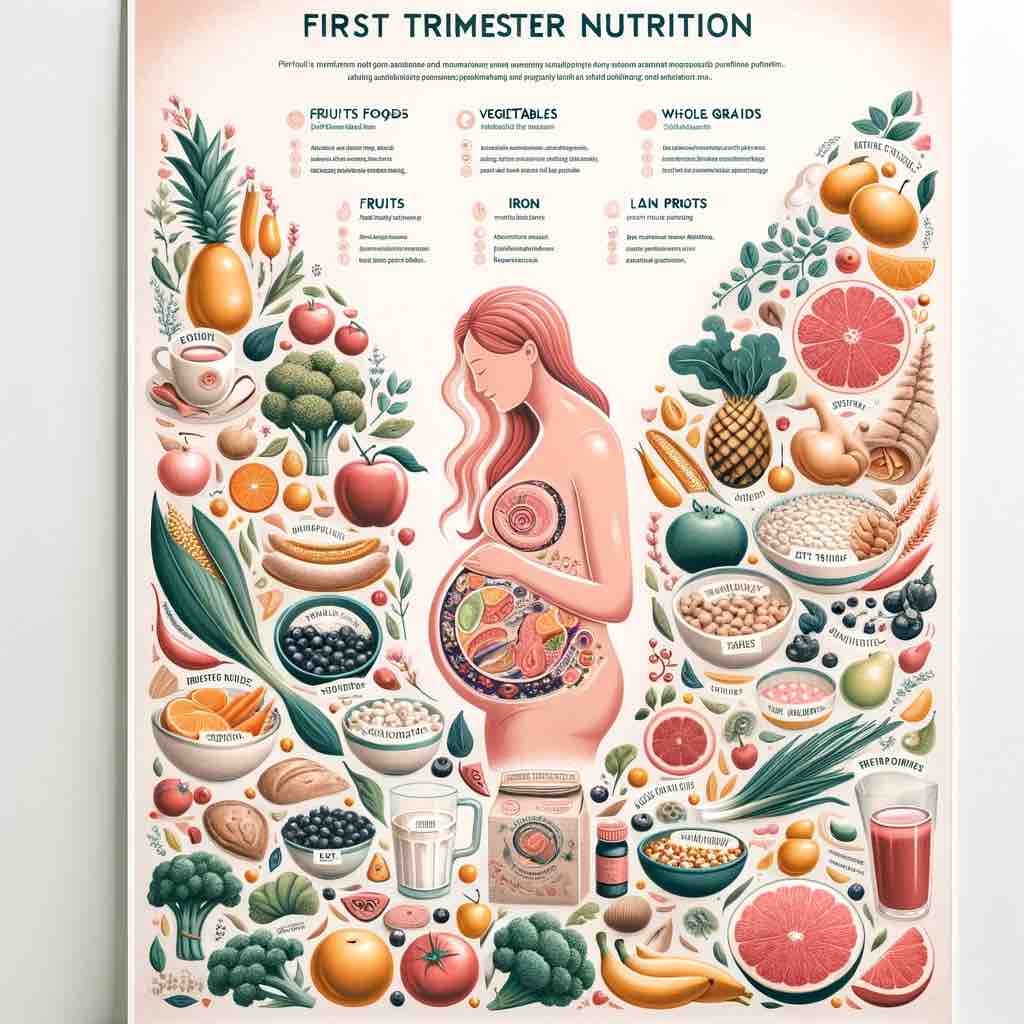
1. Can I Eat Tuna During My First Trimester?
- Answer: Yes, you can eat tuna during your first trimester. However, it’s important to stick to the recommended types and amounts, particularly focusing on low-mercury options like canned light tuna.
2. Is It Safe to Eat Tuna Salad During Pregnancy?
- Answer: Tuna salad can be safe during pregnancy, provided the tuna used is a low-mercury type and consumed within the recommended limits. Be mindful of the additional ingredients in the salad, ensuring they are pregnancy-safe.
3. Can Eating Tuna Help with Baby’s Brain Development?
- Answer: Yes, the omega-3 fatty acids in tuna, particularly DHA, are beneficial for your baby’s brain development. However, balance your intake with other omega-3 sources to minimize mercury exposure.
4. How Much Canned Tuna Can I Safely Eat Each Week?
- Answer: For canned light tuna, up to 12 ounces (340 grams) per week is safe. For albacore tuna, limit it to less than 4 ounces (112 grams) per week.
5. Are There Any Types of Tuna I Should Avoid Completely?
- Answer: It’s best to avoid large, predatory tuna species like bigeye and bluefin, which tend to have higher mercury levels. Also, be cautious with fresh tuna steaks and sushi that contain raw tuna.
6. Can I Replace Tuna with Other Fish in My Pregnancy Diet?
- Answer: Absolutely! Fish like salmon, sardines, and anchovies are excellent alternatives, offering similar nutritional benefits with lower mercury risks.
With these FAQs, we hope to have eased some of your concerns and provided clarity on how to safely include tuna in your pregnancy diet. In the concluding section, we’ll wrap up our guide with some final thoughts.
Conclusion: Navigating Tuna Consumption for a Healthy Pregnancy
As we conclude our deep dive into the topic of tuna consumption during pregnancy, let’s reflect on the key takeaways. Eating tuna can be a nutritious part of your pregnancy diet, but it comes with caveats. The balance between enjoying its health benefits and mitigating the risks associated with mercury exposure is crucial.
Embracing Balance and Variety:
- Moderation is Key: Whether it’s canned light tuna or a freshly cooked tuna steak, moderation remains essential. Adhering to the recommended serving sizes ensures you reap the benefits without unnecessary risks.
- Diversify Your Diet: Don’t rely solely on tuna for your omega-3 intake. Explore other fish and plant-based options to keep your diet varied and interesting.
Staying Informed and Consultative:
- Keep Up-to-Date: Recommendations can change as new research emerges. Stay informed by following credible sources and health advisories.
- Professional Guidance: Always consult with your healthcare provider for personalized dietary advice, especially if you have specific health considerations.
Enjoying Your Pregnancy Journey:
- Healthy Choices for You and Your Baby: Remember, the food choices you make now contribute to your health and the healthy development of your baby.
- Savor the Flavors: Enjoy the culinary journey of pregnancy. Experiment with safe and healthy recipes that include tuna and its alternatives.
We hope this guide has provided you with a clearer understanding of how to safely include tuna in your pregnancy diet. Your journey through motherhood is unique, and so are your dietary needs. Here’s to making informed, healthy choices for you and your little one!
Thank you for joining us on this informative journey. Feel free to share this guide with other expectant mothers and join our community for more insights into pregnancy nutrition!
Call to Action and Engagement
Now that you’re equipped with the knowledge about safely consuming tuna during your pregnancy, we’d love to hear from you and continue this conversation!
Share Your Thoughts and Experiences:
- Join the Community: Have you found creative ways to include tuna in your pregnancy diet? Or perhaps you’ve discovered delicious alternatives? Share your stories and recipes in the comments below. Your insights could inspire and help other expecting mothers.
Stay Connected for More Insights:
- Subscribe and Follow: For more guides like this, subscribe to our blog and follow us on [social media platforms]. We regularly share tips, advice, and updates on pregnancy nutrition and health.
- Ask Questions: If you have any further questions or need clarification on anything discussed in this guide, feel free to reach out. We’re here to support you on your journey to motherhood.
Spread the Knowledge:
- Share with Friends and Family: If you know other pregnant women who might benefit from this guide, please share it with them. The more informed we are, the healthier choices we can make for ourselves and our babies.
Your journey through pregnancy is an incredible one, and making informed nutritional choices is a big part of that journey. Let’s create a community of support and knowledge-sharing, where every expecting mother feels empowered and well-informed. Together, we can navigate the complexities of pregnancy nutrition with confidence and joy!