Empowering Expectant Mothers with Informed Dietary Choices
Navigating dietary decisions during pregnancy can be complex, with certain foods posing risks and others offering essential nutrients. This detailed guide aims to thoroughly inform expecting mothers about safe and unsafe foods during pregnancy, encompassing a broad range of food categories and incorporating key food safety practices to prevent foodborne illnesses.
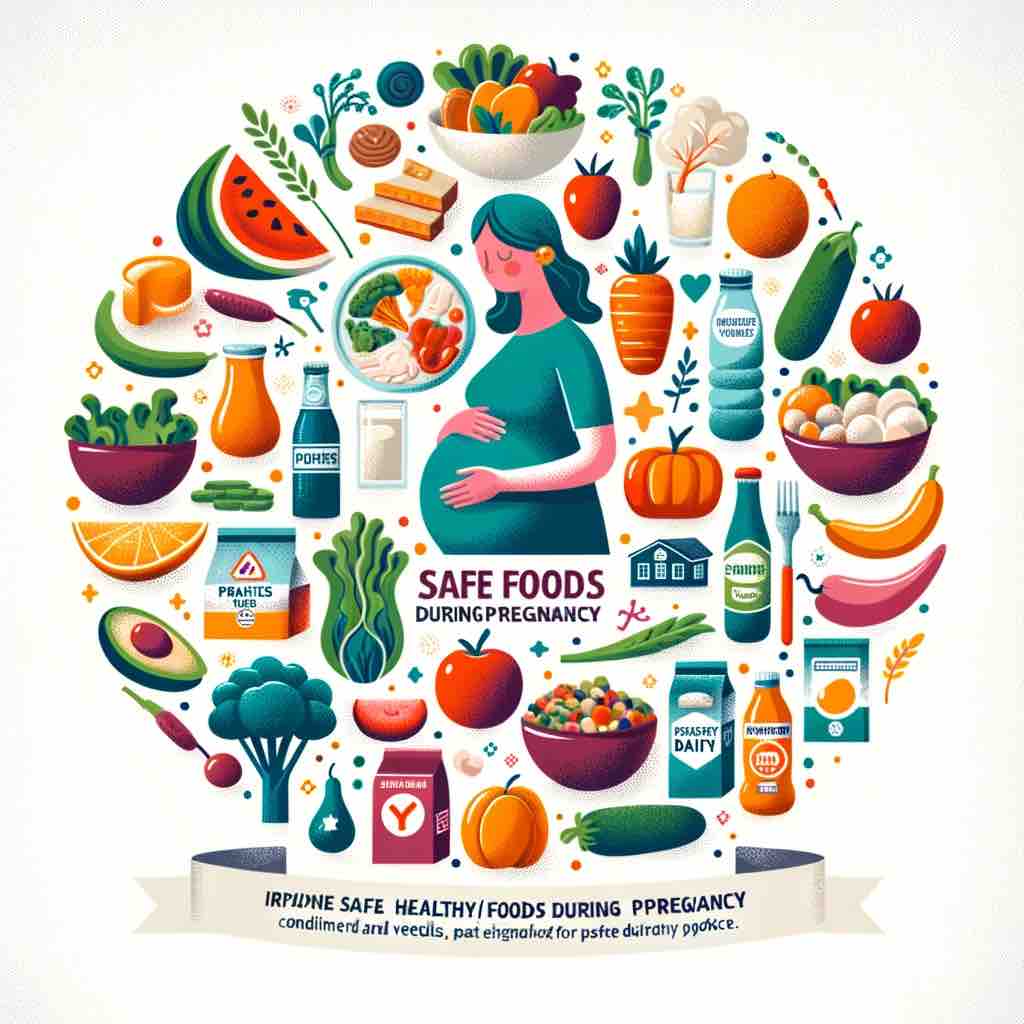
Foods to Embrace for a Healthy Pregnancy
- Fruits and Vegetables: Prioritize a variety of fresh or thoroughly washed fruits and vegetables. Leafy greens, berries, and citrus fruits are excellent for their vitamin content. Avoid pre-cut or pre-washed items unless they are reheated or cooked.
- Whole Grains: Include whole grains like quinoa, brown rice, oats, and whole wheat for essential fiber and nutrients. These aid in digestion and provide sustained energy.
- Lean Proteins: Opt for well-cooked lean meats, poultry, and plant-based proteins like lentils, beans, and tofu. These are crucial for fetal development and maternal health.
- Dairy Products: Focus on pasteurized milk, cheese, and yogurt for calcium and protein. For those who are lactose intolerant, lactose-free dairy or fortified plant-based alternatives are advisable.
Foods to Avoid or Limit During Pregnancy
- Certain Fish and Seafood: While fish is a great source of protein and omega-3 fatty acids, avoid high-mercury fish like shark, swordfish, king mackerel, and tilefish. Limit moderate-mercury fish like tuna, and opt for low-mercury choices like salmon and sardines. Avoid raw or undercooked seafood to reduce the risk of bacterial or parasitic infections.
- Raw or Undercooked Meats and Eggs: To prevent the risk of infections like Toxoplasmosis and Salmonella, avoid raw or undercooked meats, poultry, and eggs. This includes avoiding foods like rare steak, raw cookie dough, and homemade mayonnaise.
- Unpasteurized Foods: Steer clear of unpasteurized milk, cheeses (especially soft cheeses like feta, brie, and blue cheese), and juices, as they can harbor harmful bacteria like Listeria.
- Processed and High-Sugar Foods: Limit intake of processed foods, sugary snacks, and beverages, as they offer little nutritional value and can contribute to excessive weight gain and gestational diabetes.
- Excessive Caffeine and Herbal Teas: Limit caffeine intake to about 200 mg per day. Some herbal teas may not be safe during pregnancy, so consult with your healthcare provider before consumption.
Key Food Safety Practices
- Hygiene and Handwashing: Regularly wash your hands with soap and water, especially before and after handling food, to prevent the spread of bacteria.
- Proper Cooking and Storage: Cook meats, poultry, and seafood to recommended safe internal temperatures. Store perishable items in the refrigerator promptly and consume leftovers within a safe timeframe.
- Avoiding Cross-Contamination: Use separate cutting boards and utensils for raw meat and other foods. Thoroughly clean all surfaces and tools after use.
- Mindful of Food Recalls and Advisories: Stay informed about any current food recalls or safety advisories, especially regarding products prone to contamination.
- Consulting Healthcare Providers for Special Diets: If you have specific dietary needs, allergies, or health conditions, consult with healthcare professionals for tailored advice.
Supplemental Nutrition During Pregnancy
- Prenatal Vitamins and Minerals: Supplements like folic acid, iron, calcium, and vitamin D are often recommended during pregnancy to support fetal development and maternal health. Discuss with your healthcare provider the best options for you.
- Omega-3 Supplements: If fish intake is limited, consider omega-3 supplements, particularly those high in DHA, for fetal brain development.
Conclusion: Prioritizing Safety and Nutrition in Pregnancy
This comprehensive guide is crafted to provide expectant mothers with a deep understanding of dietary do’s and don’ts during pregnancy, covering a wide array of foods and emphasizing the importance of food safety practices. By making informed food choices and adhering to safety guidelines, you can significantly contribute to the health and well-being of both you and your baby. Regular consultations with healthcare providers remain essential to address any dietary concerns and to personalize your nutritional plan.
FAQs for Safe Eating During Pregnancy
1. Q: Can I eat sushi during pregnancy? A: It’s best to avoid sushi made with raw fish due to the risk of bacterial and parasitic infections. Cooked sushi options are generally safe.
2. Q: How much caffeine can I safely consume while pregnant? A: Limit caffeine intake to about 200 mg per day, equivalent to roughly one 12-ounce cup of coffee, to minimize any potential risks to the baby.
3. Q: Are there any cheeses I should avoid during pregnancy? A: Avoid unpasteurized cheeses, including soft cheeses like feta, brie, and blue cheese, unless they’re clearly labeled as pasteurized, to reduce the risk of Listeria contamination.
4. Q: What are the best sources of protein for pregnant women? A: Lean meats, poultry, fish, legumes, tofu, and dairy products are excellent sources of protein. Ensure all meat and poultry are well-cooked to avoid the risk of infection.
5. Q: Is it safe to consume herbal teas during pregnancy? A: Some herbal teas are safe, but others might not be recommended during pregnancy. Consult with your healthcare provider before consuming any herbal teas.
6. Q: What precautions should I take when preparing food at home? A: Practice good kitchen hygiene, wash hands and surfaces often, use separate cutting boards for raw meat and vegetables, and cook foods to their safe internal temperatures.
7. Q: How can I ensure the seafood I consume is safe during pregnancy? A: Choose low-mercury fish like salmon, trout, and sardines, and ensure all seafood is fully cooked. Avoid high-mercury fish and raw or undercooked seafood.
8. Q: What are the risks of consuming unpasteurized milk and dairy products during pregnancy? A: Unpasteurized milk and dairy products can contain harmful bacteria like Listeria, which can lead to severe infections in pregnant women and potentially harm the fetus.
9. Q: Can I eat rare or medium-rare cooked meat while pregnant? A: No, it’s important to eat meat that’s cooked to a safe internal temperature to avoid the risk of bacterial infections like Toxoplasmosis and Salmonella.
10. Q: Are there any specific vegetables or fruits I should avoid during pregnancy? A: Generally, fruits and vegetables are safe and healthy during pregnancy, but ensure they are thoroughly washed to remove any pesticides or bacteria. Avoid pre-cut fruits and vegetables unless you wash them again or cook them.
Blog Tags for the Post
pregnancy nutrition, food safety during pregnancy, healthy pregnancy diet, pregnancy superfoods, gestational diabetes diet, pregnancy food guide, what to eat during pregnancy, foods to avoid in pregnancy, prenatal health, safe pregnancy eating habits