Some evenings beg for ceremony—coupes from the freezer, jiggers lined up like soldiers, a playlist set to “speakeasy.” But most evenings? They just want something generous, bright, and honest. Jim Beam was made for those nights. It’s a bottle that meets you where you are: steady and vanilla-warm as a classic bourbon, playful and fruit-forward as Apple, Vanilla, Orange, Honey, Peach, or Red Stag (Black Cherry). And because our readers keep asking “what’s the best mixer for Jim Beam?” and “what do I mix with the Apple/Vanilla/Orange one?”—we’re going to answer with a human, kitchen-table approach: clear ingredients, simple “how to make” steps, smooth transitions from one idea to the next, and plenty of friendly asides you’ll actually use.
We’ll start with the fastest answer—so you can pour while you read. Then we’ll move through classic bourbon serves (highball, cola, tonic, lemonade, iced tea), and glide, glass by glass, into each flavor expression with official brand anchors where helpful and a bunch of Masala Monk twists to keep things personal. Along the way, you’ll notice more connective tissue: why a pinch of salt matters, when to choose ginger ale over ginger beer, how to scale for friends, and what to reach for when the weather turns. Think of this as a conversation in a warm kitchen—one hand on the bottle, the other rummaging for citrus—rather than a lecture across a bar.
The 10-Second Answer (so you can pour now, not later)
If you remember only one line, let it be this: use a tall glass, pack it with fresh ice, and aim for 1 part Jim Beam to 2–3 parts mixer. Then add a citrus wedge, give a very short stir, and taste. Want spice and lift? Choose ginger ale or ginger beer. Prefer a crisp, bourbon-forward feel? Go soda water with a lemon wheel. Craving comfort? Cola with a squeeze of lime never misses. Meanwhile, sunny afternoons adore lemonade and iced tea, and fruit-leaning expressions glow with cranberry, apple, or even pineapple. With that out of the way, let’s settle in and make you a short list you’ll reach for again and again.
1) Best Mixer for Jim Beam Bourbon (Highball, Cola, Tonic, Lemonade & Iced Tea)
Before we talk flavors, let’s treat the classic white-label bourbon the way it deserves: tall, chilled, and sparkling. Because when bourbon meets bubbles properly, the drink doesn’t just quench—it floats.
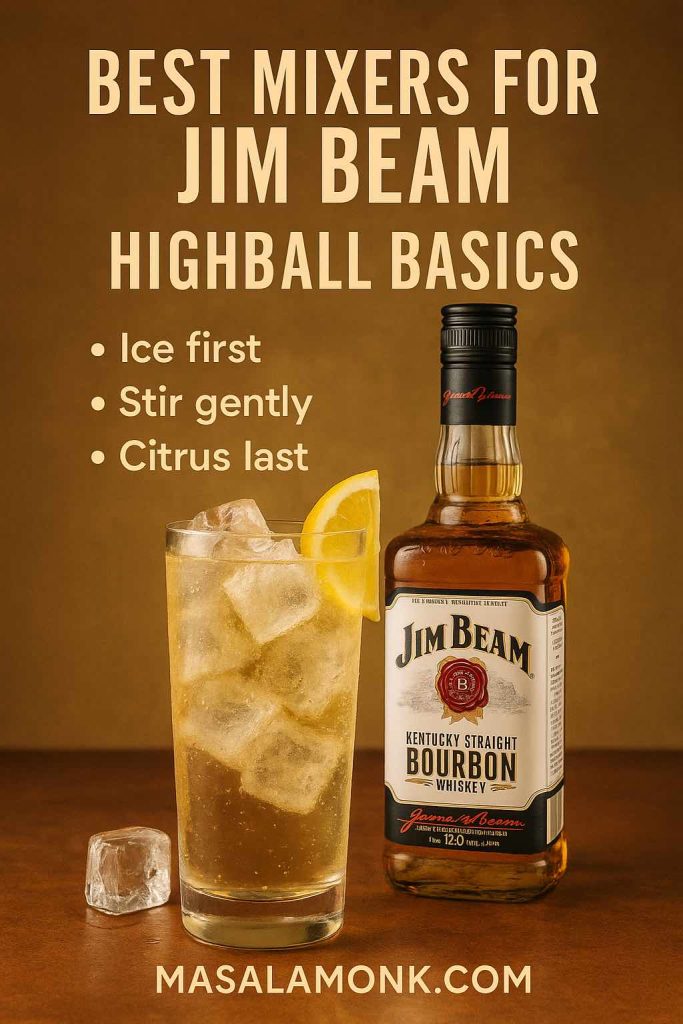
Jim Beam Highball (crisp, bright, repeatable)
There’s a small ritual here that pays off: cold topper, plenty of ice, a gentle stir. Not fussy—just respectful.
Ingredients (1 drink)
- 60 ml Jim Beam Bourbon
- 120–180 ml ginger ale (soft spice) or soda water (bone-dry and crisp)
- Lemon wheel • Tall glass • Fresh ice
How to make
Fill a tall glass with ice. Add bourbon. Top with chilled ginger ale (or soda). Stir briefly—three small turns. Rest a lemon wheel on top, and taste before you tweak. If you want more fizz, add a little more mixer; if you want more bourbon, well, top yourself up.
Why it works
Ginger ale flatters Beam’s vanilla and caramel; soda lets the grain and oak step forward. Because the stir is short, you keep the fizz; because the ice is fresh and the glass is tall, the drink stays lively from first sip to last.
Quick variations
- Zesty Highball: two dashes orange bitters before you top; express a lemon peel for fragrance.
- Tea Highball: top with unsweetened iced tea and a squeeze of lemon—smoother, food-friendlier, very “second glass.”
- Half-and-Half Mule: split your topper ½ ginger beer / ½ soda water for mule spice without extra sweetness.
- Salt-Lime Cooler: a tiny pinch of black salt on the lemon wheel; it sharpens citrus and makes the sip feel colder.
(If you enjoy a little technique reading later, this quick primer on highball ratios and chilled components is handy: Highball technique overview.)
Also read: Earl Grey Elegance: 5 Bergamot-Spiced Iced Tea Cocktails for Sophisticated Tuesday Sips
Jim Beam & Cola (classic comfort that benefits from one tiny trick)
There’s a reason this pairing never left the party. Still, a squeeze of lime before you drop the wedge in keeps the drink bright instead of syrupy.
Ingredients (1 drink)
- 60 ml Jim Beam Bourbon
- 150–180 ml cola
- Fresh ice • Lime wedge
How to make
Glass full of ice; bourbon in; cola on top; lime squeezed and dropped. Then a calm, single stir.
Two easy upgrades
- Spice-Cola: one dash Angostura + an expressed orange peel; now it tastes like a proper cocktail.
- Cola-Coffee Float (late night): 45 ml Beam + 90 ml cola + 30 ml chilled coffee over a big cube; orange twist.
Bourbon & Tonic (the sleeper hit you never asked for)
Tonic’s quinine brings a clean, brisk snap that resets your palate between sips. It surprises people—in the best way.
Ingredients (1 drink)
- 60 ml Jim Beam Bourbon
- 150–180 ml tonic water
- Tall glass • Ice • Lime wedge
How to make
Bourbon in a tall, ice-filled glass; top with tonic; delicate stir; lime wedge. Start at a 1:2 ratio and adjust to taste, because tonic’s personality is assertive.
Lemonade & Iced Tea (porch-ready and sessionable)
- Bourbon Lemonade: 60 ml Beam + 150–180 ml lemonade over ice; lemon wheel + mint.
- Bourbon Tea Highball: 60 ml Beam + 150–180 ml unsweetened iced tea; squeeze of lemon.
- Arnold Bourbon (half & half): 60 ml Beam, then equal parts iced tea and lemonade to top; lemon wedge.
Because these long drinks scale so well, you can chill the topper in the fridge, pre-cut citrus, and pour to order in seconds. Friends will think you planned; secretly, you barely did.
2) Jim Beam Apple Mixers — Crisp, Sparkling, Crowd-Pleasing
Now that the bourbon is humming, let’s turn to Apple—the friendliest of the flavors. It loves clean fizz and bright citrus; it also loves company. Two official serves give you a solid backbone; from there, the riffs write themselves.
Orchard Twist (official baseline, then our riffs)
This is the “friends are five minutes away” drink: apple whiskey, cranberry, a lift of soda, and a lime wedge. It’s ruby in the glass and gone before it waters down. If you want the brand’s minimalist baseline, see Official Orchard Twist — Jim Beam Apple + Cran + soda.
Ingredients (1 drink)
- 60 ml Jim Beam Apple
- 60 ml cranberry juice
- 60–90 ml soda water
- Ice • Lime wedge
How to make
In a tall ice-filled glass, add Apple, then cranberry, then soda; gentle stir; lime wedge. That’s it—company-proof.
Masala Monk riffs
- Apple-Cran Fizz (table ratio): as above; if your cranberry is extra-tart, add 5–7 ml simple syrup.
- Apple Ginger Pop: top with dry ginger ale + a fast lemon squeeze; garnish with a thin fan of grated apple.
- Masala Apple Shandy: make your topper half lemonade, half soda; dust a pinch of black salt on the rim.
- Warm Orchard (winter): 45 ml Apple + hot apple cider + a thin slice of fresh ginger; cinnamon stick stirrer.

Apple Highball (official spritz, clean and lean)
This is Apple at its simplest: bright, sparkling, and very refillable. The brand’s version is here: Official Apple Highball — Jim Beam Apple + soda.
Ingredients (1 drink)
- 60 ml Jim Beam Apple
- 120–180 ml soda water
- Lemon wheel • Ice
How to make
Apple over ice, soda to the top, brief stir, lemon wheel. If you want color and bite, swap half the soda for cranberry.
Two gentle variations
- Berry Apple: 60 ml Apple + 60 ml cranberry + 60–90 ml soda; lemon wheel.
- Spearmint Apple: clap a few mint leaves to perfume the glass (don’t muddle hard).
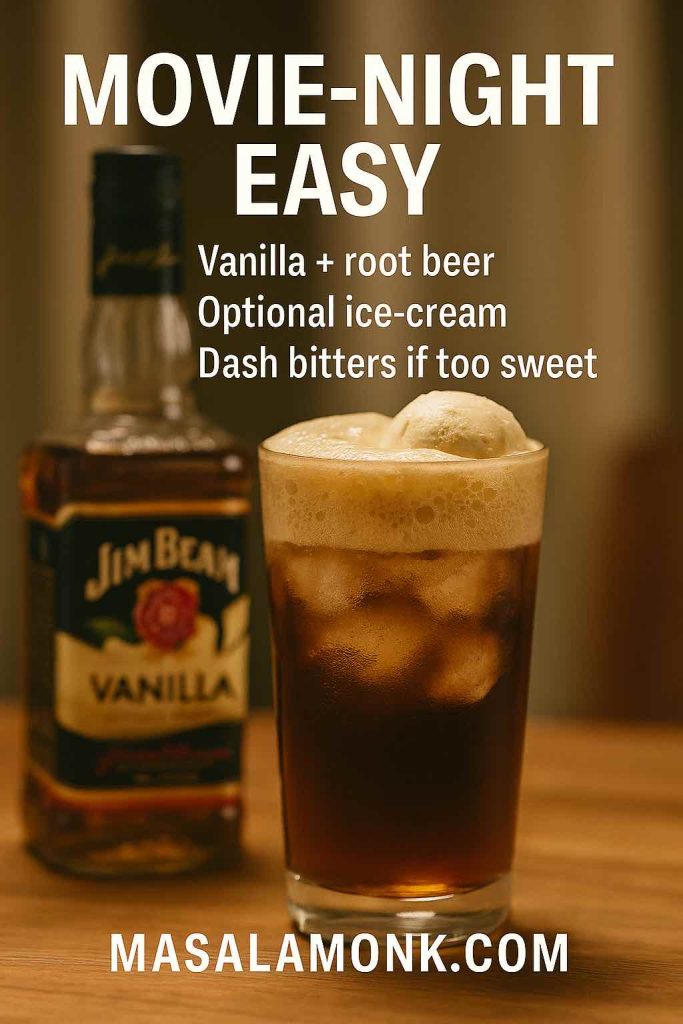
3) What to Mix with Jim Beam Vanilla — Dessert-Adjacent, Movie-Night Perfect
If Apple is an afternoon picnic, Vanilla is movie night on the couch—nostalgic, mellow, and sneakily sippable. Naturally, the best mixers feel like comfort food in a glass.
Vanilla & Root Beer Float (nostalgia without the fuss)
Ingredients (1 drink)
- 45–60 ml Jim Beam Vanilla
- Root beer to top
- Ice • Optional small scoop vanilla ice cream
How to make
Ice in, Vanilla in, root beer up to the top, and—if dessert is calling—slip in that small scoop. Because root beer is already sweet, you won’t need extra syrup.
Coffee-Vanilla Highball (the “one more episode” pour)
Ingredients (1 drink)
- 45 ml Jim Beam Vanilla
- 90–120 ml cold brew coffee
- 15 ml cream or half-and-half
- Pinch cinnamon • Ice
How to make
Vanilla over ice, add cold brew, float the cream, dust the cinnamon, and give one gentle lift with the spoon so the layers mingle slowly.
4) Jim Beam Orange — Mule Magnet, Citrus Charmer (and yes, Ginger Sour)
Ginger beer, lime, ice: Orange practically begs for that trio. Yet, because life is full of small surprises, it also shines shaken—especially with ginger syrup—and, on “I’m already late” nights, with a fast lemon-lime soda you can pour without thinking.
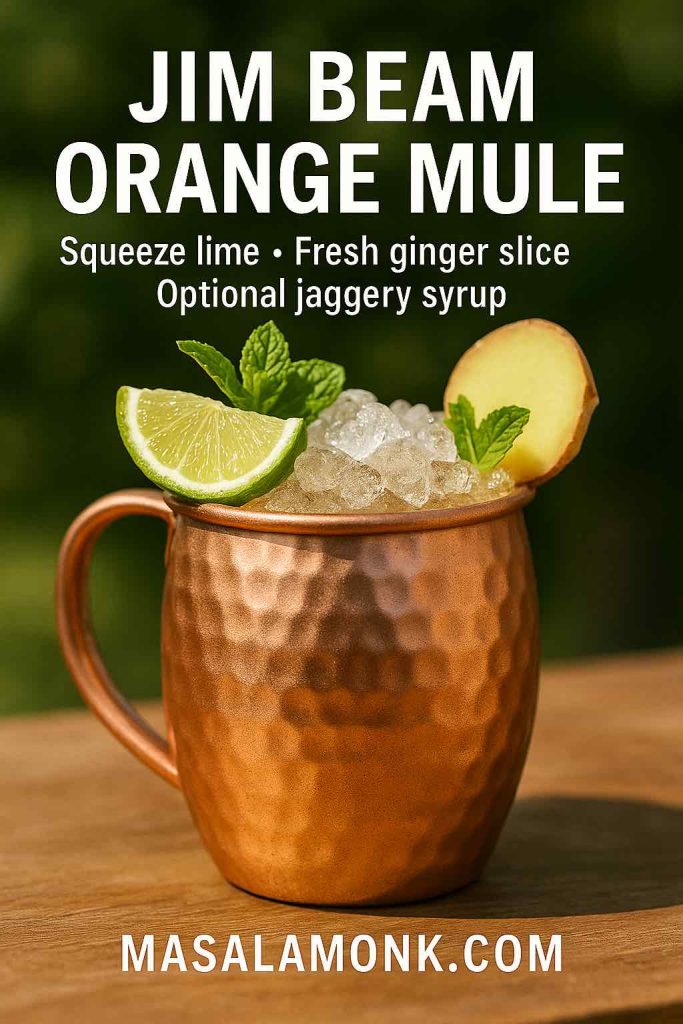
Jim Beam Orange Mule (official, tall and refreshing)
The crowd-pleaser. It’s fizzy, aromatic, and dangerously easy to refill. For the brand’s baseline, see Official Jim Beam Orange Mule — brand recipe.
Ingredients (1 drink)
- 60 ml Jim Beam Orange
- 120–150 ml ginger beer
- 10 ml fresh lime juice (or a small orange-and-lime blend)
- Optional 5–10 ml simple syrup if your ginger beer is ultra-dry
- Ice • Orange peel + mint (or lime wedge) • Copper mug or tall glass
How to make
Fill the mug with ice, add Orange, squeeze in lime, top with ginger beer, and give one gentle roll with your spoon. Garnish generously—it’s part of the joy.
Masala Monk twists
- Monk’s Spicy Mule: 2 dashes Angostura + thin slice fresh ginger; swap simple for ½ tsp jaggery syrup (1:1).
- Tamarind Mule: ½ tsp tamarind syrup for tang; pinch black salt on the orange peel.
- Low-ABV Spritz: 45 ml Orange + 90 ml ginger beer + 60 ml soda; mint bouquet.
- Zero-Proof “Mule”: orange cordial + ginger beer + lime in a mule mug (clearly non-alcoholic).
Orange Crush (official, shaken and sunny)
A citrusy shake with a soda lift so it reads lively instead of heavy. See Official Jim Beam Orange Crush — brand cocktail.
Ingredients (1 drink)
- 45 ml Jim Beam Orange
- 30 ml orange juice
- 20–22.5 ml lemon juice
- 10–15 ml simple syrup
- Ice • Soda to top • Orange wheel
How to make
Shake Orange, citrus, and syrup hard with ice. Strain over fresh ice. Top with a light splash of soda. Orange wheel to finish.
Two simple riffs
- Salted Citrus Crush: tiny pinch black salt before topping; mint for aroma.
- Grapefruit Crush: split the OJ with pink grapefruit (50:50) for a drier finish.
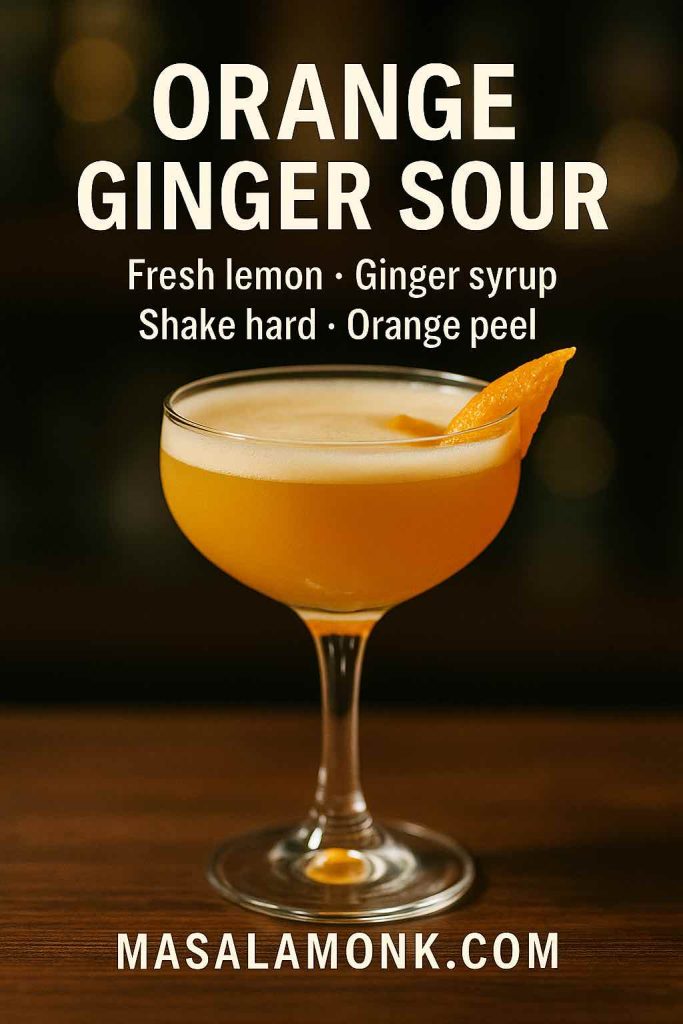
Orange Ginger Sour (because people keep asking)
This covers that “jim beam orange ginger sour” long-tail with a balanced, bar-quality sour you can shake at home.
Ingredients (1 drink)
- 60 ml Jim Beam Orange
- 22.5 ml fresh lemon juice
- 10–12.5 ml ginger syrup (or reduce ~60 ml ginger beer down to ~20 ml by simmering, then cool)
- Optional: 1 egg white
- Ice • Orange peel
How to make
Dry shake (if using egg), then add ice and shake until the tin frosts. Fine strain into a chilled coupe—or over a single large cube if you like it on the rocks. Express orange peel across the top; serve immediately.
Orange + Lemon-Lime (Sprite) Highball (for the “pour and smile” crowd)
Ingredients (1 drink)
- 60 ml Jim Beam Orange
- 150–180 ml lemon-lime soda
- Ice • Lime wedge
How to make
Build over ice, brief stir, lime wedge. No measuring spoons, no apologies.
5) What to Mix with Jim Beam Honey — Soft, Friendly, Sunshine-Ready
If a flavor could smile, Honey would. It prefers sunlight, laughter, and tall glasses. Keep it bright; keep it simple; and watch the pitcher empty itself.

Honey Lemonade Cooler (the “one more glass” special)
Ingredients (1 drink)
- 60 ml Jim Beam Honey
- 150–180 ml lemonade
- Ice • Mint sprig
How to make
Honey over ice, lemonade to the top, one gentle nudge with the spoon. Mint goes in last so the aroma hits first.
Variations
- Honey-Tea Highball: 60 ml Honey + 150 ml unsweetened iced tea + lemon wheel.
- Honey-Ginger: 60 ml Honey + 120–150 ml dry ginger ale + lemon squeeze.
- Hot Honey Cider: 45 ml Honey + hot apple cider + cinnamon stick; a flamed orange peel if you’re feeling fancy.
6) What to Mix with Jim Beam Peach — Porch-Perfect, Picnic-Ready
As the light softens and conversation slows, Peach slides happily into tea and lemonade. These are the drinks you’ll set in a jug on the table and refill without thinking.
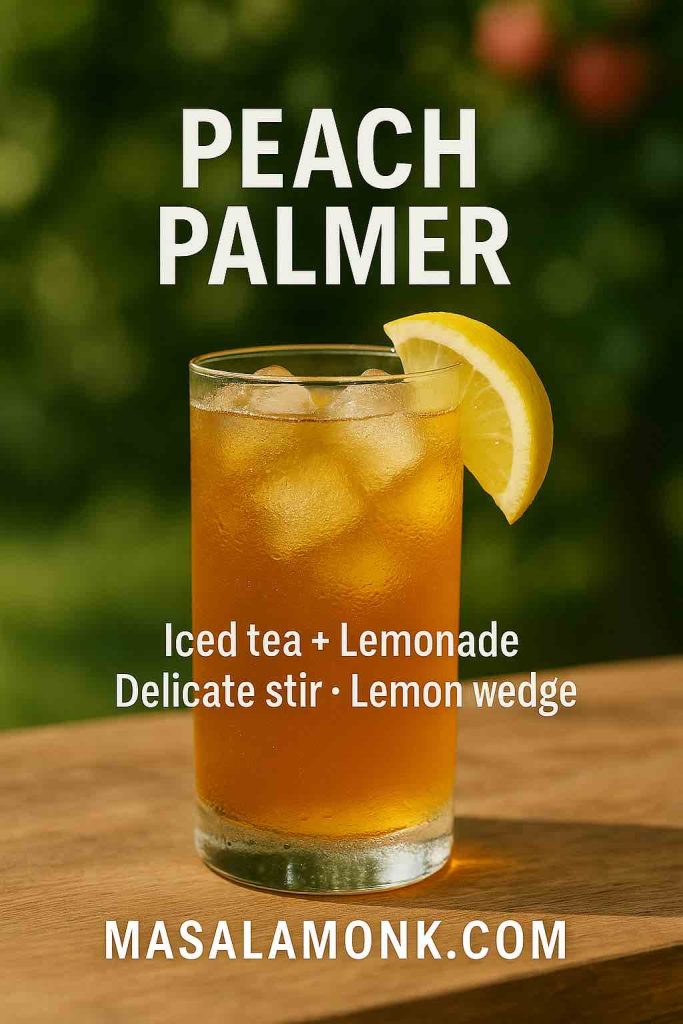
Peach Palmer (half tea, half lemonade, all smiles)
Ingredients (1 drink)
- 45 ml Jim Beam Peach
- 90 ml unsweetened iced tea
- 60 ml lemonade
- Ice • Lemon wedge
How to make
Peach over ice, add tea, float lemonade, and give a delicate stir. Lemon wedge to finish. If you prefer bubbles, swap lemonade for lemon-lime soda.
Variations
- Ginger-Peach Fizz: sub the lemonade for dry ginger ale; add 1 dash Angostura.
- Cran-Peach Spritz: 45 ml Peach + 60 ml cranberry + 60–90 ml soda; lime wheel.
7) Jim Beam Red Stag (Black Cherry) — Cola, Soda & a Little Lime
Red Stag is cherry with a bourbon backbone—no wonder it loves cola. Yet it’s just as happy going drier with soda water and lime. For extra context and pairings in the brand’s own words (including iced tea and lemonade), skim Red Stag product page — cherry with cola or with iced tea/lemonade.
Red Stag & Cola (official, lime-balanced)
If you want the tidy baseline, here’s the brand’s page: Official Red Stag & Cola — brand serve.
Ingredients (1 drink)
- 45–60 ml Red Stag
- 135–180 ml cola
- Ice • Lime wedge
How to make
Build over ice, squeeze the lime, then a gentle stir. That squeeze is everything.

Red Stag & Soda Highball (official, cleaner and brighter)
Brand anchor here: Official Red Stag & Soda Highball — brand serve.
Ingredients (1 drink)
- 60 ml Red Stag
- 150 ml soda water
- Ice • Lime wedge
How to make
Build over plenty of ice, quick stir, lime wedge.
Red Stag Half & Half (tea + lemonade long drink)
If you like half-tea, half-lemonade, the brand even spells it out: Red Stag Half & Half — brand recipe.
Home-bar version
- 45–60 ml Red Stag
- 90 ml unsweetened iced tea
- 90 ml lemonade
- Tall glass • Ice • Lemon wedge
Our riffs
- Cherry-Lime Rickey: Red Stag + soda + 10 ml fresh lime + 2 dashes Angostura; lime wheel + cherry.
- Tea-Time Highball: topper is ½ iced tea / ½ lemonade; lemon wedge and a gentle roll.
- Smoked Cherry Old Fashioned (quick): 60 ml Red Stag + 1 barspoon rich syrup (2:1) + 2 dashes bitters; big cube; orange peel.
8) What to Mix with Jim Beam Fire — Three Fast Winners
Fans keep asking, and these three land every time—no extra bells required.
- Cream Soda Fire: 45–60 ml Jim Beam Fire + 150 ml cream soda over ice; cinnamon stick.
- Hot Apple Fire: 45 ml Fire into hot apple cider; lemon peel + cinnamon.
- Ginger Fire Highball: 60 ml Fire + 120–150 ml dry ginger ale + lemon wedge.

Because Fire brings cinnamon sweetness, keep things lean—no syrup unless you truly love it sweet.
9) Bourbon Cream & Winter Bottles — Cozy Weather, Simple Joy
When the weather turns, Bourbon Cream becomes your shortcut to warm, velvety drinks that feel like a blanket. Likewise, any wintery limited release can follow the same playbook.
Bourbon Cream Coffee (silky, café-cozy)
Ingredients (1 drink)
- 45 ml Bourbon Cream
- Hot coffee to fill
- Whipped cream, dusted with cocoa
How to make
Warm mug; Bourbon Cream in; coffee on top; cream to crown. Consequently, you get gentle alcohol heat, rounded sweetness, and coffee aromatics in three friendly moves.
A simple float for dessert
- Adult Cola Float: 45 ml Bourbon Cream + 120 ml cola over ice; tiny scoop vanilla ice cream optional.
Seasonal note (Winter Reserve & friends)
If a winter bottle shows up in your market, treat it like Bourbon Cream for cozy serves (coffee, cocoa) or like straight bourbon for hot toddies and hot cider. The methods and ratios above still apply, and your guests will thank you when the wind picks up.
10) Two Timeless Jim Beam Cocktails (Whiskey Sour & Old Fashioned)
Sometimes the best “mixer” is simply lemon, sugar, and patience with ice. With these two, you get grown-up balance with zero drama—and because they’re anchored to global standards, they’re repeatable even on autopilot.
Whiskey Sour (IBA baseline, scaled for home jiggers)
For the canonical baseline, the Whiskey Sour — IBA official spec lists 45 ml whiskey, 25 ml lemon, 20 ml simple syrup, and an optional egg white. Meanwhile, our build nudges the whiskey to 60 ml—friendlier for common 30 ml jiggers and a big cube—while keeping the balance crystal-clear.
Ingredients (1 drink)
- 60 ml Jim Beam Bourbon (IBA lists 45 ml; we scale)
- 22.5 ml fresh lemon juice
- 15 ml simple syrup
- Optional: 1 egg white
- Ice • Lemon peel • Cherry (optional)
How to make
Dry shake (if using egg) to whip the texture, then shake hard with plenty of ice. Strain over a large cube into a rocks glass. Express a lemon peel over the top; if you’re in a retro mood, add a cherry.
Why Beam sings here
Beam’s vanilla and gentle oak soften lemon’s edges, so you can keep syrup modest. Consequently, the drink finishes clean rather than cloying—a second-round kind of sour.

Old Fashioned (IBA structure, modern home-bar method)
The Old Fashioned — IBA official spec is famously spare: sugar, bitters, whiskey, water. When simplicity rules, technique whispers the loudest.
Ingredients (1 drink)
- 60 ml Jim Beam Bourbon
- 1 sugar cube (or 7.5 ml simple syrup)
- 2 dashes Angostura bitters
- Tiny splash water
- Big clear ice • Orange peel
How to make
If using a cube, place it in a rocks glass with bitters and a few drops of water; muddle gently to dissolve. Add bourbon and ice; stir until the glass is cold and the surface looks glossy. Strain onto a big cube. Express an orange peel and serve.
Two tasteful upgrades
- Swap white sugar for jaggery syrup (2:1) to echo Beam’s vanilla and caramel.
- Add a single dash of orange bitters if you like a citrus-bright finish.
How to Drink Jim Beam (a beginner-to-enthusiast path)
Start with a Highball: 1 part bourbon to 2–3 parts fizz (ginger ale for spice, soda water for crispness), a pile of fresh ice, and a lemon wedge. If you prefer sweeter, try Bourbon & Cola with a firm squeeze of lime. When you’re ready for a “proper cocktail,” shake a Whiskey Sour—bright, silky, impossible not to like. Next, graduate to the Old Fashioned—still simple, just more spirit-forward. After that, let curiosity pull you across the flavored range: Apple for spritzy afternoons; Orange when you’re craving a mule; Vanilla for dessert-ish nightcaps; Honey and Peach for picnics and long lunches; and Red Stag for cola nights and tea-lemonade afternoons. Because this isn’t about mastering tricks; it’s about learning which small choices make your glass taste like you.
Party Batching, Glassware & Ice (the quiet details that change everything)
Batching for four highballs
- 240 ml Jim Beam (classic or flavored)
- 480–720 ml chilled topper (soda, ginger ale, lemonade, or iced tea)
- Pre-cut citrus • Extra-cold ice
How to serve
Keep the topper very cold in the fridge. Pour bourbon over ice in each glass, top from the chilled bottle, and stir briefly. Consequently, you preserve carbonation while still marrying flavors. Add citrus at the last second so the oils are fresh.
Glassware
- Highballs & long drinks: tall, straight-sided glasses keep bubbles tight and the profile clean.
- Sours (up or on the rocks): a chilled coupe for “up”; a rocks glass with a big cube for “down.”
- Old Fashioned: a heavy rocks glass with a wide mouth for easy peel expression.
Ice
- For tall drinks, more (and larger) ice means less dilution and longer fizz.
- For stirred or spirit-forward drinks, a single big cube melts slowly and keeps the texture silky.
- For shakes, don’t be shy—hard shaking makes cold, airy sours that feel luxurious without extra sugar.
Troubleshooting & Taste Tweaks (so every pour lands)
- Too sweet? Add a squeeze of lemon or lime; or swap half your topper for soda water.
- Too sharp? Add 5 ml simple syrup in sours, or choose ginger ale instead of soda in highballs.
- Too flat? Your mixer wasn’t cold enough, your stir was too vigorous, or the glass was warm. Chill what you can and stir less.
- Not enough flavor? Increase the spirit to 75 ml, or add a dash of bitters to deepen the finish.
- Want lighter ABV? Drop spirit to 45 ml and extend the topper; or use the Low-ABV Spritz variations above.
- No fresh citrus? Express a peel (even from an older lemon or orange) over the drink—the oils go a long way.
Pantry-Powered Twists (little moves, big returns)
Because your kitchen is already a flavor lab, here are a few reliable upgrades:
- Jaggery syrup (2:1): earthy, mineral sweetness that flatters bourbon; unbeatable in an Old Fashioned.
- Black salt (kala namak): the tiniest pinch on a citrus garnish lifts fruit and tames sweetness.
- Fresh ginger: a thin slice in mules and highballs adds aroma and bite—especially with Jim Beam Orange.
- Green chilli (nimbu-mirch style): a tiny slice floated on a Whiskey Sour foam gives aroma first, heat second.
- Masala chai: brew strong, chill, and use in place of plain iced tea with Peach or Honey; the spices echo bourbon’s caramel.
- Citrus zest oils: express peels over the glass (don’t just toss them in); the first sip becomes a little ceremony.
A tiny cooking aside (for those marinade & BBQ quereis)
While this guide is all about drinks, Jim Beam plays nicely in the kitchen, too. If you’re fielding “marinade” or “BBQ sauce” questions, steer folks to a quick glaze: equal parts ketchup and brown sugar, a healthy splash of Beam, a dash of Worcestershire, and a pinch of chilli flakes. Simmer until glossy and brush onto grilled chicken or ribs at the very end so the sugars don’t burn. Not a drink, but a weeknight hero.
Responsible Enjoyment (because good nights end well)
Measure your pours, sip water between rounds, and plan your ride before the bottle opens. Label pitchers when you batch, offer a zero-proof option that’s just as pretty as the “real” thing, and keep an eye on friends who pour generously. The best cocktail, after all, is the one everyone remembers fondly in the morning.
Helpful official Links & Sources mentioned above
- Official Jim Beam Orange Mule — brand recipe — Orange + ginger beer + citrus; tall, fizzy build. Jim Beam®
- Official Jim Beam Orange Crush — brand cocktail — citrusy shaker, topped with soda. Jim Beam®
- Official Orchard Twist — Jim Beam Apple + Cran + soda — crisp and bright; lime wedge. Jim Beam®
- Official Apple Highball — Jim Beam Apple + soda — clean apple spritz with citrus hint. Jim Beam®
- Official Red Stag & Cola — brand serve — cola highball with lime. Jim Beam®
- Official Red Stag & Soda Highball — brand serve — drier cherry-lime cooler. Jim Beam®
- Red Stag product page — cherry with cola or with iced tea/lemonade — more pairing ideas in the brand’s own words. Jim Beam®
- Red Stag Half & Half — brand recipe — tea + lemonade + Red Stag; easy long drink. Jim Beam®
- Whiskey Sour — IBA official spec — canonical 45:25:20 sour. IBA
- Old Fashioned — IBA official spec — sugar, bitters, whiskey, water. IBA
- Highball technique & typical ratios (Food & Wine overview) — chilled components, gentle stir, 1:2–1:3 range. Food & Wine
Last sip: good home bartending isn’t about impressing the room; it’s about small, caring choices—cold mixers, clean ice, a bright wedge of citrus, and a moment to taste before you tweak. With Jim Beam, that’s usually all it takes. Tonight, let the bottle meet you where you are, and pour something you’ll happily make again tomorrow.
FAQs
1) What’s the best mixer for Jim Beam?
First things first: ginger ale is the best mixer for Jim Beam if you want easy spice and gentle sweetness. Next best, for a drier, bourbon-forward sip, is soda water with a lemon wheel. In short, start at 1 part Jim Beam : 2–3 parts mixer, lots of ice, quick stir.
2) How do I make a simple Jim Beam highball at home?
To begin, fill a tall glass with fresh ice. Then pour 60 ml Jim Beam and top with 120–180 ml chilled ginger ale (or soda water). Finally, give three gentle stirs and add a lemon wheel. This crisp Jim Beam highball is the baseline for most easy Jim Beam mixers.
3) What mixes well with Jim Beam Apple?
For starters, try cranberry + soda (clean, tart, and sparkling). Moreover, dry ginger ale with a squeeze of lemon is wonderfully balanced. Meanwhile, in cooler weather, go warm with hot apple cider and a thin slice of fresh ginger—an instant crowd-pleaser for Jim Beam Apple mixers.
4) What can I mix with Jim Beam Vanilla for dessert vibes?
Begin with a root beer float (add a small scoop of vanilla ice cream if you like). Next, for a cozier spin, go cold brew + a splash of cream with a pinch of cinnamon. Both are nostalgic, easy, and highly appreciated “drinks with Jim Beam Vanilla.”
5) Besides the Mule, what else pairs with Jim Beam Orange?
Naturally, the Jim Beam Orange Mule (ginger beer + lime) is a classic. However, for a shaken option, make an Orange Ginger Sour (lemon + ginger syrup, shaken hard). On busy nights, simply top with lemon-lime soda and add a lime wedge—fast Jim Beam Orange cocktails that still feel bright.
6) What’s a quick, reliable drink with Jim Beam Honey?
Start with lemonade—sunny and refreshing. Also great: unsweetened iced tea for a smoother finish, or dry ginger ale with a lemon squeeze when you want extra zip. These are no-brainer Jim Beam Honey cocktails.
7) What should I mix with Jim Beam Peach?
First, reach for iced tea + lemonade (a Peach Palmer) for a porch-perfect long drink. Alternatively, choose ginger ale for subtle spice, or cranberry + soda for a pink, patio-ready spritz. All three are strong Jim Beam Peach cocktails for summer.
8) Red Stag mixed drinks—cola or soda?
Both, but for different moods. With cola, add a lime squeeze so it doesn’t read too sweet. Meanwhile, with soda water, you’ll get a cleaner cherry-lime feel—lighter, longer, and great with food. Consequently, Red Stag mixed drinks are an easy win at parties.
9) I’m new to bourbon—how should I drink Jim Beam?
First, keep it simple with a highball (1:2 to 1:3). Next, when you’re ready for a classic, shake a Whiskey Sour Jim Beam (bourbon + lemon + a touch of syrup). Finally, graduate to an Old Fashioned Jim Beam (sugar + bitters + bourbon) when you want spirit-forward elegance.
10) What ratio works best for Jim Beam mixers?
As a rule of thumb, use 1 part Jim Beam to 2–3 parts mixer. Moreover, the taller the glass (and the colder the topper), the longer your bubbles last. As a result, your Jim Beam mixed drinks stay lively from first sip to last.
11) Can I make a Whiskey Sour with Jim Beam?
Absolutely. For Whiskey Sour Jim Beam, shake 60 ml bourbon + 22.5 ml lemon + 15 ml simple (optional egg white). Then strain over a big cube, add a lemon peel, and enjoy. Meanwhile, keep sugar modest—Beam’s vanilla notes already round the edges.
12) Is Jim Beam good in an Old Fashioned?
Yes. For Old Fashioned Jim Beam, stir 60 ml bourbon with a sugar cube (or 7.5 ml simple) and 2 dashes bitters, then serve over a big cube with an orange peel. Furthermore, swapping simple for jaggery syrup adds a warm, caramel depth that suits Beam.
13) Is Jim Beam and Sprite a good idea?
Indeed. Jim Beam and Sprite (or any lemon-lime soda) is bright and ultra-easy. Even better, Jim Beam Orange and Sprite tastes like a fizzy creamsicle—just add a lime wedge and you’ve got a 10-second highball.
14) Does Jim Beam work with tonic water?
Yes—surprisingly well. Bourbon and tonic is brisk and aromatic, especially with a lime wedge. Therefore, if you’re exploring best mixer for Jim Beam options beyond ginger ale, tonic is a sophisticated, summer-friendly choice.
15) What mixes well with Jim Beam Fire?
Try cream soda (dessert-leaning and quick), hot apple cider (cozy and seasonal), or dry ginger ale + lemon (clean and snappy). Consequently, what to mix with Jim Beam Fire becomes a three-option answer you can pour in seconds.
16) What are the best non-carbonated mixers for Jim Beam?
When you want less fizz, choose unsweetened iced tea, lemonade, cranberry, apple, or even pineapple juice. Moreover, a tiny pinch of black salt on the citrus garnish can lift fruit and tame sweetness—small move, big result.
17) How can I batch Jim Beam cocktails for a party?
Start with the friendly template: for four Jim Beam mixed drinks, use 240 ml Jim Beam and 480–720 ml chilled mixer (soda, ginger ale, lemonade, or iced tea). Then pour bourbon over ice in each glass, top from the chilled bottle, give a brief stir, and add citrus last for maximum aroma.
18) Which garnishes make Jim Beam mixers pop?
First and foremost, fresh citrus—lemon wheels, lime wedges, and expressed orange peels. Next, consider two dashes of bitters to add backbone. And finally, for a Masala Monk twist, a pinch of black salt or a thin slice of fresh ginger can transform a good drink into a great one.
19) How do I lower ABV but keep flavor in Jim Beam cocktails?
Simply reduce the pour to 45 ml and extend the topper, or choose our Low-ABV Spritz variations (spirit + ginger beer + extra soda). Meanwhile, crushed ice and taller glasses make lighter drinks feel just as satisfying.
20) What glass and ice should I use for Jim Beam mixers?
Use a tall highball and lots of fresh ice for long drinks—more ice actually means less dilution and better fizz. Conversely, choose a heavy rocks glass and a single big cube for Old Fashioneds and spirit-forward serves. As a result, your Jim Beam cocktails look polished and taste consistent.