Pregnancy is one of the most beautiful and life-changing experiences you’ll ever have. It’s also a time when your relationship with food takes on a whole new meaning. What you eat now isn’t just fueling you — it’s shaping your baby’s brain, bones, and future health.
And here’s the thing: that old saying “eating for two”? It’s a myth. In reality, your body needs quality over quantity — nutrient-rich foods that meet the unique demands of pregnancy without overloading you with unnecessary calories.
In this guide, we’ll explore the latest science on pregnancy nutrition, reveal the most important nutrients to focus on, and share easy, tasty ways to get them into your daily meals — with plenty of Masala Monk recipes and resources along the way to inspire you.
Why Pregnancy Nutrition Matters More Than Ever
Recent research from the British Nutrition Foundation (2025) revealed something worrying: many expectant mothers — especially teenagers, low-income women, and those carrying more than one baby — aren’t getting enough folate, iron, iodine, or omega-3 fatty acids.
These nutrient gaps can have lifelong effects, from higher risks of neural tube defects to slower brain development and an increased likelihood of chronic diseases later in life. The good news? With thoughtful eating and the right supplements, you can close those gaps and give your baby the best possible start.
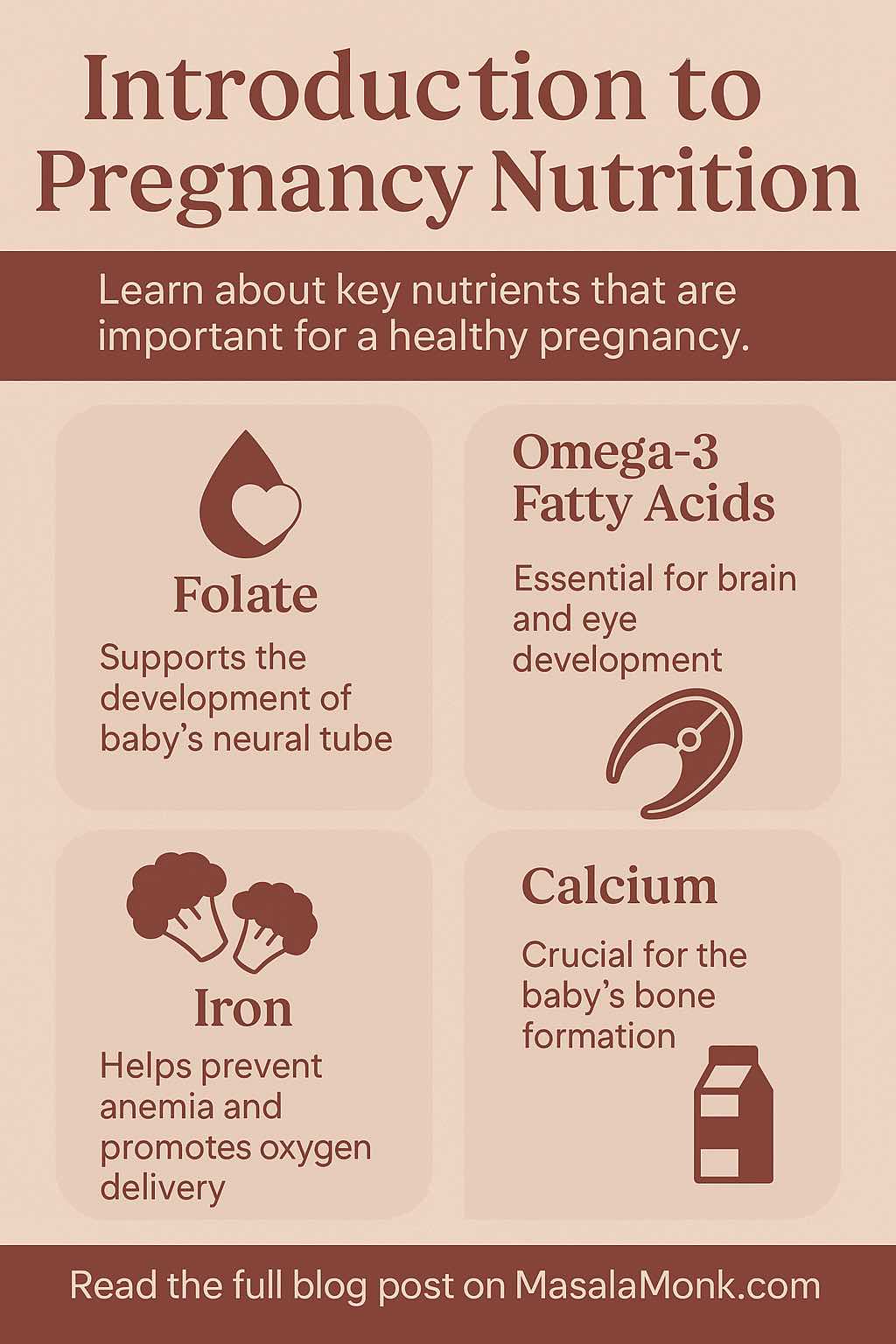
The Pregnancy Nutrition Power List
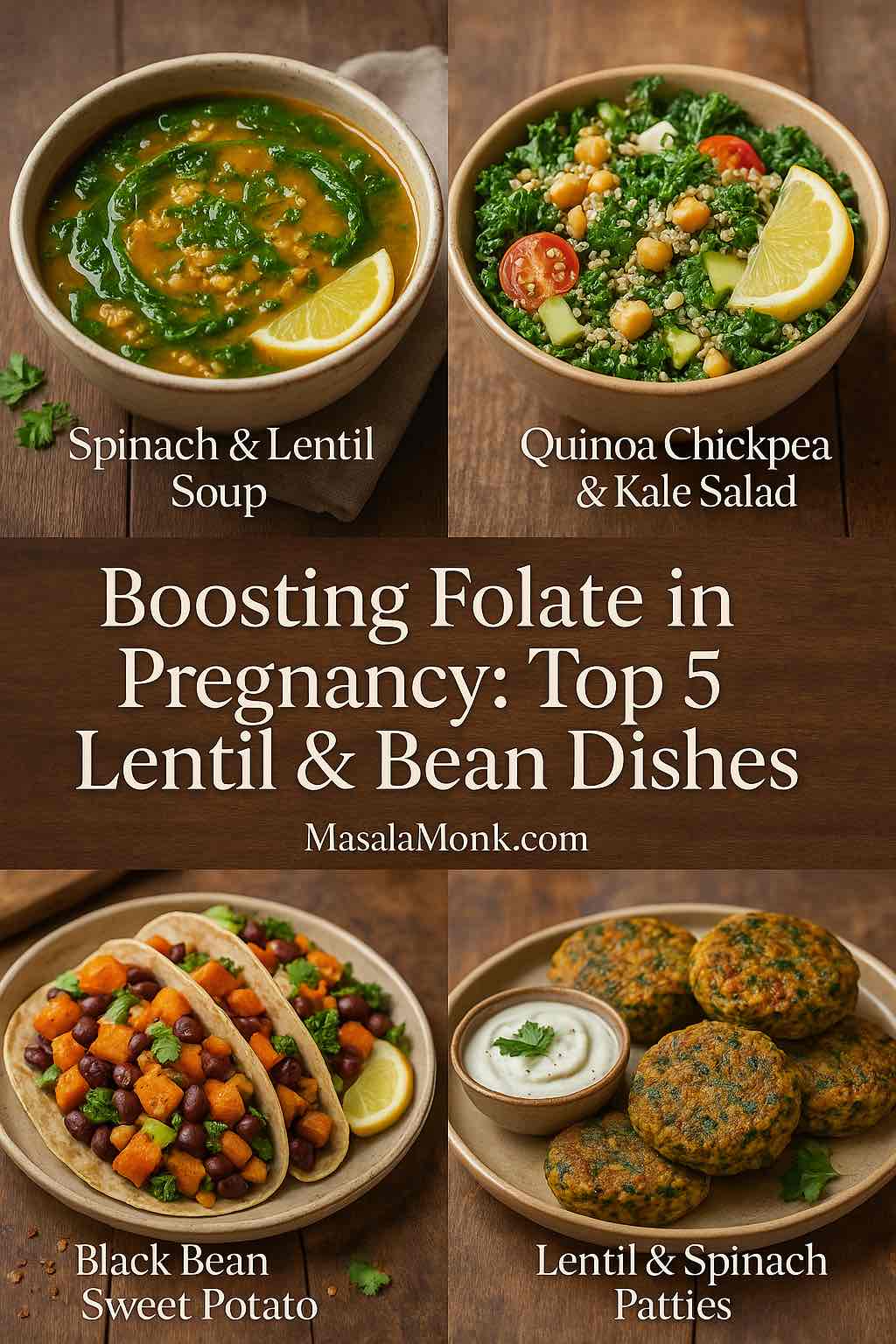
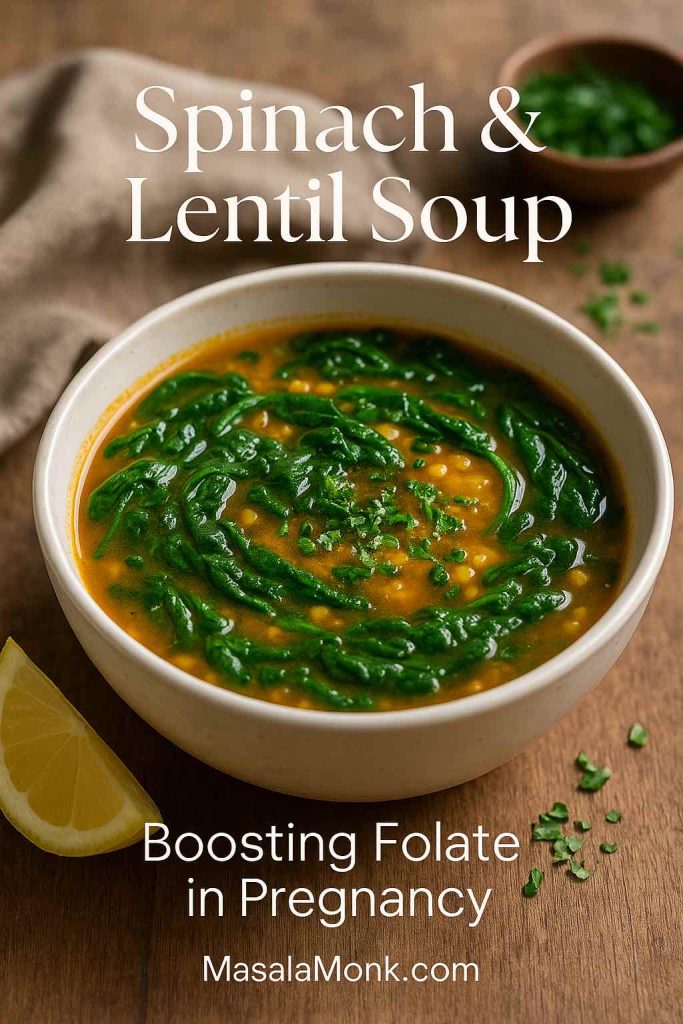
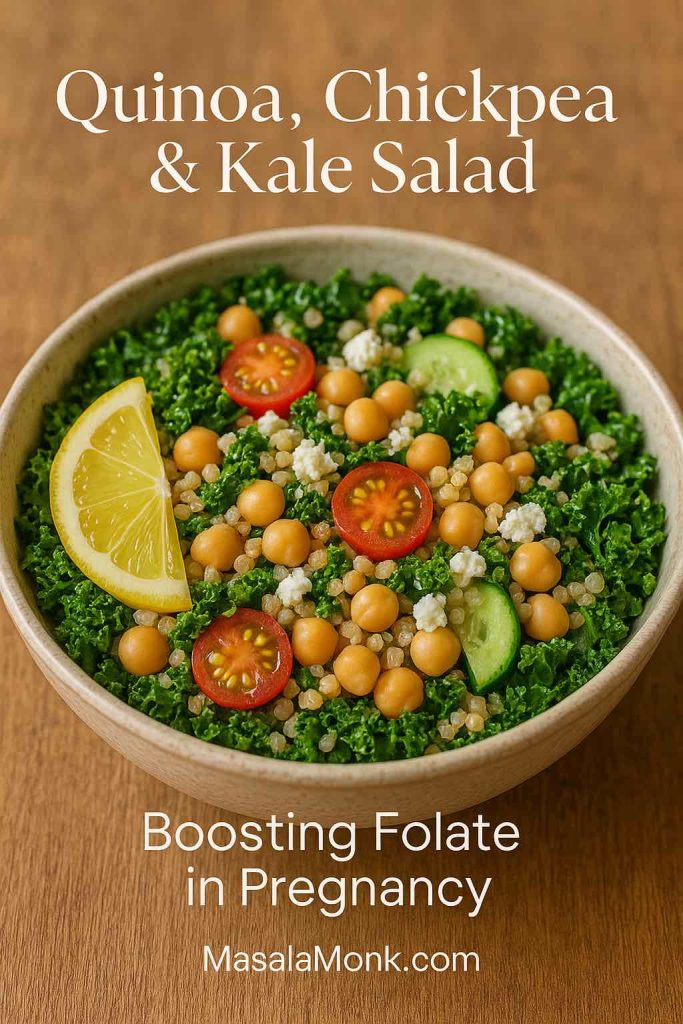
Folate / Folic Acid
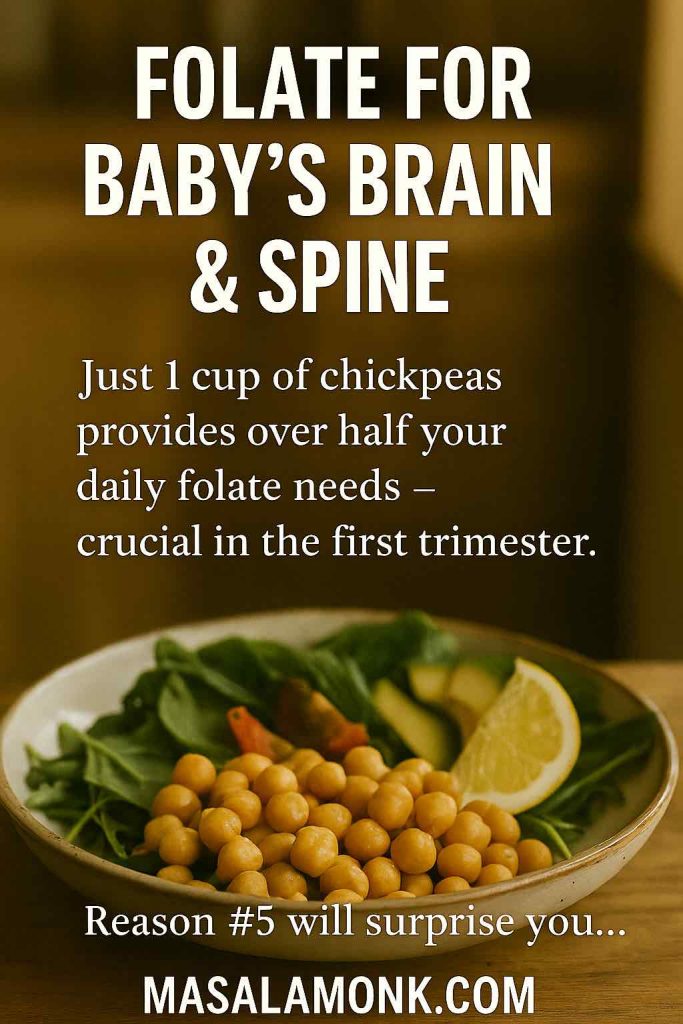
Folate is the star nutrient of early pregnancy, helping prevent neural tube defects and supporting rapid cell growth. Experts recommend starting supplementation before conception if possible — 400 mcg daily pre-pregnancy, increasing to 600 mcg once you’re expecting.
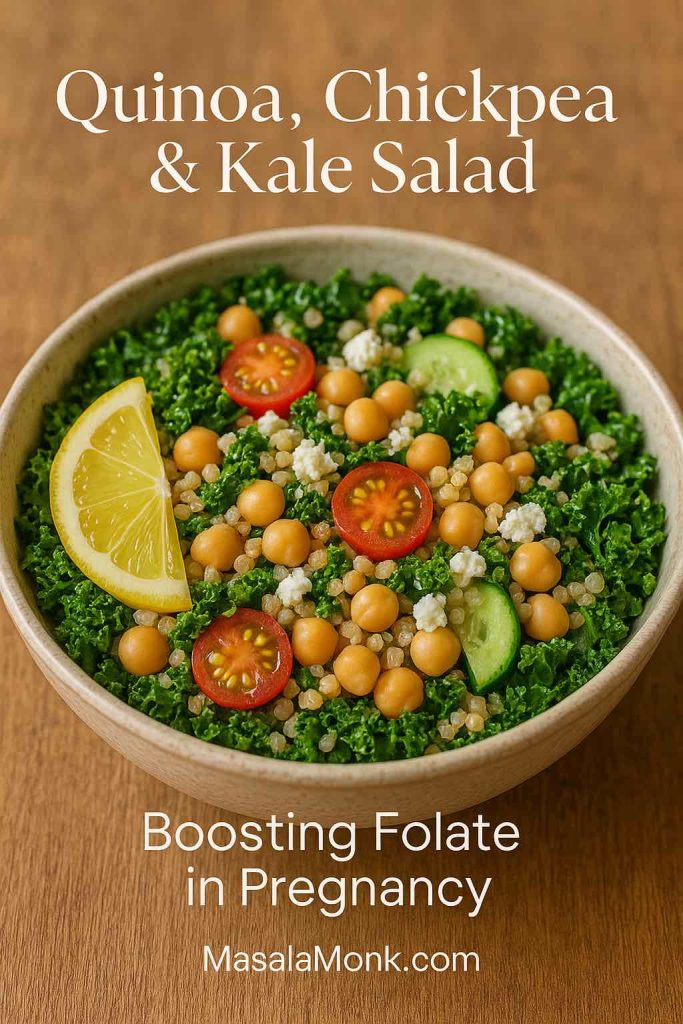
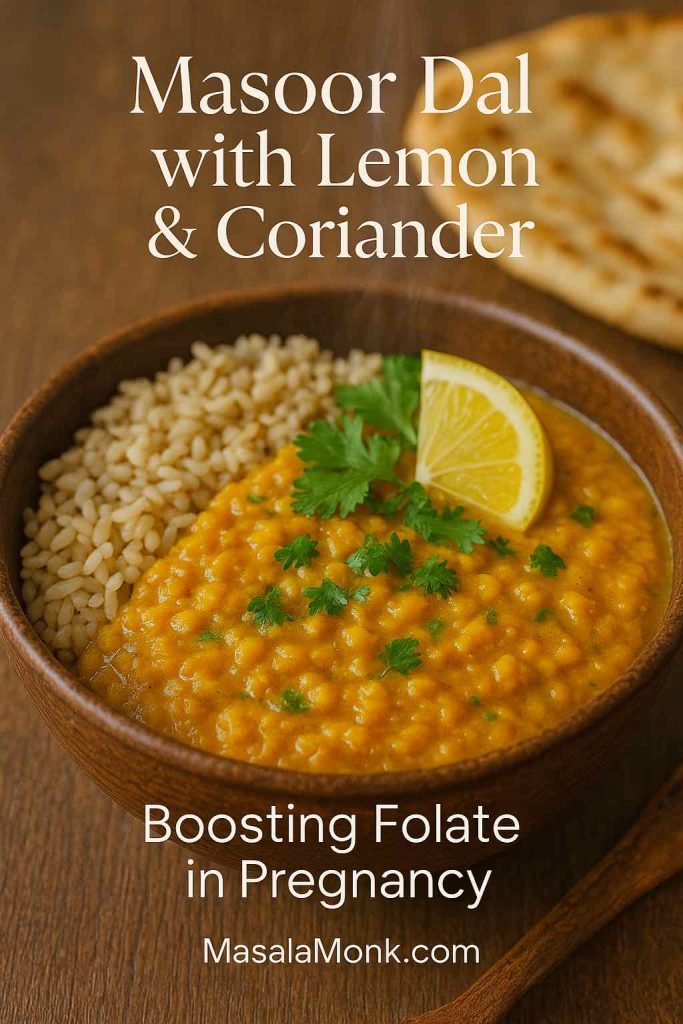
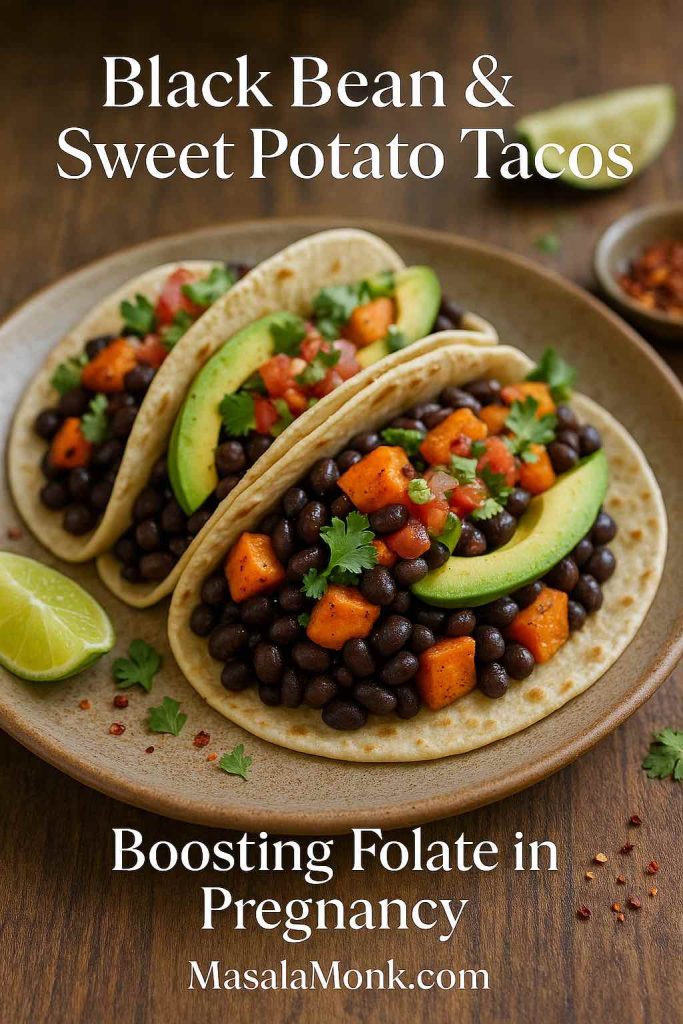
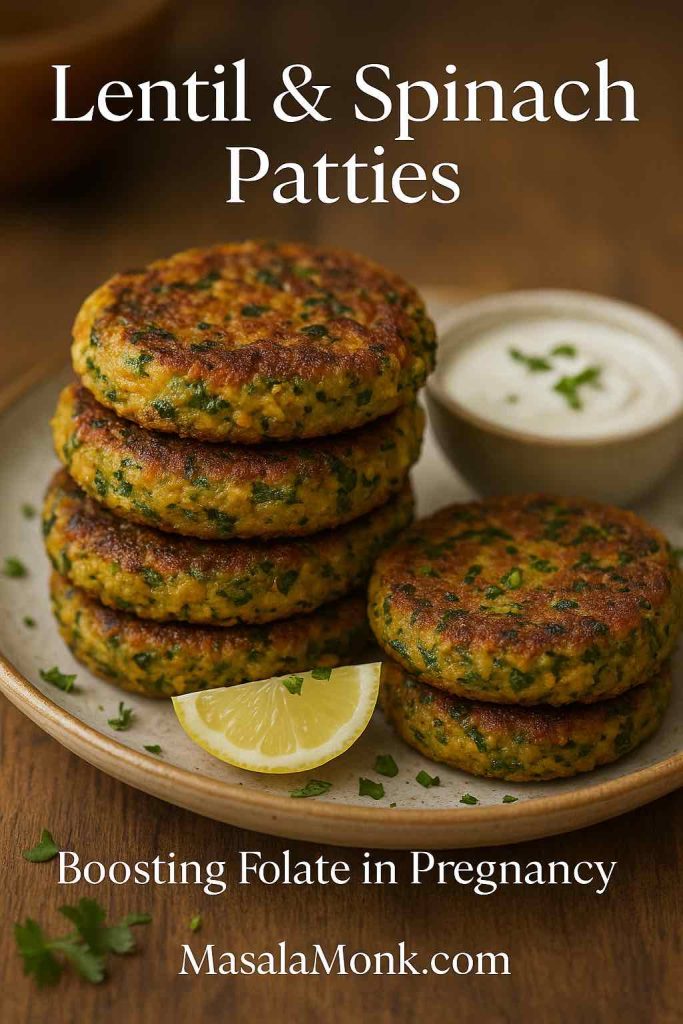
You’ll find it in leafy greens, lentils, beets, and citrus fruits. To make it delicious, try one of our folate-rich salads with kale, quinoa, and beets, or explore these lentil and bean dishes designed to boost folate in pregnancy.
Iron
Pregnancy increases your blood volume by almost 50%, so your need for iron skyrockets. Without enough, you risk iron-deficiency anemia — which can leave you feeling drained and affect your baby’s oxygen supply.
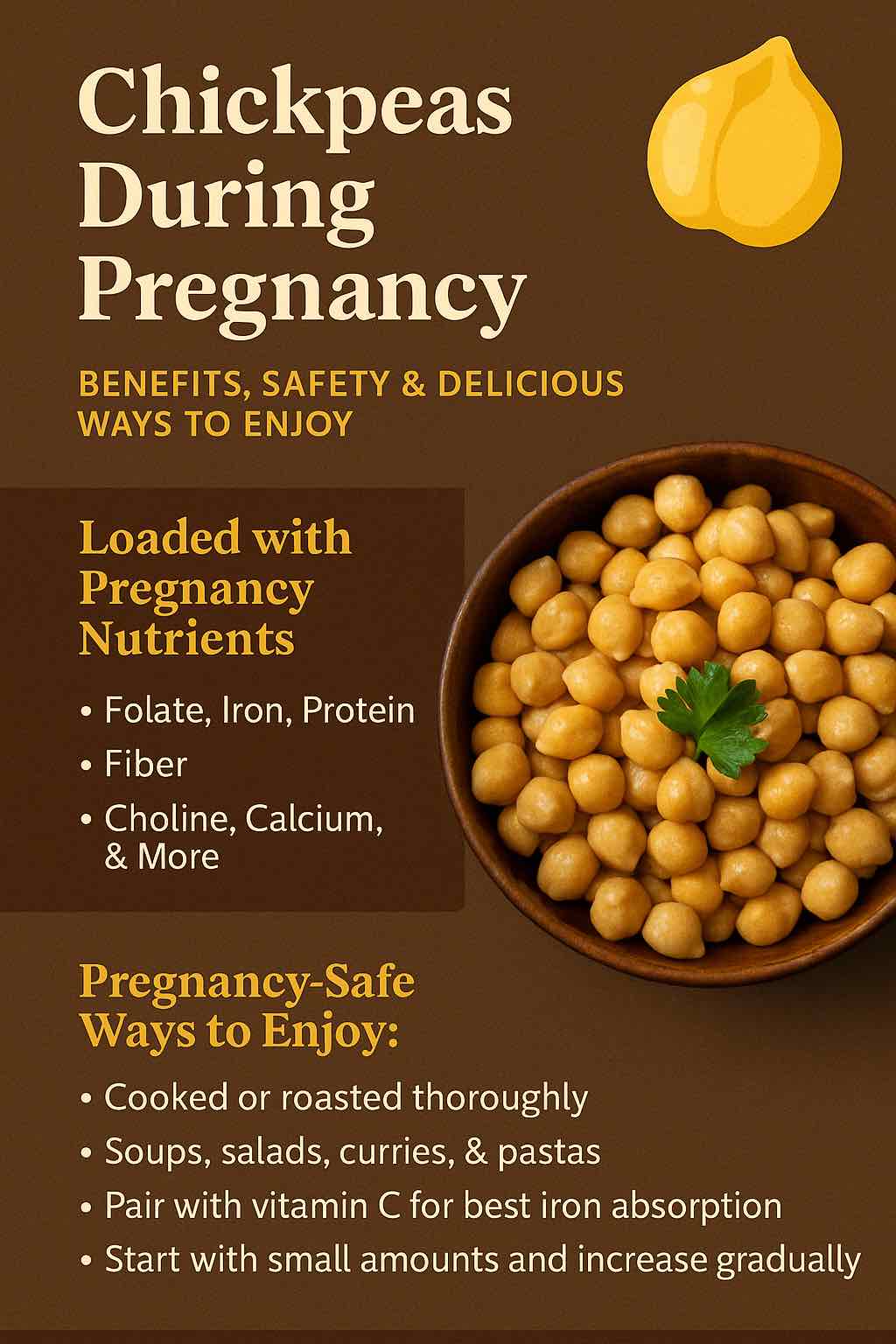
Aim for 27 mg/day through foods like spinach, chickpeas, lean meats, and fortified cereals. Pair iron-rich foods with vitamin C sources (like citrus or tomatoes) for better absorption. For something quick and satisfying, blend up one of our iron-enriched smoothies with spinach and apple.
Calcium & Vitamin D
While your baby’s bones are forming, your body will draw calcium from your own stores if you’re not getting enough — putting you at risk of bone loss.
Calcium needs hover around 1,000 mg/day, with vitamin D helping your body absorb it efficiently. Dairy products, fortified plant milks, almonds, leafy greens, and small fish with bones are all great options. If you want a plant-based boost, check out our guide to millets in pregnancy — they’re rich in calcium, magnesium, and other essential minerals.
Iodine
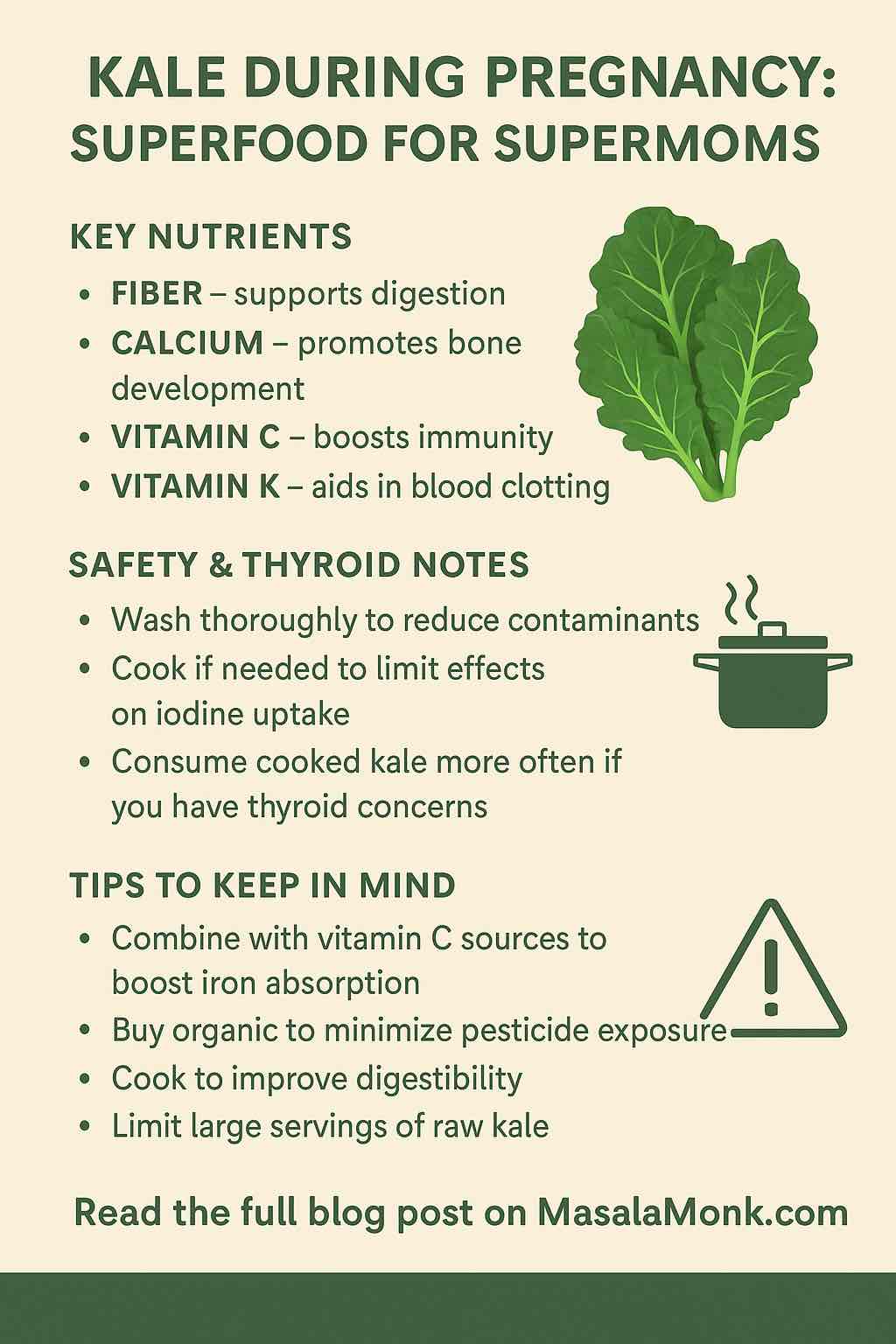
This often-overlooked mineral is essential for thyroid function and fetal brain development. You can get iodine from dairy, eggs, seaweed (in moderation), and seafood — but many women still need a supplement. Check your prenatal label to be sure it’s included.
Might also want to read: Kale During Pregnancy: Superfood for Supermoms
Omega-3 Fatty Acids (DHA & EPA)
Omega-3s are critical for your baby’s brain, eye, and nervous system development. They also reduce the risk of preterm birth and may lower your chances of postpartum depression.
If you eat fish, aim for 2–3 servings of low-mercury varieties per week (think salmon, sardines, trout). Vegetarian or vegan? Consider an algae-based DHA supplement to ensure you’re covered.
Choline
Choline works hand-in-hand with folate to support brain development and memory. Eggs are one of the richest sources, but it’s also found in meat, soybeans, and some nuts. Many prenatal vitamins don’t have enough, so you might need to get it from your diet.
Also read: Chickpeas Through Pregnancy
Zinc & Selenium
These trace minerals support your immune system and act as antioxidants, protecting both you and your baby from oxidative stress. Nuts, seeds, seafood, and whole grains are excellent sources.
Supplements: Quality Over Quantity
While a healthy diet is the foundation, supplements are your insurance policy. But here’s a wake-up call — recent testing found some prenatal vitamins contain heavy metals like lead, arsenic, and cadmium or don’t deliver the nutrients they claim.
That’s why it’s worth reading labels carefully, choosing third-party tested brands, and understanding what’s inside your prenatal. If you’re unsure about folic acid vs. methylfolate, our guide on methylated prenatal vitamins breaks it down clearly.
Eating Well in Every Trimester
First Trimester
Morning sickness can make eating a challenge, so focus on nutrient-rich, nausea-friendly foods — and don’t skip your folate supplement. Need inspiration? Our first trimester nutrition guide offers practical tips to balance nourishment and comfort.
Second Trimester
Energy levels often rise, making it a great time to focus on calcium, vitamin D, and omega-3 intake. Add an extra 300 healthy calories per day from nutrient-rich snacks like avocado toast or yogurt with fruit.
Third Trimester
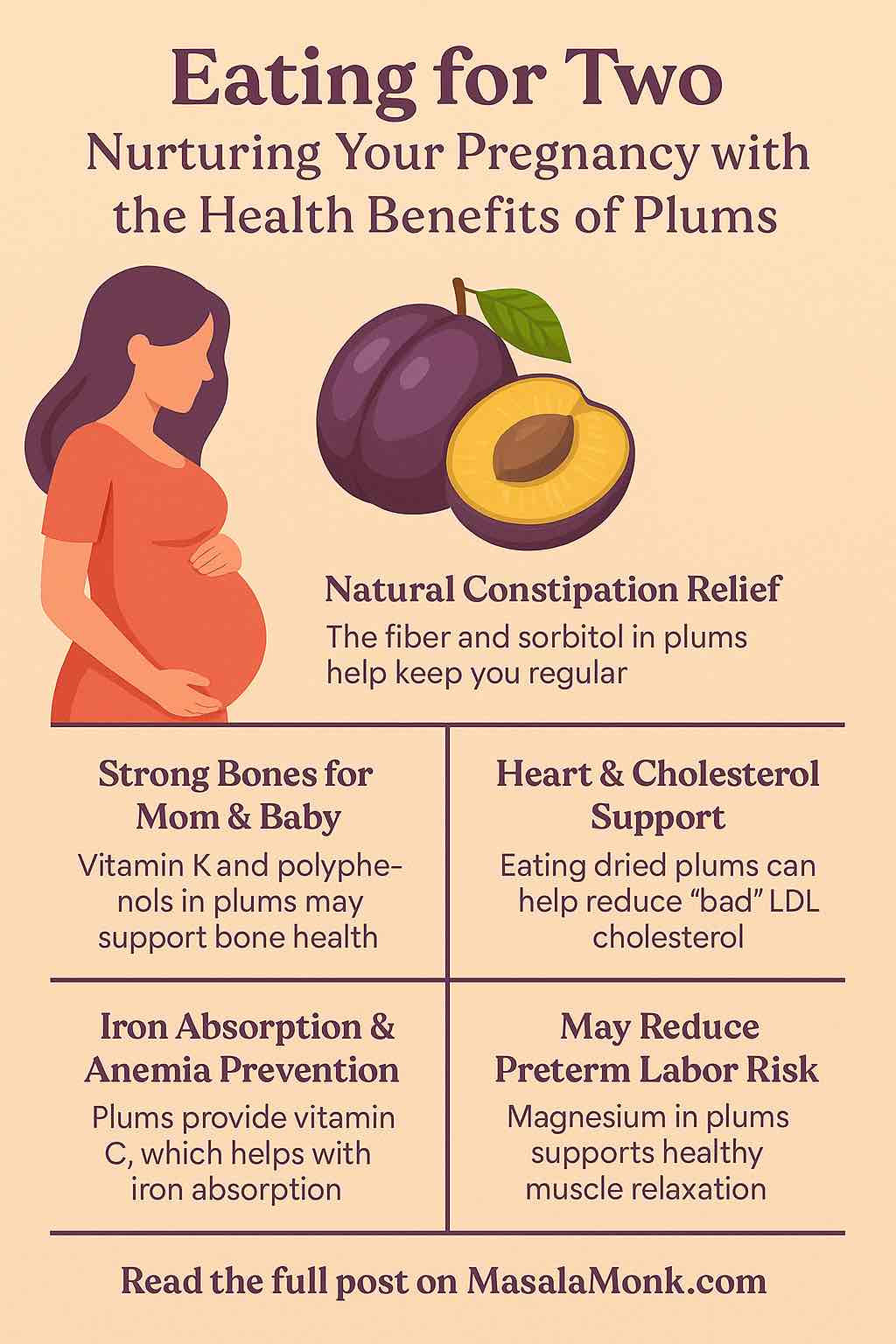
Your baby is growing fast — protein, iron, and fiber are your allies. Keep constipation at bay with plenty of fluids, whole grains, and fresh fruit. If you need help choosing safe, hydrating produce, see our guide to fruits during pregnancy.
The Bottom Line
Pregnancy nutrition isn’t about rigid rules — it’s about making small, intentional choices that nourish you and your baby every single day.
With a plate full of colorful fruits, leafy greens, whole grains, quality proteins, and healthy fats — plus smart supplementation — you’re giving your little one the strongest possible start in life.
And remember, every bite counts. Let food be your ally, not your stress. With a little planning and the right resources, you’ll be confident, well-nourished, and ready for the beautiful journey ahead.
FAQs: Introduction to Pregnancy Nutrition
1. How many extra calories should I eat during pregnancy?
In most cases, you only need about 300 extra healthy calories per day in the second and third trimesters. The first trimester usually doesn’t require extra calories—focus on nutrient density instead.
2. Why is folic acid so important in early pregnancy?
Folic acid (or folate) helps prevent neural tube defects in the baby’s brain and spine. It’s most critical during the first trimester and ideally should be started before conception.
3. Can I get all the nutrients I need from food alone?
A balanced diet is essential, but many women still need prenatal vitamins to meet requirements for folate, iron, iodine, vitamin D, and omega-3s.
4. What’s the difference between folic acid and methylfolate?
Folic acid is a synthetic form of folate. Methylfolate is a bioactive form your body can use directly, especially important for those with MTHFR gene variants.
5. How can I prevent iron-deficiency anemia during pregnancy?
Eat iron-rich foods like spinach, lentils, and lean meats, pair them with vitamin C foods, and consider supplements if your doctor recommends them.
6. Should I take an omega-3 supplement if I don’t eat fish?
Yes. DHA and EPA are critical for fetal brain and eye development. Plant-based sources like flax and chia provide ALA, but you may need an algae-based DHA supplement.
7. How much calcium do I need daily?
Aim for around 1,000 mg/day during pregnancy from a mix of dairy, fortified plant milks, leafy greens, almonds, and other calcium-rich foods.
8. Why is choline often overlooked in pregnancy nutrition?
Choline supports brain development and cell structure, but many prenatal vitamins don’t have enough. Eggs, lean meat, and legumes are good sources.
9. Are all prenatal vitamins safe?
Not necessarily. Some have been found to contain heavy metals or inaccurate nutrient levels. Always choose third-party tested brands and check labels for key nutrients.
10. How can I manage nausea while still eating well?
Opt for smaller, frequent meals, bland foods, ginger, and hydration. Avoid skipping meals—try nutrient-rich snacks like smoothies, nuts, or yogurt.