Tooth pain doesn’t wait for a good time. Coffee turns harsh, ice water stings, and your jaw starts pulsing with every heartbeat. In moments like these, you want relief that is fast, simple, and safe. That’s why clove oil for toothache has stuck around for generations. Used correctly, it can gently numb a hot spot and turn a brutal evening into one you can manage—long enough to arrange the treatment that actually solves the problem.
However, relief is not repair. Eugenol—the main active in clove bud essential oil—can calm irritated tissues and blunt pain signals, yet it cannot remove decay, seal a crack, or drain an abscess. This guide gives you the exact way to use clove oil without hurting your mouth, shows what it can and cannot do, and spells out the signs to stop DIY and book care. You’ll also see real dental science—explained in plain language—so you can act with confidence rather than guesswork.
If you prefer a quick refresher to keep on your phone, here’s a single internal resource you can save now: step-by-step clove oil application (safe dilution + dabbing). Then come back and dive into the details.
⚠️ For education only—not medical advice. Always consult a dentist for diagnosis and treatment.

Why Clove Oil Helps (and why it’s a bridge, not a cure)
Let’s begin with what’s established in dentistry. For decades, clinicians have used zinc-oxide eugenol in short-term, sedative materials because low concentrations of eugenol show anti-inflammatory and local anesthetic effects on the dental pulp. That’s not folk wisdom; it’s documented in classic dental literature on zinc-oxide eugenol’s sedative effect on the pulp. At gentle doses, sore tissues settle; at excessive doses or prolonged exposure, tissues can be irritated—so strength and contact time matter.
Next, move from materials to real patients. In urgent dentistry, there’s modern, human data: a randomized clinical trial in emergency care found that a eugenol pulp dressing delivered meaningful short-term pain reduction after pulpotomy. The full paper is open access—see the randomized clinical trial of eugenol pulp dressing for emergency pulpotomy pain. Although a pulpotomy dressing is a clinic procedure (not a home trick), the take-home is clear: eugenol can provide genuine analgesia in dental contexts.
Meanwhile, bench science helps the experience make sense. A recent review summarizes the antibacterial and antibiofilm actions of clove oil and eugenol against mouth-relevant microbes and biofilms. That doesn’t make clove oil a daily mouthwash, but it does explain why a precisely placed dab can feel “cleaner” along a sore margin.
Even so, here’s the crucial contrast: clove oil turns down signals; dental treatment removes sources. It won’t close a cavity, bond a fracture, or evacuate pus. Therefore, use clove oil as first aid—a humane bridge that buys you time without pretending to be the cure.
Exactly How to Use Clove Oil for Toothache (very dilute, very local, very short-term)
You’ll need
- Clove bud essential oil (check the label; “bud” is the standard profile)
- A carrier oil (coconut or olive oil work well)
- Cotton swabs or a tiny cotton pellet
- A teaspoon and a clean surface
Dilution that respects your mouth
Aim for ~0.5%. In kitchen terms, that’s 1 drop of clove bud oil in ~10 ml (2 teaspoons) of carrier oil. This ceiling helps you numb without burning or sensitizing oral tissues. Stronger is not kinder; it’s just riskier.
Also Read: Guide to Oil Pulling for Dental Health.
Step-by-step How to Use Clove Oil for Toothache
- Rinse first. Use a warm salt-water rinse to reduce irritation and clear debris. Then floss gently around the sore area—trapped food is a common driver of “mystery pain.”
- Mix a tiny batch. In a clean spoon or dish, blend 1 drop clove bud oil with 2 tsp (10 ml) carrier oil. Stir.
- Spot-apply only. Dip a cotton swab and dab just the sore spot—the tender gum margin or the exposed area that winces with air. Do not swish oils; do not paint large areas of soft tissue.
- Wait 5–10 minutes. Mild numbness typically builds within minutes. Spit any excess.
- Repeat sparingly. If needed, reapply every 2–3 hours for a day or two. If you still need this after 48 hours, book care—the pain is telling you something a dab can’t fix.
Safety that isn’t optional
- Do not swallow clove oil, and do not use it intra-orally in children. The NIH monograph documents that while therapeutic topical use hasn’t been linked to liver injury, ingestions can cause severe, acute liver damage—especially in kids. Read the Eugenol (Clove Oil) – LiverTox safety overview for context. A published case even reports fulminant hepatic failure after ~10 ml clove-oil ingestion in a toddler—sobering proof that “natural” isn’t risk-free; see pediatric hepatic failure after clove-oil ingestion (~10 mL).
- Never use neat (undiluted). Oral mucosa is delicate. High-strength oils burn and can sensitize tissues—making the next exposure worse.
- Don’t make it a routine. Repeated, frequent use raises irritation risk and delays the treatment that ends the problem.
⚠️ For education only—not medical advice. Always consult a dentist for diagnosis and treatment.
Clove Oil for Gums vs. Tooth-Deep Pain (choose the right tactic)
Because “toothache” often starts at the edges, it helps to split gum-led soreness from tooth-deep pain.
- If tenderness sits on the gumline—after rough flossing, a popcorn husk, or a retainer rub—start with the basics (salt-water rinse, cleaning the area), then consider a very dilute, spot-only dab for comfort.
- If the ache is inside the tooth—a deep throb, pain on biting, or a hot/cold zing—clove oil can soften the surface misery, but the source is likely pulp irritation, a crack, or a brewing infection. In that case, use the spot dab as a bridge and book care.
If you want one broader read about the spice beyond pain relief—benefits, caveats, and culture—take a single pass through benefits of clove for teeth and gums and then come back to the plan that actually gets you sleeping again.
Clove Oil for Cavities, Cracks, and Sensitivity: Relief vs. Repair
Let’s stay practical. Cavities are a structural and bacterial process; cracks are mechanical failures; sensitivity is often exposed dentin with open tubules. Therefore, clove oil can numb and calm surface irritation, but it cannot rebuild enamel, seal a fracture, or stop bacterial progression.
Consequently, if cold air zings a tooth, a ≤0.5% dab can settle the surface for a while. But if biting on a seed sends lightning down a cusp—or if a visible hole catches food—the relief will be brief because the cause remains. Meanwhile, protect the tooth: chew on the other side, skip ultra-hot or icy drinks, and call a dentist. The earlier you address a crack or deep decay, the simpler the fix tends to be.
For a single, practical read on reactions and limits so you don’t overdo it, bookmark side effects and precautions for cloves/clove oil.
Clove Oil for Tooth Infection and Dental Abscess (why source control matters)
When infection builds under a tooth or in the surrounding gum, pressure and pus don’t care about numbing balms. A careful dab may buy you a calmer hour, yet the relief collapses because the source is still there. Primary-care advice is consistent: first, manage pain; then drainage or definitive treatment by a dentist; and importantly, repeated antibiotics without drainage are inappropriate. If you want a clear, patient-facing summary you can trust, read dental abscess primary-care guidance (NHS Inform)—it explains exactly why home remedies cannot end the cycle when pus is involved.
In short, clove oil is a bridge here too—useful while you organize care—but source control is what stops the pain from coming back.
Also Read: Coconut Oil for Oral Health.
⚠️ For education only—not medical advice. Always consult a dentist for diagnosis and treatment.
After Extraction (and Dry Socket): Please Don’t DIY Pack With Oils
If your pain peaks on days 2–3 after an extraction, a dry socket (alveolar osteitis) may be to blame. At that point, the right move is back to the chair, not a cotton pellet soaked in your spice cabinet. In clinic, a dentist may place a medicated dressing; some materials include eugenol, others don’t, and choices vary by presentation and preference. For a balanced snapshot of what’s used and how strong the evidence is, read the Cochrane review of local interventions for dry socket. The headline for you is simple: sockets are wounds, and evidence comparing materials is low-certainty—so let a clinician examine and treat; no home packing.
What Clove Oil Can Do Around Oral Microbes (adjunct, not a substitute)
Many people report that a careful dab “feels cleaner.” Mechanistically, that makes sense. A recent review brings together evidence on the antibacterial and antibiofilm actions of clove oil and eugenol, including effects on oral-relevant microorganisms and biofilm structures. Even so, that is a supporting act. It may explain a fresher feel at a sore margin after a precise application, but it does not replace brushing with fluoride, interdental cleaning, or professional care.
If you’re tempted to build a daily clove mouthwash from this, don’t. Essential oils are potent; the mouth is delicate. Keep clove oil for acute, spot-only relief, and keep your daily rinse simple: warm salt water.
Variants of Clove (and what’s reasonable)
Clove Oil for Gums (surface tenderness)
For gumline soreness after a scratch or rough floss, a ≤0.5% spot dab can help after a salt-water rinse and gentle cleaning. If the same area bleeds or puffs up often, clove oil won’t fix the pattern—book a cleaning and a gum check.
Clove Powder for Toothache (kitchen-friendly, but too rough)
Clove powder feels familiar, but it’s abrasive and potent on inflamed mucosa. If you try anything powder-based, blend a pinch into 1 teaspoon of carrier oil and dab briefly—never pack dry powder into a cavity or under the gum. If tissue turns white or stings persistently, rinse and stop.
Clove Mouthwash or “Clove Water” (keep it ultra-dilute and occasional)
For daily rinsing, stick to warm salt water. If you occasionally add a clove touch, keep it ultra-dilute and always spit. Essential-oil rinses are not for children, and frequent use increases the chance of irritation or sensitization.
Whole Cloves for Toothache (brief, if at all)
Chewing a whole clove releases eugenol, but it also drags a rough bud over tender tissue. If you do this at all, keep contact very brief, then switch back to the precise, diluted spot method—it’s more controllable and kinder to the mouth. If breath freshness is your main goal, take one careful read of chewing cloves: pros and cons and decide if it’s worth it for you.
Laung/Lavang Oil for Toothache (same oil, different name)
Different names—laung or lavang—same ingredient: clove bud essential oil. So the same rules apply: very dilute, very local, very short-term; never in children’s mouths.
⚠️ For education only—not medical advice. Always consult a dentist for diagnosis and treatment.
Safety That’s Worth Your Time (even when you’re hurting)
Because clove oil is powerful, guardrails matter:
- Dose and dilution matter. Stay at or below ~0.5% (≈ 1 drop in 10 ml / 2 tsp carrier). Higher concentrations buy risk, not more relief.
- Location matters. Spot-apply the exact sore area; do not swish essential oils in your mouth.
- Time matters. Use it short-term while you arrange care. If pain persists, that’s information—get a diagnosis.
- Children are off-limits. Intra-oral clove oil and kids don’t mix. The Eugenol (Clove Oil) – LiverTox safety overview explains why ingestions are dangerous, and the pediatric hepatic failure case illustrates how little volume it can take.
- Your medical context matters. If you’re pregnant, on anticoagulants, have a bleeding or liver disorder, or manage complex conditions, prefer non-oil measures (salt water, cold compress, appropriate analgesics) and prioritize a clinician visit.
- Don’t make clove a daily mouthwash. It’s a remedy, not a routine. Repeated exposure raises the odds of irritation and sensitization.
For a deeper look at possible reactions and common sense limits, you can skim this once and keep life simple: side effects and precautions for cloves.
A Pain Plan You Can Follow While You Arrange Care
1) Rinse, then protect.
Warm salt-water rinse; gentle floss to clear the culprit; avoid chewing on the sore side. Small habits pay big dividends. If you want “get me through the next hour” tactics, peek at one-minute toothache easers once, then come back.
2) Use clove oil for toothache as a precise bridge.
Mix the ≤0.5% blend, dab only the sore spot, wait 5–10 minutes, and repeat every 2–3 hours if needed for up to two days.
3) Add analgesics that actually work.
If they’re suitable for you, NSAIDs (ibuprofen/naproxen), alone or combined with acetaminophen, are first-line for acute dental pain; for dosing logic and cautions, see the ADA overview of oral analgesics for acute dental pain. Follow labels and any clinician direction.
4) Book the dentist, then keep nudging.
Ask for cancellations and urgent slots; be specific about symptoms (swelling, fever, night pain). For infection-type stories, remember: drainage/source control by a dentist ends the cycle—not another loop of home remedies. For clarity, read dental abscess primary-care guidance (NHS Inform).
5) Make the night survivable.
Avoid very hot or cold drinks, go easy on alcohol, and sleep slightly elevated to reduce pulsing. Stack small advantages and the night gets easier.
Also Read: Peppermint Oil and Dental Health
Aftercare and “Dry Socket” Revisited (because it’s a common curveball)
Two dots to connect. First, post-extraction discomfort should ease steadily after day one. Second, when pain intensifies on days two or three, dry socket climbs the list. In that scenario, oils and home dressings are a detour. The best next step is an in-person socket check and, if appropriate, a medicated dressing placed by a clinician. For a wide-angle view of what’s used and why choices vary, the Cochrane review of local interventions for dry socket is your neutral explainer. It’s precisely why “clinic, not kitchen” is the rule.
⚠️ For education only—not medical advice. Always consult a dentist for diagnosis and treatment.
Where the Science and Real Life Meet (confidence, not anxiety)
- Pulp biology makes the numb sensible. Low-dose eugenol shows anti-inflammatory and local anesthetic effects on dental pulp; this underpins its use in zinc-oxide eugenol sedative materials and explains why a tiny, diluted dab can make a sore margin feel quieter (see the paper on zinc-oxide eugenol’s sedative effect on the pulp).
- Clinical relief in the chair is real. In emergency pulpotomy, a eugenol pulp dressing delivered short-term pain relief in a randomized trial—confirming we’re not imagining eugenol’s effect (see the randomized clinical trial of eugenol pulp dressing for emergency pulpotomy pain).
- Microbes and biofilms respond in vitro. Modern reviews show antibacterial and antibiofilm actions of clove oil/eugenol relevant to oral biofilms. That supports an adjunct role for a careful dab; it does not replace hygiene or care (see antibacterial and antibiofilm actions of clove oil and eugenol).
- Dry socket is not a DIY project. Comparing socket dressings shows low-certainty evidence overall; clinical judgment rules (see the Cochrane review of local interventions for dry socket).
- Safety isn’t optional. The Eugenol – LiverTox monograph and a pediatric hepatic failure case explain why swallowing oils—especially in children—is dangerous.
- Pain control has a playbook. For what actually works while you wait for care, the ADA overview of oral analgesics for acute dental pain is the north star.
When to Stop DIY and Go Now
Please switch from home care to a dentist promptly if you notice any of the following:
- Pain lasting more than 48 hours despite sensible self-care
- Swelling, a bad taste, fever, or pain that wakes you at night
- Pain on biting, a broken tooth, or pain after trauma
- Post-extraction pain that worsens on days 2–3 (possible dry socket)
- Any difficulty breathing, swallowing, or opening your mouth fully (urgent)
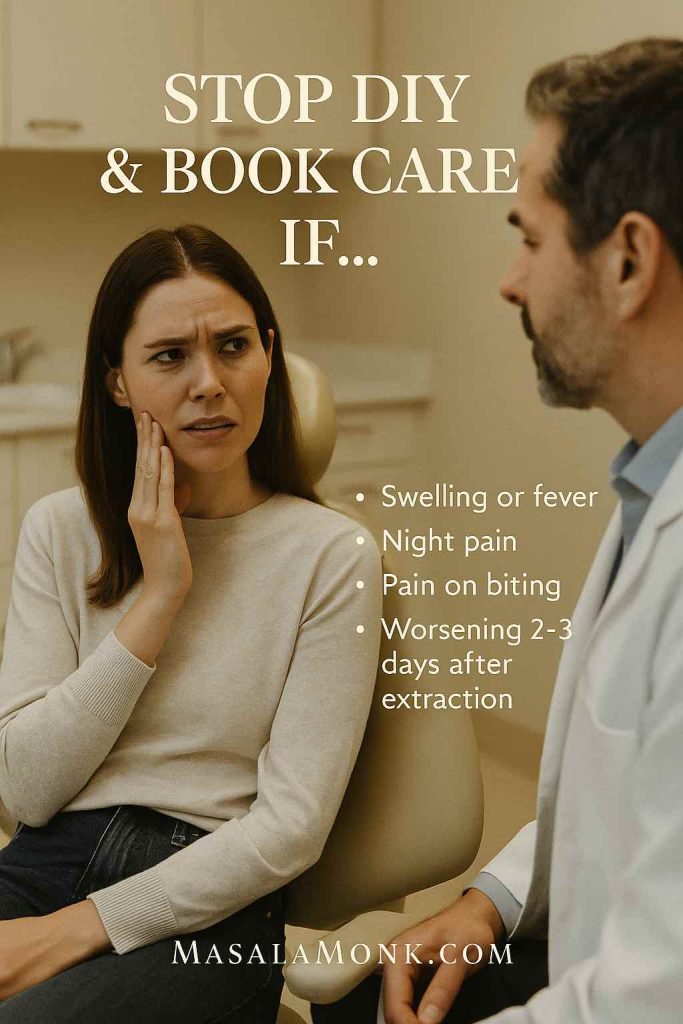
These are the moments when clove oil becomes a distraction. Get examined. If the story sounds like an abscess, remember the primary-care rule you already saw: drainage/source control ends the cycle.
⚠️ For education only—not medical advice. Always consult a dentist for diagnosis and treatment.
Bring It All Together
- Yes, clove oil for toothache can quiet a throbbing tooth—especially at the gum margin—when you use it very dilute, very local, and very short-term.
- No, it doesn’t fix cavities, seal cracks, or drain infections—those need a dentist.
- Meanwhile, pair a careful ≤0.5% spot dab with salt-water rinses and evidence-based analgesics from the ADA overview of oral analgesics for acute dental pain to keep the night humane.
- If pain persists beyond 48 hours, or you see red flags (swelling, fever, night pain), book care now. For infection-type stories, follow dental abscess primary-care guidance (NHS Inform): drainage/source control ends the cycle.
- After extraction, don’t pack sockets at home; let the clinic examine and treat, as the Cochrane review of local interventions for dry socket makes clear.
If you’re reading this mid-throb, breathe. Mix the tiny batch. Dab the exact spot. Give it a few quiet minutes. Then call the clinic and ask for the earliest slot. Relief now, treatment next—that’s how you get your bite, your sleep, and your day back.
Also Read: 5 Natural Spices Used in Ayurveda for Dental Health, Teeth, and Oral Wellness
External sources used in this post
- zinc-oxide eugenol’s sedative effect on the pulp — Oral Surg Oral Med Oral Pathol review PDF: https://www.oooojournal.net/article/0030-4220(92)90020-Q/pdf
- randomized clinical trial of eugenol pulp dressing for emergency pulpotomy pain — open access: https://pmc.ncbi.nlm.nih.gov/articles/PMC10377881/
- antibacterial and antibiofilm actions of clove oil and eugenol — review: https://www.sciencedirect.com/science/article/pii/S0023643822011847
- Cochrane review of local interventions for dry socket: https://pmc.ncbi.nlm.nih.gov/articles/PMC9511819/
- Eugenol (Clove Oil) – LiverTox safety overview: https://www.ncbi.nlm.nih.gov/books/NBK551727/
- pediatric hepatic failure after clove-oil ingestion (~10 mL): https://pubmed.ncbi.nlm.nih.gov/15895251/
- dental abscess primary-care guidance (NHS Inform): https://www.nhsinform.scot/illnesses-and-conditions/mouth/dental-abscess/
- ADA overview of oral analgesics for acute dental pain: https://www.ada.org/resources/ada-library/oral-health-topics/oral-analgesics-for-acute-dental-pain
⚠️ For education only—not medical advice. Always consult a dentist for diagnosis and treatment.
FAQs
) What is Clove Oil for Toothache and how does it actually help?
Clove Oil for Toothache is typically clove bud essential oil diluted in a carrier oil and dabbed on the sore spot. Thanks to eugenol, it can dull pain signals and calm irritated tissues. However, it eases symptoms for a short time; it doesn’t fix cavities, cracks, or infections.
2) How do I dilute Clove Oil for Toothache correctly?
For practical safety, keep it very weak: about one drop of clove bud oil mixed into roughly two teaspoons of carrier oil. Then, apply only to the exact sore area with a cotton swab. This way, you get comfort without burning delicate oral tissues.
3) How often can I apply it during the day?
Use sparingly—generally every two to three hours, and only for a day or two. If you’re still relying on it after 48 hours, the underlying problem likely needs professional treatment, so move from DIY to a dental visit.
4) Can I put Clove Oil for Toothache directly on the tooth, undiluted?
No. Undiluted essential oils are too strong for the mouth. Instead, dilute first and dab precisely. This approach is gentler, more controllable, and, importantly, safer for your gums and inner cheeks.
5) Does Clove Oil for Toothache work for gum soreness as well?
Yes—sometimes. After you rinse with warm salt water and remove any trapped debris, a carefully diluted, spot-only dab can soothe minor gum irritation. Even so, repeated bleeding, swelling, or tenderness points to a gum issue that needs a cleaning and a check-up.
6) Will Clove Oil for Toothache treat cavities or infections?
Unfortunately, no. It can take the edge off while you arrange care, but it won’t rebuild enamel, seal a fracture, or drain pus. Consequently, use it as a bridge to proper treatment rather than a substitute for it.
7) Is Clove Oil for Toothache safe for everyone?
Not quite. Children should not have clove oil used inside the mouth, and no one should swallow it. Furthermore, if you are pregnant, on blood thinners, or have liver or bleeding disorders, stick to gentle measures like salt water and appropriate pain relief, and seek professional guidance promptly.
8) What’s the best way to apply Clove Oil for Toothache so it actually works?
First, rinse. Next, mix a tiny batch at a low dilution. Then, dip a cotton swab and tap only the sore margin or exposed area—don’t swish, don’t coat large surfaces. Finally, wait five to ten minutes for relief to develop, and spit any excess.
9) Can I use clove powder or a whole clove instead of oil?
Sometimes, but carefully. Clove powder is abrasive, so if you try it, mix a pinch into a little carrier oil and dab briefly. Meanwhile, a whole clove can release eugenol but also scrapes tender tissue; if you try it, keep contact very short and switch back to the precise spot-dab method.
10) What about a clove mouthwash—does that count as Clove Oil for Toothache?
Only as an occasional add-on. If you do it at all, keep it ultra-dilute and always spit. However, daily essential-oil rinsing can irritate oral tissues. For toothache, a tiny, targeted dab is usually more effective and much safer.
11) How can I make the relief from Clove Oil for Toothache last a bit longer?
Begin with basics: warm salt-water rinses, careful flossing to clear the area, and avoiding very hot or very cold drinks. Then, use the diluted spot dab. Additionally, appropriate over-the-counter pain relief (if suitable for you) can help carry you through until you’re seen.
12) When should I stop using Clove Oil for Toothache and see a dentist immediately?
Stop DIY and go now if pain lasts beyond 48 hours, if you notice swelling or fever, if biting hurts sharply, or if pain worsens two to three days after an extraction. Likewise, any trouble breathing, swallowing, or opening your mouth fully is an urgent situation.










