In today’s fast-paced world, stress is unavoidable; however, chronic stress can wreak havoc on health. One of the main reasons is cortisol, the body’s primary stress hormone. Elevated cortisol levels are linked to anxiety, poor sleep, weight gain, and even burnout. Recent research shows a strong connection between fish oil and cortisol balance, with omega-3 fatty acids helping the body regulate stress hormones naturally.
Lifestyle changes such as better sleep, regular exercise, and mindfulness remain important. However, omega-3s from fish oil may offer additional support, acting as a nutritional ally in reducing cortisol and calming stress.
Therefore, in this article, we’ll dive into the science-backed connection between Fish Oil’s omega-3 and cortisol and explore whether fish oil could help calm the storm within.
In case you want to know how to pick a good fish oil supplement, this post has information to help: Best Fish Oil Supplements on Amazon India
🧠 What is Cortisol—and Why Should You Care?
Cortisol is a steroid hormone produced by your adrenal glands. It helps your body respond to stress, regulate metabolism, reduce inflammation, and control blood pressure. But when cortisol levels stay high for too long—due to chronic stress, poor sleep, or underlying health conditions—it can lead to serious problems like:
- Fatigue and brain fog
- Anxiety or irritability
- Weight gain, especially belly fat
- Poor immune function
- Sleep disturbances
- High blood pressure and sugar levels
In short, keeping your cortisol levels balanced is essential for your mental and physical well-being.
How to Lower, Reduce, and Manage Cortisol Levels Naturally
High cortisol doesn’t have to control your life. With the right lifestyle changes and nutrition, you can gradually lower cortisol levels, reduce stress responses, and manage this hormone more effectively. Below are science-backed strategies — plus links to deeper MasalaMonk guides.
🛏️ How to Lower Cortisol with Better Sleep
Quality sleep is the most powerful way to reduce cortisol naturally. Going to bed at the same time, avoiding late-night screens, and building a calming routine help decrease stress hormone levels overnight.
🧘 How to Reduce Cortisol Through Stress-Relief Practices
Simple daily techniques like meditation, yoga, and deep breathing lower high cortisol levels by calming your nervous system. Even 10 minutes a day can help manage stress more effectively.
🥗 Foods That Lower Cortisol Levels Naturally
Nutrition is key in cortisol management. Whole foods, healthy fats, and fiber-rich meals can reduce stress hormones. For a full guide, see Diet Strategies to Lower Cortisol Levels Naturally.
🍫 What Foods Help Reduce Cortisol Quickly?
Certain foods directly support cortisol reduction. Avocados, salmon, chia seeds, dark chocolate, and berries are proven to help decrease cortisol levels. Discover more in 5 Foods That Naturally Decrease Cortisol.
🍵 Teas That Help Lower Cortisol Hormone
Herbal teas like chamomile, tulsi, and lemon balm, along with green tea, naturally reduce cortisol spikes while promoting relaxation. Learn more in Tea and Cortisol: How Your Favorite Brew Can Help Manage Stress.
🐟 Does Fish Oil Help Lower Cortisol?
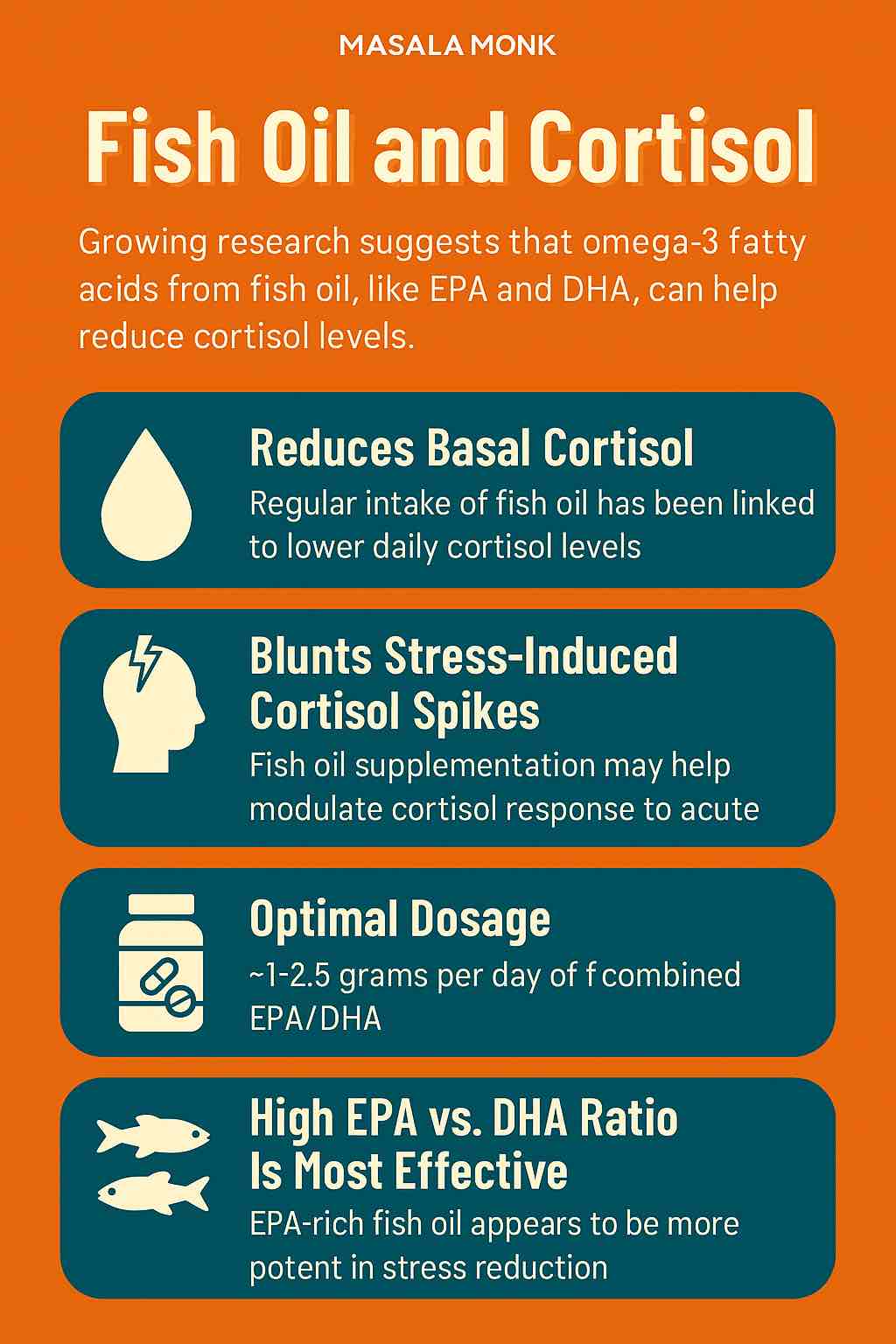
Yes — omega-3 fatty acids (EPA + DHA) from fish oil have been shown to reduce cortisol levels and blunt stress-induced surges. This makes fish oil supplements one of the best nutritional tools for stress resilience.
💧 How to Manage Cortisol with Daily Habits
Staying hydrated, practicing deep breathing, and spending time outdoors all support cortisol management. These small habits add up to significant long-term benefits.
👉 By combining these steps — sleep, stress management, diet, teas, and omega-3s — you create a sustainable way to lower cortisol levels and restore balance naturally.
🐟 Fish Oil: What Makes It Special?
Cortisol is a steroid hormone released by your adrenal glands, and it plays a crucial role in how your body responds to stress. In fact, it is often called the “stress hormone” because it helps regulate metabolism, reduce inflammation, and control blood pressure when your body is under pressure.
However, when cortisol levels remain high for too long—due to chronic stress, lack of sleep, or underlying health conditions—the effects can be harmful. Elevated cortisol can gradually disrupt your body’s balance and lead to:
- Fatigue and brain fog, which affect focus and productivity.
- Anxiety or irritability, making stress feel even worse.
- Weight gain, especially stubborn belly fat.
- Poor immune function, leaving you more vulnerable to illness.
- Sleep disturbances that create a vicious cycle of stress.
- Higher blood pressure and blood sugar levels over time.
Therefore, while cortisol is essential for survival, keeping it balanced is the key to long-term physical and mental well-being. In short, understanding cortisol—and knowing how to lower or manage it—can be life-changing.
Do not miss Best Fish Oil Supplements on Amazon India
🧪 Scientific Evidence: Fish Oil and Cortisol in Human Studies
When it comes to stress and hormones, research matters. Fortunately, several human clinical trials and randomized controlled studies show that fish oil can indeed influence cortisol—the body’s main stress hormone. Let’s look at the findings step by step.
1. Fish Oil Lowers Basal (Resting) Cortisol
Multiple studies demonstrate that consistent omega-3 supplementation may decrease baseline cortisol levels, which are often elevated due to chronic stress:
- Alcohol Recovery Patients: In a 3-week study, men recovering from alcohol addiction who took fish oil (60 mg EPA + 252 mg DHA daily) experienced significantly lower daily cortisol compared to the placebo group.
- Adolescents with Depression: A 12-week trial found that depressed teenagers taking omega-3 supplements showed a clear reduction in morning cortisol levels—indicating better emotional and hormonal balance.
- Healthy Adults: A 6-week trial using 4g/day of high-EPA fish oil showed a trend toward lower cortisol, though not statistically significant. Still, it points toward potential benefits.
- Burned-Out Nurses: Healthcare workers under severe stress saw a marked reduction in the cortisol awakening response (the morning spike) after 8 weeks of fish oil supplementation.
👉 In summary, evidence suggests that fish oil can help regulate daily cortisol rhythms, particularly in stressed or vulnerable populations.
2. Fish Oil Blunts Stress-Induced Cortisol Surges
Even more compelling is research showing that omega-3s blunt cortisol spikes during acute stress—moments when your body overreacts to pressure:
- Social Stress Test (TSST): In a 4-month trial, people taking 2.5 g/day of EPA-rich fish oil had 19% lower cortisol levels during a public-speaking stress test than the placebo group. Even a lower dose (1.25 g/day) showed measurable benefits.
- Pregnant Women: Supplementing with 450 mg/day DHA led to significantly calmer hormonal responses, reducing cortisol reactivity during stressful situations.
👉 These studies highlight how fish oil doesn’t just lower cortisol at rest—it also protects you during stressful moments, keeping your response more balanced and less overwhelming.
✅ Takeaway: Scientific evidence strongly supports that fish oil and omega-3 fatty acids can help lower cortisol, regulate daily rhythms, and reduce stress-related hormonal spikes.
💊 What’s the Ideal Fish Oil Dosage for Cortisol?
Different studies used different doses, but here’s what we know works:
| Goal | Suggested Dose | EPA:DHA Ratio |
|---|---|---|
| Lower daily cortisol | 300–1000 mg EPA+DHA/day | Any ratio |
| Reduce stress reactivity | 1.25g to 2.5g/day EPA+DHA | High EPA (5:1 to 6:1) |
| Improve mood + stress in teens or pregnancy | 400–900 mg/day DHA | Balanced or DHA-rich |
👉 Tip: Look for high-quality fish oil supplements with at least 1 gram of total omega-3s (EPA + DHA). EPA-rich formulas seem especially effective for stress reduction. Read More: Best Fish Oil Supplements on Amazon India
👩⚕️ Who May Benefit the Most?
Fish oil supplements can be useful for almost everyone. However, certain groups may experience even greater benefits due to the role of omega-3s in stress and hormone regulation. For example, fish oil may help if you:
- Struggle with chronic stress or burnout → Omega-3s can support a calmer stress response and reduce cortisol spikes.
- Have anxiety or mood issues → Regular intake may improve emotional resilience and reduce irritability.
- Experience high morning cortisol or poor sleep → Balanced cortisol levels often improve sleep quality and energy during the day.
- Are recovering from addiction or emotional trauma → Fish oil may aid in stabilizing mood and supporting brain health during recovery.
- Want to support hormonal balance during pregnancy → Omega-3s play a vital role in both maternal well-being and fetal brain development.
In short, while anyone can take fish oil for general wellness, it is particularly valuable for people managing stress, mood, and hormone-related concerns.
⚠️ Who Should Be Cautious with Fish Oil Supplements?
Although fish oil offers powerful benefits for heart, brain, and stress management, it is not suitable for everyone. Therefore, it’s important to know when caution is needed:
- People on blood-thinning medication → Omega-3s can enhance blood-thinning effects. If you are on anticoagulants (like warfarin or aspirin), always consult your doctor first.
- Individuals with upcoming surgery → High-dose fish oil may increase bleeding risk, so it’s best to pause supplementation before medical procedures (with your doctor’s guidance).
- Those with fish or shellfish allergies → Since these capsules are derived from fish oil, allergic individuals should avoid them and consider algae-based omega-3 alternatives instead.
- Pregnant or breastfeeding women → Omega-3s are important, but dosage and source matter. Always seek medical advice for safe intake.
- Children and seniors with health conditions → Dosage and safety may vary, so professional guidance is recommended.
⚖️ What About Side Effects of Fish Oil?
In general, fish oil is safe and well-tolerated. Nevertheless, some people may notice mild side effects, especially at higher doses or with low-quality supplements:
- Fishy burps or aftertaste → This can be reduced by choosing enteric-coated capsules.
- Upset stomach or bloating → Taking fish oil with meals often minimizes digestive discomfort.
- Blood thinning at very high doses → Excess intake may increase bleeding risk, especially if combined with medication.
👉 For most healthy adults, side effects are rare and mild. However, it’s always wise to start with a moderate dose and check with a healthcare professional, particularly if you take medications or have chronic health issues
🔬 Scientific References: Fish Oil, Omega-3, and Cortisol Regulation
When we talk about lowering cortisol naturally, it’s important to back claims with real science. Fortunately, multiple clinical studies and trials show that omega-3 fatty acids from fish oil can play a measurable role in balancing stress hormones.
First, a randomized controlled trial on alcohol recovery patients found that daily fish oil supplementation reduced basal (resting) cortisol levels and improved overall emotional stability (PubMed). Similarly, a 12-week study on adolescents with depression revealed that omega-3 supplementation significantly lowered morning cortisol, supporting its role in hormonal and mood regulation (MDPI).
Moreover, research has shown that fish oil does more than just lower resting cortisol—it also helps blunt stress-induced cortisol surges. In the well-known Trier Social Stress Test (TSST), participants taking EPA-rich omega-3 supplements showed nearly 19% lower cortisol spikes compared to placebo, making them more resilient under pressure (PubMed).
Finally, beyond human trials, lab studies confirm that both EPA and DHA protect neurons from cortisol-induced damage, suggesting that omega-3s may help safeguard long-term brain health as well (Nature).
Taken together, these findings strongly suggest that omega-3 fatty acids—particularly from high-quality fish oil capsules—may help lower cortisol levels, reduce stress reactivity, and promote better mental and physical resilience.
🔗 Related Reads on Cortisol, Stress Management, and Hormonal Health
Explore more in-depth insights on how cortisol impacts your stress levels, metabolism, mood, and overall well-being:
- How Coffee Affects Cortisol, Stress, and Weight Management
Learn how caffeine and timing of your daily coffee can influence cortisol levels and body weight. - Can Drinking Tea Help Reduce Cortisol Naturally?
Discover the calming effects of herbal and green teas on stress hormone regulation. - Top 5 Cortisol-Lowering Drinks to Reduce Stress and Anxiety
Sip your way to serenity with these science-backed calming beverages. - Best Diet Strategies to Lower Cortisol Levels Naturally
A nutritionist-informed guide to eating in a way that supports balanced cortisol and mental well-being. - Omega-3 and Cortisol: How Fish Oil Supports Stress Hormone Balance
Understand how essential fatty acids like EPA and DHA help manage stress responses. - 5 Common Foods That Spike Cortisol and Increase Stress
Avoid these dietary culprits that may elevate your cortisol and disrupt hormonal balance. - 10 Warning Signs of High Cortisol in Women
A detailed look at symptoms and hormonal patterns specific to females with elevated cortisol. - 5 Foods That Naturally Help Lower Cortisol and Promote Calm
Add these anti-stress superfoods to your diet for better mood and lower cortisol levels.
🧘 Final Thoughts: Omega-3 as Nature’s Stress Shield
In today’s high-pressure world, stress is impossible to avoid. However, the way your body responds to stress can be improved with the right nutrients. Fish oil, rich in omega-3 fatty acids, does not eliminate stress instantly; yet, it helps the body manage stress more effectively over time.
Clinical studies suggest that omega-3s may lower elevated cortisol levels, improve resilience to daily challenges, and reduce the intensity of stress-related symptoms such as anxiety, fatigue, and poor sleep. In other words, consistent supplementation can gradually create a calmer, more balanced response to life’s pressures.
Moreover, unlike quick fixes such as caffeine or sugar, omega-3 fatty acids support long-term brain, heart, and hormonal health—making them a reliable addition to any holistic wellness plan.
👉 If you’re feeling overwhelmed, burned out, or anxious, it may be the right moment to support your nervous system naturally. Adding a high-quality fish oil supplement could be one of the simplest, evidence-based ways to protect your mind and body from the hidden toll of stress.
🧠 10 FAQs About Fish Oil and Cortisol
1. Can fish oil really help lower cortisol levels?
Yes, several human studies have shown that regular intake of fish oil—especially EPA and DHA—can help reduce both basal cortisol and stress-induced cortisol spikes.
2. How much fish oil should I take to lower cortisol?
For general cortisol regulation, a dose between 1–2.5 grams of combined EPA and DHA daily is typically effective. Higher EPA concentrations seem to work best for stress.
3. Which is better for cortisol—EPA or DHA?
While both are beneficial, EPA-rich fish oil appears to be more effective in blunting cortisol spikes in response to stress, based on current studies.
4. How long does it take for fish oil to affect cortisol?
Improvements have been observed in as little as 3 to 8 weeks. Long-term use may offer more stable hormonal support.
5. Can fish oil help with anxiety and mood along with cortisol?
Yes. Lowering cortisol can help reduce symptoms of anxiety, and omega-3s also support mood regulation independently through anti-inflammatory pathways in the brain.
6. Is it safe to take fish oil every day?
Yes. Fish oil is generally safe for daily use, especially when taken within recommended dosages (1–3 grams per day). Consult your doctor if you’re on medication or pregnant.
7. What are the best fish oil supplements for cortisol reduction?
Look for high-quality, third-party tested fish oil supplements with at least 1000 mg of EPA+DHA per serving, preferably with a higher EPA ratio for stress support.
8. Can I get the same benefits from eating fish?
Yes, fatty fish like salmon, sardines, and mackerel are excellent sources of omega-3s. Aim for 2-3 servings per week for general hormonal and cardiovascular health.
9. Can fish oil interact with medications?
Yes, particularly blood thinners and blood pressure medications. Always consult your healthcare provider before starting supplements.
10. What other lifestyle changes should I combine with fish oil for cortisol management?
For best results, combine fish oil with adequate sleep, regular exercise, stress management (like meditation), and a balanced diet to naturally reduce cortisol levels.