Introduction
Ferritin, a crucial protein in the human body, plays a vital role in storing and releasing iron as needed. It’s like a reservoir, ensuring that we have a steady supply of iron for various bodily functions. However, the balance of ferritin and iron in our system is delicate and can be disrupted by numerous health conditions, ranging from kidney disease to anemia. Understanding the dynamics of ferritin levels, their causes, symptoms, and how they are managed is essential for maintaining good health.
Section 1: Basic Understanding of Ferritin and Iron in the Body
Subsection 1.1: What is Ferritin?
Ferritin is more than just a storage protein for iron; it’s a key player in regulating iron’s availability in the body. It’s found in almost all living organisms, from bacteria to plants to humans, indicating its fundamental role in biological processes. In humans, ferritin is present in various tissues, with significant amounts in the liver, spleen, and bone marrow.
But why is ferritin so important? The answer lies in its unique ability to store iron in a non-toxic form and release it when needed. Each ferritin molecule can hold up to 4,500 iron atoms, keeping them safe and readily accessible. This mechanism is crucial because while iron is essential for functions like oxygen transport and energy production, it can be harmful in excess, leading to cellular damage.
Subsection 1.2: Role of Iron in the Body
Iron’s primary role in the body is in the production of hemoglobin, a component of red blood cells that carries oxygen from the lungs to the rest of the body. Iron also contributes to the creation of myoglobin, a protein that provides oxygen to muscles, and is involved in various other cellular functions, including energy production and DNA synthesis.
However, our body cannot produce iron; we must obtain it from our diet. Foods rich in iron include red meat, beans, nuts, and fortified cereals. Once absorbed, iron is either used immediately, stored as ferritin, or transported throughout the body bound to a protein called transferrin.
Subsection 1.3: Relationship Between Ferritin and Iron
The relationship between ferritin and iron in the body is a dynamic one. When iron levels are high, more ferritin is produced to store the excess iron safely. Conversely, when iron levels are low, ferritin releases its stored iron to maintain a balance.
Monitoring ferritin levels through blood tests helps in understanding the body’s iron status. A low ferritin level indicates depleted iron stores, often leading to iron deficiency anemia if not addressed. On the other hand, high ferritin levels might indicate conditions like hemochromatosis, where there’s too much iron in the body, or be a response to inflammation.
Understanding ferritin and iron’s roles is the first step in recognizing the signs and managing conditions related to their imbalance. In the following sections, we will delve deeper into various health conditions associated with ferritin levels, their symptoms, and effective treatment strategies.
Section 2: Health Conditions Related to Ferritin Levels
Subsection 2.1: Low Ferritin Levels and Kidney Disease
Ferritin levels can be a critical indicator in diagnosing and managing kidney diseases. Kidneys play a significant role in creating red blood cells by producing erythropoietin, a hormone that stimulates their production. When kidneys are not functioning optimally, they may produce less erythropoietin, leading to a decrease in red blood cell production and, consequently, low ferritin levels. This condition is often observed in chronic kidney disease (CKD) patients and can exacerbate their health challenges.
Subsection 2.2: High Ferritin with Low Iron: Understanding the Paradox
It may seem contradictory, but it’s possible to have high ferritin levels while also having low iron levels in the body. This scenario often occurs in inflammatory conditions, where ferritin acts as an acute phase reactant. The inflammation causes the liver to release more ferritin as a defense mechanism, regardless of the body’s actual iron levels. This paradoxical situation can be seen in chronic diseases like rheumatoid arthritis and certain infections.
Subsection 2.3: Anemia and Elevated Ferritin
Anemia with elevated ferritin levels is an unusual combination, often pointing to anemia of chronic disease (ACD). ACD is typically seen in individuals suffering from long-term medical conditions like infections, cancer, or autoimmune diseases. In this scenario, the body has adequate iron stores (reflected by high ferritin) but cannot effectively utilize the iron due to the underlying condition.
Subsection 2.4: Low Ferritin with Normal Iron Levels
Having low ferritin with normal iron levels suggests that the body’s iron stores are beginning to deplete, but there’s still enough iron in the bloodstream. This condition can be a precursor to iron deficiency anemia and often serves as an early warning sign. It’s essential to monitor and manage ferritin levels at this stage to prevent further complications.
Subsection 2.5: Iron Saturation: Low Ferritin and Its Implications
Iron saturation refers to the percentage of transferrin (the iron transport protein) that is saturated with iron. Low ferritin combined with low iron saturation is a clear indicator of iron deficiency. This condition can have various causes, including inadequate dietary iron intake, chronic blood loss, or issues with iron absorption.
Subsection 2.6: Iron Deficiency Without Anemia
Iron deficiency without anemia is a condition where there is a decrease in iron stores (low ferritin) but not yet enough to cause anemia. This stage is often referred to as “pre-anemia” or “latent iron deficiency.” It can be challenging to diagnose because, despite the low iron stores, hemoglobin levels remain normal. Symptoms might be subtle or non-existent, but they can include fatigue, weakness, or decreased immune function. This condition is particularly concerning because it often goes unnoticed until it progresses to iron deficiency anemia.
Subsection 2.7: Celiac Disease and Low Ferritin
Celiac disease, an autoimmune disorder where the ingestion of gluten leads to damage in the small intestine, can also impact ferritin levels. The damage to the small intestine can lead to malabsorption, which includes the reduced absorption of iron, leading to depleted ferritin stores. Individuals with celiac disease often have nutrient deficiencies, including iron, which can manifest as low ferritin levels. It’s essential for patients with celiac disease to be regularly monitored for iron deficiency, as it can contribute to anemia and other health complications.
Section 3: Symptoms and Diagnosis
Subsection 3.1: Identifying Symptoms of Low Ferritin
The symptoms of low ferritin are often subtle and can be easily overlooked. Common signs include:
- Fatigue and Weakness: A lack of iron in the body can lead to decreased oxygen supply to the tissues, causing persistent tiredness.
- Hair Loss: Iron is crucial for hair growth. Low ferritin levels can disrupt the hair growth cycle, leading to hair loss.
- Restless Leg Syndrome: Low iron levels have been linked to restless leg syndrome, a condition characterized by an uncomfortable sensation in the legs and an uncontrollable urge to move them.
- Impaired Immune Function: Iron plays a vital role in immune health; low ferritin levels can lead to increased susceptibility to infections.
- Pale Skin: Iron deficiency can cause the skin and mucous membranes to lose their normal color, resulting in paleness.
Subsection 3.2: Ferritin Blood Test: Understanding the Process and Costs
A ferritin blood test is a simple yet effective diagnostic tool to assess the body’s iron stores. The test measures the amount of ferritin in the blood, providing insight into the total iron available in the body. It’s typically performed alongside other blood tests, such as hemoglobin and hematocrit, to give a complete picture of an individual’s iron status.
The cost of a ferritin blood test can vary depending on several factors, including geographic location, healthcare provider, and insurance coverage. Generally, the test is affordable and widely accessible. It’s important for individuals at risk of iron deficiency, such as women of childbearing age, vegetarians, and people with chronic conditions, to undergo regular ferritin testing.
Subsection 3.3: At-Home Tests for Low Iron and Ferritin
Advancements in medical technology have made it possible to test ferritin levels at home. These at-home test kits typically involve collecting a small blood sample, usually through a finger prick, and sending it to a laboratory for analysis. The results are then provided online or via a mobile app. While these tests offer convenience and privacy, it’s crucial to discuss the results with a healthcare professional for accurate interpretation and advice.
Section 4: Treatment and Management
Subsection 4.1: Treatments for Low Ferritin and Iron Deficiency
Treating low ferritin and iron deficiency involves a multifaceted approach:
- Dietary Changes: Increasing the intake of iron-rich foods, such as red meat, poultry, fish, legumes, and fortified cereals, can help boost ferritin levels.
- Iron Supplements: Oral iron supplements are commonly prescribed to increase ferritin levels. They are effective but can sometimes cause gastrointestinal side effects like constipation or nausea.
- Treating Underlying Causes: If the low ferritin is due to an underlying condition like celiac disease or chronic blood loss, addressing the root cause is essential.
- Monitoring: Regular monitoring of ferritin levels is crucial to ensure that the treatment is effective and to prevent recurrence of deficiency.
Subsection 4.2: Supplements for Managing Low Ferritin
When choosing supplements for low ferritin, it’s important to consider the type of iron. Ferrous sulfate, ferrous gluconate, and ferrous fumarate are common forms, with varying absorption rates and side effects. It’s often recommended to take iron supplements on an empty stomach to enhance absorption, but for those who experience gastrointestinal issues, taking them with food can mitigate these side effects. Vitamin C is known to enhance iron absorption, so pairing iron supplements with a source of this vitamin can be beneficial.
Subsection 4.3: Dietary Approaches and Best Iron Sources
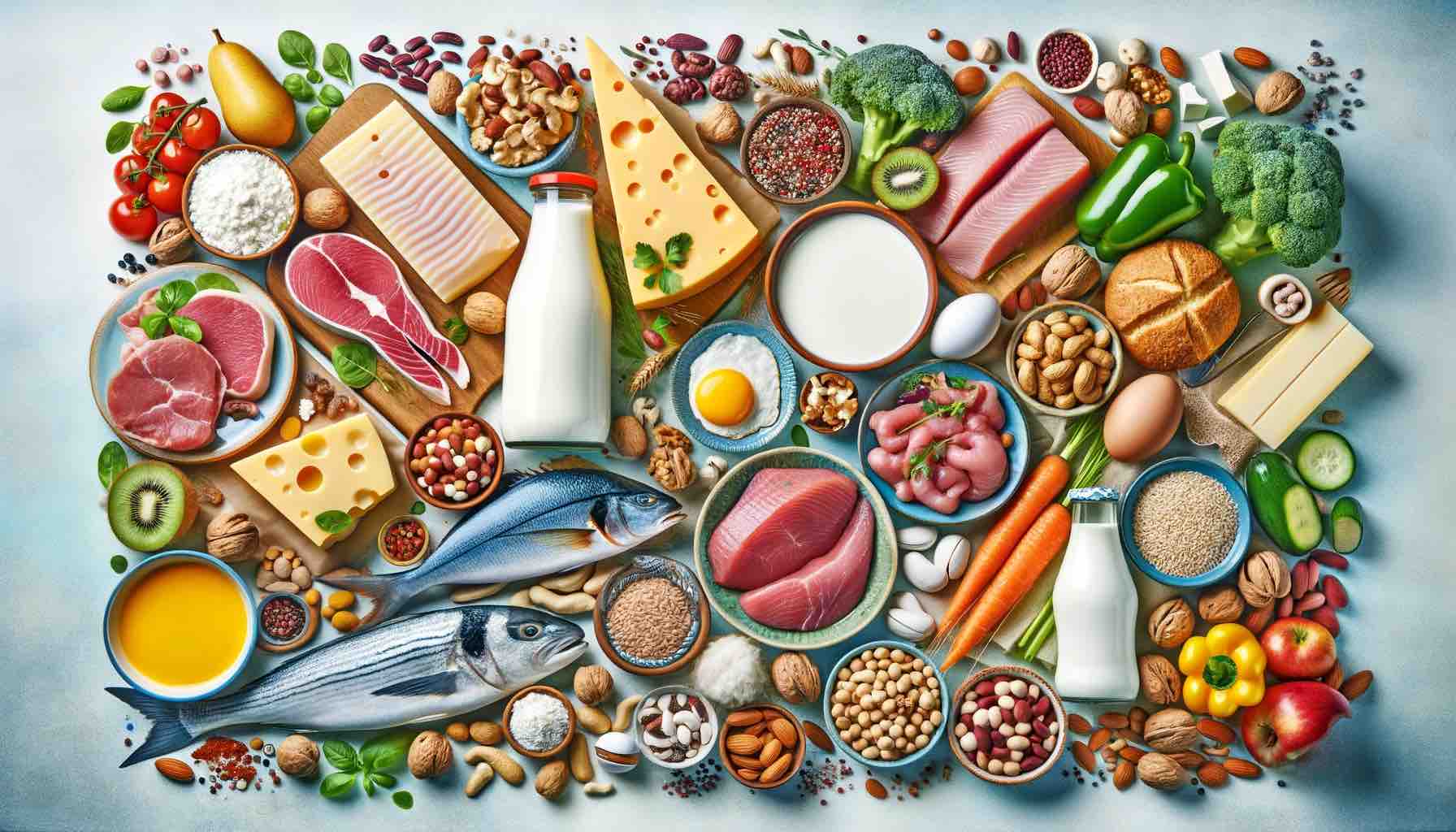
D
iet plays a crucial role in managing ferritin levels. Iron-rich foods are divided into two categories: heme iron (found in animal products) and non-heme iron (found in plant-based foods). Heme iron, which is more readily absorbed by the body, is abundant in meats, especially red meats. Non-heme iron sources include legumes, nuts, seeds, whole grains, and green leafy vegetables. To enhance the absorption of non-heme iron, it’s advisable to consume them with vitamin C-rich foods like citrus fruits, tomatoes, and bell peppers.
Subsection 4.4: IV Iron Therapy and Its Applications
Intravenous (IV) iron therapy is a treatment option for individuals who cannot tolerate oral iron supplements or those with severe iron deficiency anemia. This therapy involves delivering iron directly into the bloodstream, bypassing the gastrointestinal tract, and is usually done in a hospital or a clinic. IV iron therapy can quickly replenish iron stores and is particularly beneficial for patients with chronic kidney disease, inflammatory bowel disease, or those who have had bariatric surgery.
Section 5: Special Considerations
Subsection 5.1: Ferritin Levels in Women: Unique Concerns
Women, particularly those of childbearing age, face unique challenges regarding ferritin levels due to factors like menstruation, pregnancy, and breastfeeding. Menstruation can lead to significant iron loss each month, increasing the risk of low ferritin levels. During pregnancy, the body’s demand for iron increases to support the growing fetus and placenta and to expand the maternal red blood cell mass. Low ferritin levels in pregnant women can lead to complications such as preterm delivery and low birth weight. Breastfeeding also requires additional iron, and without proper dietary intake or supplementation, ferritin levels can drop.
Subsection 5.2: Low Ferritin in Autoimmune Diseases like Lupus and MS
Autoimmune diseases such as Lupus (Systemic Lupus Erythematosus) and Multiple Sclerosis (MS) can impact ferritin levels. Chronic inflammation, a hallmark of these conditions, can disrupt iron metabolism, leading to anemia of chronic disease. The inflammatory process can cause the body to shift iron into storage within ferritin, making it less available for red blood cell production. Regular monitoring of ferritin and iron levels is vital in managing these conditions effectively.
Subsection 5.3: The Impact of Alcohol on Ferritin Levels
Alcohol consumption can have a complex effect on ferritin levels. Chronic alcohol use can lead to liver damage, where most of the body’s ferritin is stored. Liver damage can cause ferritin to leak into the bloodstream, artificially raising ferritin levels. However, this does not necessarily indicate adequate iron stores, as the body’s ability to use this iron can be compromised. Conversely, alcohol can also contribute to nutritional deficiencies, including iron deficiency, particularly in individuals with alcohol use disorders who may have poor dietary habits.
Subsection 5.4: Understanding Ferritin Levels in Cancer Patients
In cancer patients, ferritin levels can be a double-edged sword. Some cancers can cause elevated ferritin levels due to increased production by cancer cells or as a response to inflammation and tissue damage. High ferritin levels in cancer patients can sometimes be a marker of tumor burden or a prognostic indicator. On the other hand, treatments such as chemotherapy can lead to decreased production of red blood cells, thereby reducing ferritin levels. Anemia and low ferritin are common in cancer patients and can significantly impact their quality of life and response to treatment.
Conclusion
Understanding ferritin levels is crucial in diagnosing and managing a wide range of health conditions. From kidney disease and autoimmune disorders to pregnancy and cancer, ferritin serves as an important biomarker for overall health and well-being. Recognizing the signs of ferritin imbalances, undergoing regular testing, and adopting appropriate treatment strategies are key steps in maintaining optimal health.
It’s essential for individuals, especially those at higher risk of iron imbalances, to work closely with healthcare professionals to monitor and manage their ferritin levels effectively. By doing so, they can address potential health issues early and maintain a healthier, more balanced life.
Remember, while this guide provides comprehensive information on ferritin and its impact on health, it’s always advisable to seek personalized advice from healthcare providers for specific concerns and conditions.
10 FAQs for the Blog Post
- What are common signs of low ferritin levels in the body?
- Common signs of low ferritin include fatigue, hair loss, restless leg syndrome, impaired immune function, and pale skin. These symptoms occur due to the reduced availability of iron for essential bodily functions.
- How can diet influence ferritin and iron levels?
- Diet plays a significant role in managing ferritin and iron levels. Consuming iron-rich foods like red meat, poultry, fish, legumes, and fortified cereals can boost ferritin levels. Additionally, pairing non-heme iron sources (plant-based) with vitamin C-rich foods enhances iron absorption.
- What is the relationship between celiac disease and ferritin levels?
- In celiac disease, the damage to the small intestine leads to malabsorption, including iron, resulting in low ferritin levels. Regular monitoring for iron deficiency is essential for those with celiac disease to prevent anemia and other health complications.
- Why might someone have high ferritin but low iron levels?
- This paradoxical situation can occur in inflammatory conditions, where the body increases ferritin production as a defense mechanism, despite low iron levels. It’s commonly seen in chronic diseases like rheumatoid arthritis.
- Can ferritin levels affect hair health?
- Yes, ferritin plays a crucial role in hair health. Low ferritin levels can disrupt the hair growth cycle, potentially leading to hair loss. Maintaining adequate ferritin levels is important for healthy hair growth.
- What are the implications of low ferritin in pregnancy?
- During pregnancy, the demand for iron increases. Low ferritin levels in pregnant women can lead to complications like preterm delivery and low birth weight. It’s important for pregnant women to monitor and manage their ferritin levels.
- How does alcohol consumption affect ferritin levels?
- Chronic alcohol use can lead to liver damage, causing ferritin to leak into the bloodstream, which may raise ferritin levels. However, this does not necessarily indicate adequate iron stores, as alcohol can also contribute to nutritional deficiencies, including iron deficiency.
- What role does ferritin play in autoimmune diseases like Lupus and MS?
- In autoimmune diseases, chronic inflammation can disrupt iron metabolism, leading to anemia of chronic disease. This process causes the body to shift iron into storage within ferritin, making it less available for red blood cell production.
- Are there any specific considerations for cancer patients regarding ferritin levels?
- Yes, in cancer patients, ferritin levels can be indicative of tumor burden or a response to inflammation and tissue damage. Treatments like chemotherapy can also reduce ferritin levels, leading to anemia.
- What are the treatment options for low ferritin and iron deficiency?
- Treatment options include dietary changes to include more iron-rich foods, oral iron supplements, addressing underlying causes, and regular monitoring. In severe cases, intravenous (IV) iron therapy might be recommended.
Blog Tags for the Post
iron deficiency, ferritin levels, anemia, kidney disease, celiac disease, iron-rich diet, iron supplements, hair loss and iron, pregnancy iron needs, alcohol and ferritin, autoimmune disease and ferritin, cancer and ferritin, iron absorption, iron tests, iron treatment