Coriander, often regarded as a staple in global cuisine, is more than just a flavorful herb. It has a long history in traditional medicine, particularly in Ayurveda, for its potential health benefits. While most of us are familiar with coriander leaves, the seeds of the plant, often referred to as coriander seeds or dhania, are an unsung hero in the world of herbal remedies. In recent years, these tiny seeds have been gaining attention for their potential role in supporting thyroid health.
The thyroid, a small butterfly-shaped gland located at the base of the neck, plays a crucial role in regulating metabolism, energy production, and overall hormonal balance in the body. Disruptions to thyroid function, whether from hypothyroidism (underactive thyroid) or hyperthyroidism (overactive thyroid), can have significant impacts on physical and emotional well-being. This has led many to explore natural ways to support thyroid health, with coriander seeds emerging as a promising option.
In this post, we’ll delve deep into the benefits of coriander seeds for thyroid health, their potential risks, and how to safely incorporate them into your diet.
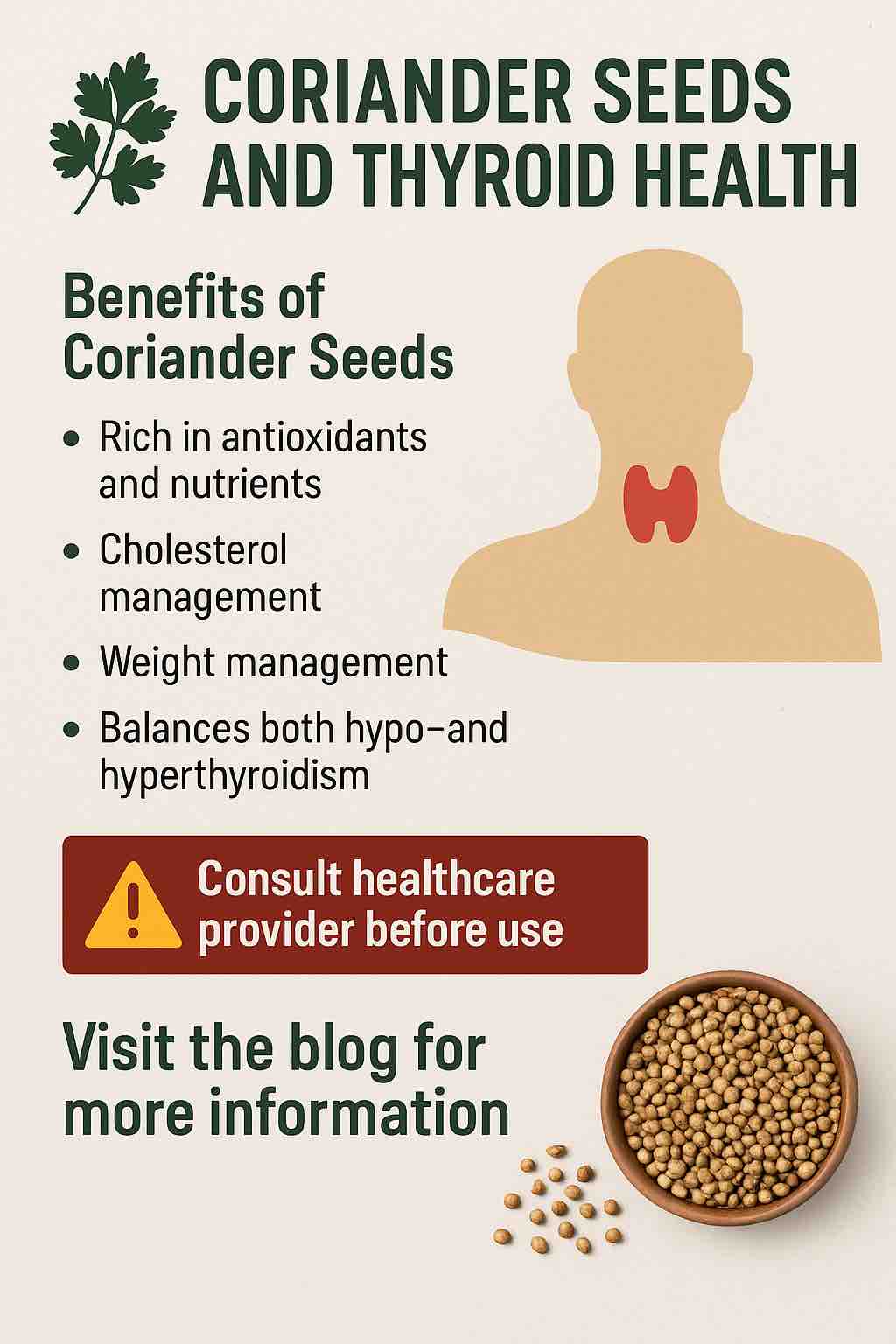
The Surprising Benefits of Coriander Seeds for Thyroid Health
1. Rich in Antioxidants and Essential Nutrients
Coriander seeds are a powerhouse of essential vitamins, minerals, and antioxidants. They are an excellent source of vitamin C, which is crucial for maintaining a healthy immune system and reducing oxidative stress. The seeds are also rich in vitamin A, vitamin K, folate, and several essential minerals like iron, calcium, and magnesium.
When it comes to thyroid health, antioxidants play an important role. The thyroid gland, like many other organs, is susceptible to damage from free radicals. Coriander seeds, with their rich antioxidant content, can help reduce oxidative damage, supporting the thyroid’s ability to function optimally.
Additionally, coriander seeds contain phytochemicals that may help reduce inflammation in the body. Chronic inflammation is a known contributor to autoimmune thyroid conditions, such as Hashimoto’s thyroiditis (an autoimmune form of hypothyroidism), and managing inflammation can be a key step in supporting thyroid health.
2. Supporting Cholesterol Management
Thyroid dysfunction often impacts cholesterol levels. People with hypothyroidism may experience elevated cholesterol, which can increase the risk of heart disease. Interestingly, coriander seeds have been shown to help in managing cholesterol levels.
Coriander seeds contain compounds that may help lower bad cholesterol (LDL) while boosting good cholesterol (HDL) levels. This dual effect on cholesterol can be particularly beneficial for individuals dealing with thyroid imbalances, as it can help mitigate the cardiovascular risks associated with thyroid dysfunction.
3. Supporting Weight Management in Hypothyroidism
One of the most challenging symptoms of hypothyroidism is weight gain, often caused by a slow metabolism. As thyroid hormones regulate metabolism, an underactive thyroid can cause weight to accumulate, even with a relatively healthy diet.
Coriander seeds, when consumed in the form of coriander seed water, can help stimulate weight loss. The high fiber content of coriander seeds aids in digestion, supports gut health, and helps regulate blood sugar levels. Drinking coriander seed water regularly has been linked to improved metabolic function, which can support weight management in individuals with hypothyroidism.
4. Balances Both Hypo- and Hyperthyroidism
Traditional medicine, particularly Ayurveda, suggests that coriander seeds have a balancing effect on the thyroid. Whether the thyroid is underactive or overactive, coriander seeds are believed to have the ability to bring the thyroid hormones into balance. The seeds contain compounds that may support normal thyroid function, thus helping to manage both hypothyroidism and hyperthyroidism. However, it’s important to note that the exact mechanisms are still not fully understood, and individual responses can vary.
Potential Risks and Important Warnings
While coriander seeds can offer numerous benefits for thyroid health, there are some important precautions and risks to consider.
1. Coriander Seeds Are Not a Substitute for Medical Treatment
Coriander seeds, while beneficial, should never be considered a substitute for conventional medical treatment for thyroid disorders. Individuals with thyroid conditions, especially those on medications such as levothyroxine for hypothyroidism, should continue their prescribed treatment under the supervision of a healthcare provider.
Coriander seeds can support thyroid health as part of a broader, holistic approach, but they should not replace medical advice or prescribed treatments.
2. Possible Interference with Thyroid Function Tests
One surprising risk of consuming coriander seeds is their potential interference with thyroid function tests (TFTs). Certain compounds in coriander, when consumed in large quantities, have been reported to affect the results of these tests. This could lead to misleading diagnoses or delays in identifying thyroid dysfunction, particularly in individuals who are undergoing regular monitoring of their thyroid function.
If you are undergoing thyroid testing, it is advisable to consult your healthcare provider about the inclusion of coriander seeds in your diet, especially if you plan to consume them in larger quantities.
3. Allergic Reactions and Sensitivities
Like any food or herb, coriander seeds can cause allergic reactions in some individuals. Symptoms can range from mild irritation, such as skin rashes, to more serious reactions like digestive discomfort. If you are new to coriander seeds, it is a good idea to start with a small amount and observe how your body reacts.
Additionally, coriander seeds are part of the Apiaceae family, which includes other herbs like parsley, celery, and fennel. If you have an allergy to any of these foods, you may be more likely to experience an adverse reaction to coriander.
4. Interactions with Medications
Coriander seeds have hypoglycemic properties, meaning they may help lower blood sugar levels. While this can be beneficial for individuals with diabetes, it can pose a risk for people taking anti-diabetic medications like insulin. The combination of coriander and blood sugar-lowering drugs may cause blood sugar levels to drop too low, leading to hypoglycemia. If you are on medication for diabetes, it’s essential to consult your healthcare provider before adding coriander seeds to your diet.
How to Safely Incorporate Coriander Seeds into Your Diet
If you’re eager to experience the potential benefits of coriander seeds for thyroid health, here are a few simple ways to include them in your daily routine:
1. Coriander Seed Water
One of the easiest and most popular ways to consume coriander seeds is by making coriander seed water. Here’s how:
- Soak 1-2 teaspoons of coriander seeds in water overnight.
- In the morning, boil the water with the seeds.
- Once boiled, strain the water and drink it on an empty stomach.
This practice is thought to support digestion, improve metabolic function, and provide the nutrients necessary for thyroid health.
2. Coriander Seed Tea
Another easy method is to make coriander seed tea:
- Boil soaked coriander seeds in water for 10-15 minutes.
- Strain the water and drink it warm.
- You can add honey or a squeeze of lemon for added flavor.
Drinking this tea in the morning can help kickstart your metabolism and provide a gentle detox to start your day.
Conclusion
Coriander seeds offer an impressive array of health benefits, particularly for individuals managing thyroid conditions. From supporting antioxidant activity to helping regulate cholesterol and weight, these seeds can play a supportive role in thyroid health. However, it’s essential to approach their use with caution, recognizing that they should complement, not replace, conventional medical treatments.
Before incorporating coriander seeds into your diet, especially if you are managing a thyroid condition or taking medications, always consult with a healthcare provider to ensure safety and appropriateness.
With their rich nutritional profile and potential thyroid-supporting properties, coriander seeds could become a valuable part of your wellness routine. Just remember: moderation, awareness, and consultation with a healthcare provider are key to reaping the benefits while avoiding any risks.
FAQs About Coriander Seeds and Thyroid Health
1. Can coriander seeds help with hypothyroidism?
Yes, coriander seeds may support hypothyroidism by helping to balance thyroid hormone levels and improving metabolism. They are believed to aid in weight management, cholesterol control, and digestive health, which can be beneficial for individuals with an underactive thyroid.
2. Are coriander seeds effective for hyperthyroidism?
Coriander seeds may help in managing hyperthyroidism by balancing thyroid hormone levels. Their anti-inflammatory and antioxidant properties may support overall thyroid health, though their effectiveness can vary from person to person.
3. How do coriander seeds benefit thyroid function?
Coriander seeds are rich in antioxidants, essential vitamins, and minerals that support thyroid health. They help reduce oxidative stress and inflammation, which can aid in maintaining optimal thyroid function. They also help regulate cholesterol and weight, which can be impacted by thyroid imbalances.
4. What’s the best way to consume coriander seeds for thyroid health?
Coriander seed water and coriander seed tea are two popular methods. To make coriander seed water, soak 1-2 teaspoons of coriander seeds in water overnight, boil the water in the morning, strain, and drink. For tea, boil soaked seeds in water and drink after straining.
5. Are there any risks to consuming coriander seeds for thyroid health?
While coriander seeds are generally safe, they may interfere with thyroid function tests, cause allergic reactions in some individuals, or interact with certain medications, especially those for diabetes. Always consult your doctor before adding coriander seeds to your routine.
6. Can coriander seeds help with weight loss in people with thyroid issues?
Yes, coriander seeds may help stimulate weight loss by improving digestion, regulating blood sugar, and boosting metabolism. This can be especially beneficial for individuals with hypothyroidism, as weight gain is a common symptom of an underactive thyroid.
7. Can coriander seeds replace thyroid medications?
No, coriander seeds cannot replace thyroid medications such as levothyroxine. They should be used as a complementary approach, not a substitute for prescribed treatments. Always follow your healthcare provider’s recommendations for thyroid management.
8. How much coriander seed water should I drink daily for thyroid health?
It’s generally recommended to drink 1 cup (approximately 250 ml) of coriander seed water daily, preferably in the morning on an empty stomach. However, always start with small amounts to assess tolerance.
9. Can coriander seeds interfere with blood sugar medications?
Yes, coriander seeds have hypoglycemic effects and may lower blood sugar levels. If you are on anti-diabetic medications, consult your healthcare provider before consuming coriander seeds to avoid potential interactions or hypoglycemia.
10. Are there any side effects from consuming coriander seeds?
In most cases, coriander seeds are safe when consumed in moderation. However, some people may experience digestive discomfort or skin rashes, especially if they are allergic to the herb. Always start with a small quantity to monitor your body’s response.













