Milk allergy—often called cow’s milk protein allergy (CMPA)—happens when the immune system reacts to milk proteins (mainly casein and whey). That reaction or Milk Allergy Symptoms can show up on the skin, in the gut, in the airways, or—when severe—across the whole body. By contrast, lactose intolerance is trouble digesting the milk sugar (lactose) and is uncomfortable but not dangerous. If you want clinician-grade context as you read, the EAACI guideline on IgE-mediated food allergy covers allergy mechanisms and care, and NIDDK’s lactose intolerance pages explain why intolerance feels so different.
Quick note: This guide is educational and not a substitute for medical advice. If you suspect a milk allergy—especially in an infant—please speak to your clinician.
What “Milk Allergy Symptoms” Can Look Like
Because milk allergy is an immune reaction, symptoms don’t look the same for everyone. Timing helps: some symptoms appear quickly (often within minutes to two hours) and are typically IgE-mediated; others are delayed (hours to a couple of days) and tend to be gut-focused or eczema-like. Recognizing both patterns explains why one child may get hives right away while another develops slow-burn tummy issues later.
Faster (often IgE-type) symptoms
- Itchy hives (wheals), flushing, or rapidly spreading rash
- Swelling of lips, eyelids, face, or tongue
- Vomiting shortly after milk exposure
- Cough, wheeze, chest tightness, voice change
- Dizziness or fainting from a drop in blood pressure (anaphylaxis)
Slower (often non-IgE) symptoms
- Eczema flares that are stubborn despite good skin care
- Ongoing gastrointestinal issues: abdominal pain, diarrhea, excessive gas
- In infants: mucus or blood in stools, distress with feeds, reflux-like irritability
- Feeding difficulties or poor weight gain in persistent cases
Emergency signs—act now: trouble breathing, throat tightness, repeated vomiting, sudden drowsiness/fainting, or widespread hives with breathing symptoms. Use epinephrine if prescribed and get urgent care. The latest Anaphylaxis Practice Parameter is crystal clear: epinephrine is first-line and should not be delayed.
CMPA Symptoms in Newborns & Infants (What Parents Actually Notice)
Milk allergy commonly presents in the first year of life. Not every fussy baby has CMPA, of course, but clinicians look for patterns across skin, gut, and feeding.
Skin
- Facial rash on the cheeks or scattered body rashes that worsen around feeds
- Eczema that’s difficult to control despite moisturizers and steroid creams
Gut
- Frequent regurgitation or vomiting; back-arching or discomfort during feeds
- Stools with mucus or streaks of blood in some non-IgE presentations
- Diarrhea, cramping, significant gas; occasionally constipation
Feeding and Growth
- Irritability during or after feeds; pushing the bottle/breast away
- Poor weight gain when symptoms persist over time
- Symptoms from tiny exposures via cross-contact in more sensitive infants
If you’re navigating formula or breastfeeding decisions, the World Allergy Organization’s DRACMA updates are the most practical, current references on nutrition: WAO DRACMA—Nutritional management of CMA. In short: extensively hydrolyzed formula (eHF) is typically first-line; amino-acid formula (AAF) is considered if symptoms persist or are severe; in some settings, hydrolyzed rice formulas can be options. Breastfeeding can continue, but in select cases your clinician may suggest a short, guided trial of maternal dairy elimination.
Important reminder before changes: Infant feeding is personal and should be supervised. Please talk to your pediatrician/allergist before switching formula or altering a breastfeeding diet.
For parents also dealing with skin flares, you might find our gentle, practical read on Milk and Eczema helpful—it explains how allergy (protein) and intolerance (lactose) affect skin differently and what actually helps.
Milk Allergy Symptoms in Adults
Adults can absolutely have milk allergy (even though many adult “dairy issues” turn out to be lactose intolerance). Adult allergy symptoms often mirror pediatric ones:
- Skin: hives, flushing, swelling
- Gut: cramping, nausea, vomiting, diarrhea
- Respiratory: coughing, wheeze, throat tightness
- Systemic: dizziness or fainting in severe reactions (anaphylaxis)
Because the overlap with intolerance confuses things, it helps to separate the two. If your symptoms are mainly gas, bloating, and diarrhea—especially 30 to 120 minutes after dairy—and you don’t get hives or breathing issues, lactose intolerance is more likely. For a clear, patient-friendly explainer, see NIDDK: symptoms & causes and NIDDK: diagnosis & tests.
If you’re testing the waters with dairy alternatives, our practical round-ups are handy: Easy Homemade Oat Milk, Dairy-Free Chocolate Syrup, and Chia Puddings (Dairy-Free).
Milk Allergy vs Lactose Intolerance (Plain-English, Side-by-Side)
Allergy = immune reaction to proteins.
Intolerance = enzyme problem with lactose sugar.
One can be dangerous; the other is uncomfortable.
| Feature | Milk Allergy (CMA/CMPA) | Lactose Intolerance |
|---|---|---|
| What’s reacting? | Immune system to proteins (casein/whey) | Low lactase enzyme → can’t digest lactose |
| Timing | Minutes–2 hours (IgE) or delayed (non-IgE) | 30 minutes–several hours after lactose |
| Typical symptoms | Hives, swelling, vomiting, cough/wheeze; anaphylaxis possible; delayed eczema/GI | Gas, bloating, cramps, diarrhea |
| Confirmation | History + tests; sometimes oral food challenge | Breath tests (hydrogen/methane), diet trial |
| Is lactose-free milk safe? | No (proteins still present) | Often yes |
For clinical background while you compare, the EAACI food-allergy guideline and NIDDK’s lactose pages are reliable.
If you prefer a lifestyle-focused read on cutting dairy, we have a practical overview: The Health Benefits of Going Dairy-Free.
How Doctors Actually Diagnose a Milk Allergy
Heads up before we dig into tests: Only a healthcare professional can diagnose a milk allergy. Tests help, but context is everything. The safest way to confirm—when needed—is a supervised oral food challenge.
Step 1: History + examination
A clinician maps symptoms to timing, amount eaten, and previous reactions. Recognizing immediate versus delayed patterns helps decide which tests to run and how to interpret them. The EAACI guideline walks through this approach.
Step 2: Allergy tests (supportive—not yes/no by themselves)
- Skin-prick testing (SPT) to milk and/or milk protein components
- Blood tests for specific IgE, e.g., to whole milk, casein, or whey proteins
These results must be interpreted alongside the story. High numbers don’t automatically mean “more allergic,” and low numbers don’t always mean “safe.”
Step 3: Oral Food Challenge (OFC) when needed
A carefully planned OFC in a clinic confirms allergy or tolerance; it’s also used to check whether a child can handle baked milk. This is the gold standard—never try challenges at home. For protocols and safety notes, see AAAAI: Conducting an Oral Food Challenge (2020 update).
What about “at-home allergy tests”?
Kits (like IgG panels or hair analysis) are not validated to diagnose food allergy and can mislead decisions. If you’re unsure, it’s safer to speak with an allergist and rely on validated methods.
Meanwhile, for lactose intolerance
If the story points to intolerance, clinicians may use hydrogen/methane breath tests or structured diet trials. These diagnose intolerance, not allergy. Here’s what to expect: NIDDK: Diagnosis of Lactose Intolerance.
The “Baked Milk” Pathway (Why It Matters—and Why You Shouldn’t DIY)
Some children with IgE-mediated milk allergy can tolerate extensively heated (baked) milk in foods like muffins or biscuits. Research suggests that children who safely add baked milk—as part of an allergist-guided plan—often outgrow their milk allergy sooner than those who strictly avoid all dairy. Conversely, reacting to baked milk tends to predict a more persistent allergy. A widely cited study summarizing this approach: Dietary baked milk accelerates resolution of cow’s milk allergy in children (JACI).
Plain English: There may be a bridge to tolerance for some kids, but it needs a plan and monitoring. Don’t trial baked milk without medical guidance.
Treatment & What To Do During Reactions
Safety reminder first: If breathing is difficult, the voice sounds tight, or there’s repeated vomiting or fainting—that’s an emergency. Use epinephrine (if prescribed) and seek urgent care. Antihistamines can reduce itch and hives but don’t treat airway or blood-pressure problems. The evidence-based steps are summarized in the Anaphylaxis Practice Parameter (2023).
Day-to-day management (everyone)
- Avoid milk proteins (casein, caseinate, whey). Read labels carefully; lactose-free milk still contains milk proteins and is not safe for allergy.
- If you or your child has had systemic reactions, carry epinephrine autoinjectors and keep a written action plan at home, school, and day-care. Practice with your device so you’re confident under stress.
- Antihistamines can help hives/itch; they are not a substitute for epinephrine during anaphylaxis.
Infant feeding (doctor-directed)
- For diagnosed CMPA, extensively hydrolyzed formula (eHF) is usually first-line.
- If symptoms persist or are severe, amino-acid formula (AAF) may be needed.
- In some regions, hydrolyzed rice formulas are considered.
- Breastfeeding can continue; in selected cases your clinician may suggest a short, guided trial of maternal dairy elimination.
For practical, up-to-date guidance, see WAO DRACMA—Nutritional management of CMA.
A quick note on ghee and “hidden dairy”
Highly clarified ghee contains minimal milk solids, but trace proteins may remain and can trigger symptoms in some people with true milk allergy. Discuss with your allergist before using it. For a lifestyle view on differences and tolerability, see our balanced explainer Ghee vs. Butter.
Foods To Avoid (And How To Scan a Label Fast)
Milk proteins hide in plain sight. Beyond obvious foods like milk, curd/yogurt, paneer, cheese, butter, cream, and milk-based sweets, learn to spot these ingredient words:
- Casein, caseinate, caseinates
- Whey, whey protein, whey solids
- Milk solids, milk powder, nonfat dry milk
- Lactalbumin, lactoglobulin, milk fat (fat alone isn’t the allergen, but can be a marker of dairy processing)
When eating out, ask about ingredients and preparation areas to reduce cross-contact (shared cutting boards, fryers, spatulas). If you’re re-stocking the pantry, we have several dairy-free recipes and ideas you can lean on: Vegan Stuffed Portobellos, Creamy Cauliflower Soup (vegan option), and Homemade Oat Milk.
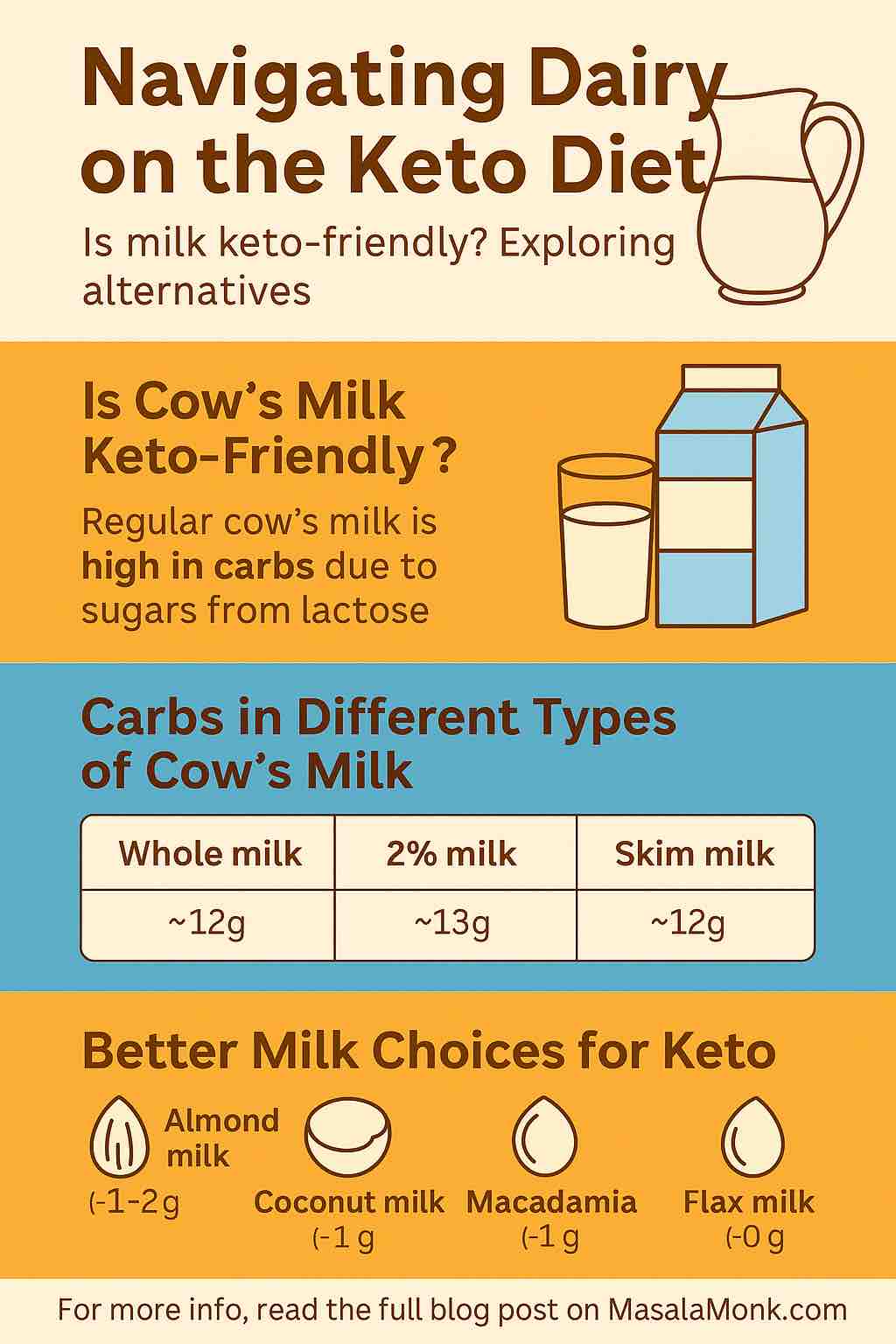
Best Milk Alternatives (Simple and Practical)
For milk allergy, you’ll want non-dairy choices that still provide calcium and vitamin D. Popular options include oat, almond, pea, soy*, and coconut beverages. Always check labels: some brands add milk-like proteins or are processed alongside dairy.
*If soy allergy is a concern, pick non-soy options. A registered dietitian can help balance nutrients during elimination.
Looking for practical ideas? Try our Baby-friendly Apple Pancakes (no milk), or a high-protein plant-based breakfast with dairy-free swaps.
When It Might Not Be Milk Allergy
Plenty of GI-only complaints after dairy—gas, bloating, cramps, diarrhea—are more likely lactose intolerance than allergy, especially in older kids, teens, and adults. Symptoms usually start 30 minutes to a few hours after lactose and don’t include hives, swelling, or breathing issues. Management is different (lactose-reduced diets, lactase tablets, or lactose-free dairy). For a clear, trusted explainer, see NIDDK: Lactose Intolerance.
If your doctor suspects a protein-driven condition affecting the esophagus rather than classic allergy, you might hear about Eosinophilic Esophagitis (EoE). It’s a different condition, but milk is a common trigger; our pragmatic primer EoE: Diet & Treatment Strategies explains the elimination-diet approach in plain English.
A Quick Word on Evidence (For Readers Who Like Receipts)
- For up-to-date clinical guidance on food allergy diagnosis and care (including the role of tests and action plans), see the EAACI IgE-mediated food allergy guideline. A downloadable PDF version is here: EAACI 2024 guideline PDF.
- For infant feeding decisions in CMPA—eHF first, AAF if needed, and when hydrolyzed rice formulas fit—see WAO DRACMA—Nutritional management of CMA (2024).
- On confirming the diagnosis, the AAAAI Oral Food Challenge update (2020) explains why OFC is the gold standard and how it’s done safely.
- For emergencies, the Anaphylaxis Practice Parameter (2023) underscores using epinephrine promptly.
- About baked milk: Kids who tolerate extensively heated milk often outgrow faster; reacting to baked milk predicts a more persistent allergy. Read the full open-access study: Kim et al., JACI 2011.
- For a clear, non-allergy explanation of lactose intolerance, see NIDDK: Symptoms & Causes and NIDDK: Diagnosis.
The Bottom Line
- Milk allergy symptoms can involve skin (hives, swelling, eczema flares), gut (vomiting, diarrhea, mucus/blood in stools in infants), breathing (cough, wheeze, throat tightness), or the whole body (anaphylaxis). Infants and newborns (CMPA) often show rashes, feed-related distress, and specific stool changes; adults can be affected too.
- Tests help, but a supervised Oral Food Challenge is what confirms allergy or tolerance (including baked milk).
- For emergencies, epinephrine is first-line—don’t delay.
- Diet changes for babies and any baked-milk trials should always be clinician-guided.
Final reminder: This article is informational. Please work with your pediatrician/allergist for diagnosis and a safe, personalized plan.
FAQs
1) What are the most common milk allergy symptoms?
Usually, they start with skin and gut signs—think itchy hives, facial swelling, vomiting soon after dairy, tummy cramps, or diarrhea. However, because it’s an immune reaction, breathing symptoms (cough, wheeze, throat tightness) can also appear—and in rare cases, anaphylaxis. In short, symptoms can be fast (minutes to two hours) or slower (hours to days), so timing matters.
2) How do CMPA symptoms show up in newborns and infants?
First, parents often notice feeding fussiness or reflux-like irritability. Next, stools may have mucus or small streaks of blood, and rashes can flare—especially on the cheeks. Finally, if symptoms persist, poor weight gain can follow. It’s the overall pattern—skin + gut + feed issues—that raises suspicion for cow’s milk protein allergy (CMPA).
3) What does a CMPA rash on the face look like?
Typically, you’ll see red, rough, or itchy patches on the cheeks or around the mouth, sometimes spreading to the neck. Because exposure can be frequent with feeds, it may wax and wane. And importantly, if other milk allergy symptoms (like vomiting or wheeze) cluster around feeds, the rash deserves a closer look.
4) Are milk allergy symptoms in adults different from children?
Mostly, no—the same buckets apply: skin (hives/swelling), gut (nausea, cramps, diarrhea), and breathing (cough/wheeze). However, adults more often confuse allergy with lactose intolerance. A quick mental check helps: if it’s mainly gas and bloating without hives or breathing issues, intolerance is more likely than allergy.
5) Milk allergy vs lactose intolerance—how do I tell?
Start with the trigger: allergy reacts to milk proteins (casein/whey), while intolerance struggles with lactose sugar. Then, consider severity and timing: allergy can be rapid and occasionally severe; intolerance is slower and uncomfortable. Finally, remember this rule of thumb—lactose-free milk isn’t safe for milk allergy because it still contains proteins.
6) Which milk allergy test is most reliable?
First comes history (what, how much, how fast). Then, skin-prick or blood tests for specific IgE can support the picture. But when it’s unclear—or to check tolerance (including baked milk)—a supervised oral food challenge is the gold standard. In other words, tests guide; a challenge confirms.
7) Do at-home dairy allergy tests work?
In short, not for diagnosis. Hair analyses and IgG kits can muddy the waters. While they may sound convenient, they can’t replace a proper assessment. A clinical history, targeted tests, and—if needed—an oral food challenge remain the evidence-based path.
8) What are baked milk trials, and who should try them?
Some children with IgE-mediated milk allergy can tolerate milk that’s been baked at high heat (for example, in muffins). Over time, carefully introducing baked milk—if appropriate—may speed tolerance. However, because reactions can still happen, this is a specialist-guided step, not a DIY experiment.
9) What are clear emergency signs to watch for?
If there’s trouble breathing, noisy wheeze, throat tightness, repeated vomiting, fainting, or sudden sleepiness—move fast. Use epinephrine if prescribed and seek urgent care. Antihistamines can calm hives, but they do not treat airway or blood-pressure problems.
10) Which foods to avoid with cow’s milk protein allergy?
Besides obvious dairy (milk, curd/yogurt, paneer, cheese, butter, cream), scan labels for casein/caseinate, whey, milk powder, milk solids, lactalbumin, and lactoglobulin. Then, think about cross-contact: shared fryers, grills, or scoops can transfer tiny amounts of milk protein.
11) Is ghee safe if I have a milk allergy?
Sometimes it’s tolerated, but not always. Although ghee is highly clarified, trace milk proteins may remain. Therefore, if your reactions have been significant—or if you’re unsure—it’s safer to discuss ghee use with your allergist first.
12) What about A1 vs A2 milk for allergy or intolerance?
For allergy, switching protein variants (A1/A2) does not remove milk proteins; reactions can still occur. For intolerance, some people report differences in comfort, but that’s not an allergy fix. In other words, A2 is not a treatment for milk allergy symptoms.
13) Which hypoallergenic formula is used for infants with CMPA?
Generally, the journey starts with extensively hydrolyzed formula (eHF). If symptoms persist or are severe, amino-acid formula (AAF) comes next. Meanwhile, breastfeeding can continue; in selected cases, a short, guided maternal dairy elimination may be considered. The key word is guided.
14) Can lactose-free milk help with milk allergy?
No. It helps lactose intolerance, not allergy. Lactose-free milk keeps the proteins that trigger milk allergy symptoms. For allergy, you need non-dairy alternatives and careful label reading.
15) What are practical milk allergy alternatives?
Start with fortified plant beverages such as oat, almond, pea, soy*, or coconut. Then, check for calcium and vitamin D, and watch for “may contain milk” advisories. *If soy is a concern, pick non-soy options and, when in doubt, ask a dietitian to help balance nutrients.
16) Why do CMPA stools sometimes show mucus or a little blood?
Because some non-IgE presentations inflame the lower gut, tiny streaks of blood or mucus can appear. However, context is everything: clinicians look at growth, feeding comfort, rashes, and response to elimination before calling it CMPA.
17) Are milk allergy symptoms always immediate?
Not necessarily. While many reactions are quick, others take hours or longer—especially gut-focused or eczema-type responses. That’s why keeping a brief food-and-symptom log can be helpful before your appointment.
18) When should I consider a specialist referral?
Consider it when symptoms escalate, when you’ve had breathing issues or systemic reactions, when an elimination diet hasn’t clarified things, or when you’re considering a baked-milk plan. In short, if the picture is complicated—or feels scary—bring in an allergist.
19) Can adults outgrow milk allergy?
It’s less common than in children, but it happens. Meanwhile, tolerance can also shift with time or with guided therapies. Regular re-evaluation with your clinician keeps the plan current and safe.
20) What’s the simple action plan for families?
First, learn your specific triggers and read labels like a pro. Next, keep any prescribed epinephrine close—and practice. Then, share a one-page plan with caregivers and schools. Finally, review progress every few months; kids (and their milk allergy symptoms) can change as they grow.