Intermittent fasting (IF) has become a popular wellness trend — praised for weight loss, improved insulin sensitivity, and even longevity. But here’s the lesser-discussed truth: fasting isn’t just about food — it’s a hormonal event. And cortisol, your body’s primary stress hormone, plays a starring role in that story.
So, is your intermittent fasting routine helping or hurting your hormone balance? Let’s unpack the science, real-world impact, and smart ways to fast without overloading your stress system.
🧬 What is Cortisol — and Why It Matters When You Fast
Cortisol is produced by your adrenal glands and released in a daily rhythm — peaking in the morning to wake you up, then tapering off by bedtime to let your body wind down.
But cortisol is also your “fight or flight” hormone. It spikes in response to:
- Fasting or calorie restriction
- Emotional stress
- Poor sleep
- Blood sugar dips
In small bursts, cortisol is helpful. It keeps you alert and mobilizes energy when you need it.
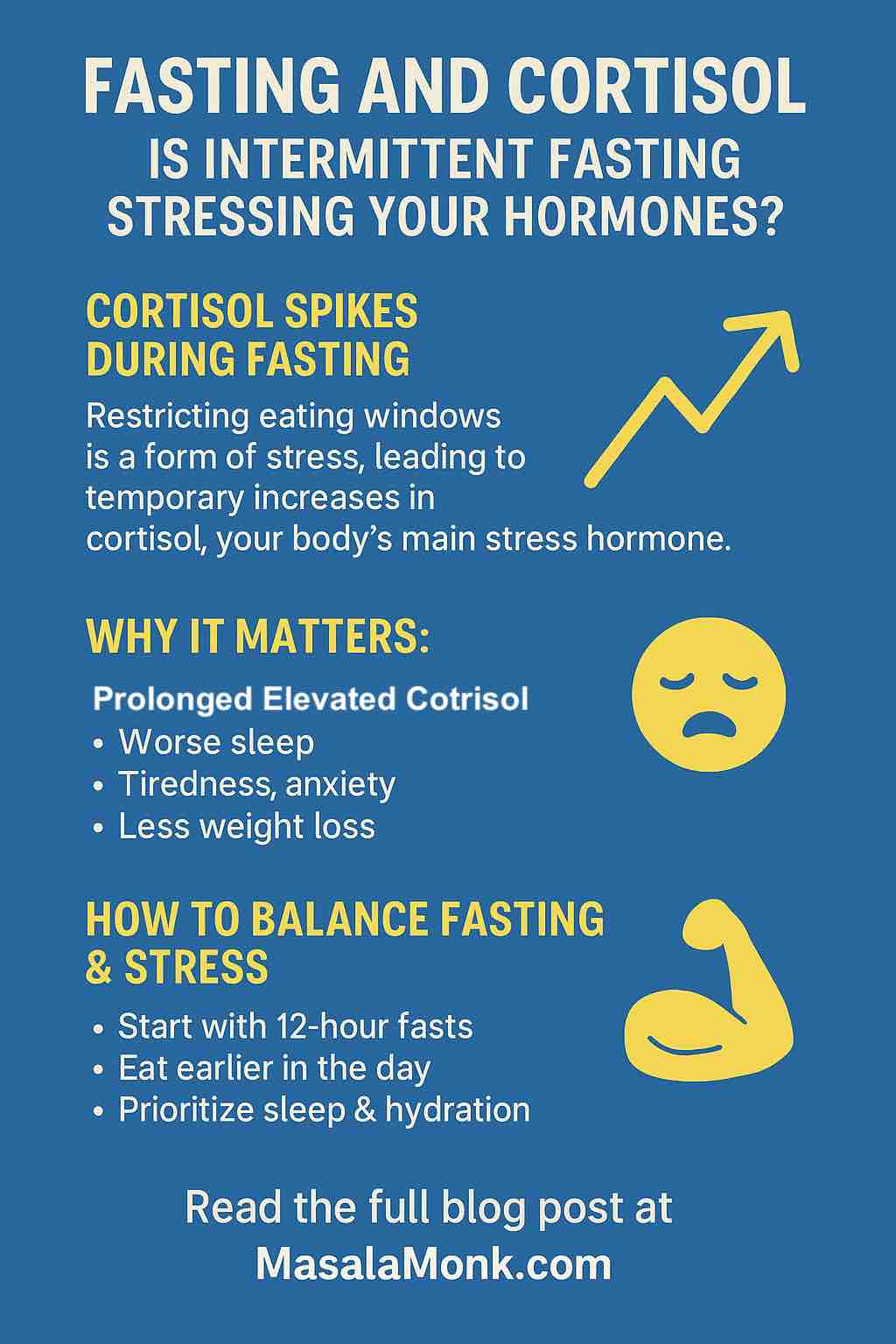
But when it’s chronically elevated, it can lead to:
- Anxiety and poor sleep
- Weight gain (especially belly fat)
- Hormonal imbalances (like low progesterone or testosterone)
- Insulin resistance
- Fatigue or burnout
So how does intermittent fasting fit in?
🧪 The Research: What Fasting Does to Cortisol
🔹 1. Fasting Can Elevate Cortisol — Especially at the Start
A recent 2025 study published in Scientific Reports found that participants on an 8-day water-only fast had consistently elevated cortisol levels from day one through day seven. Their stress hormones didn’t start to normalize until several days after resuming eating.
Even shorter fasts (like 16:8) can cause temporary cortisol spikes, especially during the fasting window. That’s because your body sees fasting as a form of stress.
💡 Key point: Fasting stresses the body — and cortisol helps it cope. But too much fasting, too often, can lead to chronically high cortisol.
🔹 2. Cortisol Timing Shifts With Meal Skipping
Fasting can disrupt the normal circadian rhythm of cortisol. Instead of peaking naturally in the early morning and falling throughout the day, some studies show:
- Skipping breakfast can suppress morning cortisol (which may make you feel sluggish)
- Skipping dinner may lead to elevated evening cortisol, interfering with sleep and repair
🔹 3. Women May Be More Sensitive to Cortisol Spikes from Fasting
Women’s bodies are more hormonally sensitive to stress. Extended fasting can:
- Disrupt menstrual cycles
- Affect fertility
- Trigger anxiety, fatigue, or brain fog
A 2024 review in Frontiers in Nutrition found that time-restricted eating in women increased cortisol rhythm disruption and delayed hormonal recovery compared to men.
⚖️ Cortisol and Weight Loss: Friend or Foe?
Here’s the paradox: cortisol can help with fat burning in the short term. It mobilizes energy and stimulates fat breakdown.
But if cortisol stays high:
- Your body stores more belly fat, especially around the midsection
- You may feel more hungry or experience sugar cravings after breaking your fast
- Sleep disturbances caused by cortisol interfere with fat loss and muscle repair
🔁 So while intermittent fasting can support weight loss, high cortisol might cancel out those benefits — especially if you’re not supporting your body holistically.
✅ How to Fast Without Wrecking Your Hormones
🌞 1. Choose Early Time-Restricted Eating (eTRE)
Try eating between 7 AM and 3 PM or 8 AM to 4 PM — and avoid eating late at night.
✔️ Skipping dinner tends to support cortisol balance better than skipping breakfast.
💧 2. Start Gently with 12–14 Hour Fasts
Instead of jumping to 16:8, start with 12:12 or 14:10. Allow your body to adapt slowly.
✔️ Women, in particular, may benefit from shorter fasting windows — especially during the luteal phase of their menstrual cycle.
🧠 3. Support Stress with Sleep, Hydration, and Movement
Cortisol is highly influenced by:
- Poor sleep (raises cortisol)
- Dehydration (triggers cortisol release)
- Overtraining (especially with fasting)
✔️ Get at least 7–8 hours of sleep and stay well hydrated during fasting windows.
🥗 4. Break Your Fast With Protein + Healthy Fats
Avoid high-carb or sugar-rich meals immediately after fasting. They can cause a blood sugar crash and spike cortisol.
✔️ Opt for eggs, nuts, seeds, avocados, or oily fish when breaking your fast.
🌿 5. Add Cortisol-Calming Foods and Herbs
- Ashwagandha – helps regulate cortisol
- Holy Basil (Tulsi) – supports adrenal function
- L-theanine (green tea) – promotes calm focus
- Magnesium-rich foods – leafy greens, seeds, nuts
✔️ Try herbal teas like tulsi or chamomile during fasting windows.
⚠️ Should You Be Fasting?
Fasting isn’t for everyone — especially if you:
- Have anxiety, burnout, or adrenal fatigue
- Are pregnant, breastfeeding, or trying to conceive
- Struggle with disordered eating
- Have sleep issues or thyroid conditions
If you notice more fatigue, mood swings, poor sleep, or stalled weight loss, your fasting routine may be too stressful.
🔁 In that case, consider switching to a nourishing, regular meal rhythm with cortisol-calming foods instead.
🧠 Final Thoughts: Balance Over Biohacking
Fasting can be a powerful tool — but like any tool, it must be used with context.
If done too aggressively or without supporting your sleep, stress, and nutrition, it may backfire — spiking cortisol, slowing metabolism, and harming hormones.
The goal isn’t to fast harder. It’s to fast smarter, with balance, personalization, and restorative practices at the core.
🔗 Related Reads You’ll Love:
- Coffee and Cortisol: How Your Brew Affects Stress, Weight & Energy
- 5 Soothing Drinks to Lower Cortisol and Calm Your Mind
- Diet Strategies to Lower Cortisol Levels
- 10 Symptoms of High Cortisol in Females
🙋♀️ FAQs: Fasting & Cortisol – What You Need to Know
1. Does intermittent fasting increase cortisol levels?
Yes, intermittent fasting can temporarily raise cortisol levels, especially during the fasting window. Cortisol helps the body mobilize energy in a fasted state, but chronically elevated cortisol can be harmful if fasting is too extreme or poorly supported.
2. Is high cortisol bad for weight loss?
Chronically high cortisol can hinder weight loss by increasing belly fat storage, disrupting sleep, and causing sugar cravings. While fasting can promote fat loss, unmanaged cortisol can slow or reverse those benefits.
3. What is the best fasting window to support healthy cortisol levels?
An early time-restricted eating (eTRE) window, such as 7 AM–3 PM or 8 AM–4 PM, tends to be less disruptive to cortisol rhythms compared to skipping breakfast or eating late at night.
4. Can fasting cause anxiety or poor sleep?
Yes. If fasting raises cortisol too much, it can lead to symptoms like anxiety, restlessness, or waking in the middle of the night — especially if paired with stress, caffeine, or poor hydration.
5. Is intermittent fasting safe for women with hormonal imbalances?
Women tend to be more sensitive to cortisol shifts. Shorter fasts (12–14 hours) may be safer for those with hormone imbalances, irregular cycles, or thyroid issues. Always monitor how your body responds.
6. How can I tell if fasting is increasing my cortisol too much?
Warning signs include: disrupted sleep, mood swings, fatigue, cravings, increased belly fat, or worsened PMS. These may indicate that fasting is stressing your body more than helping.
7. What can I do to reduce cortisol while fasting?
Support your body with good sleep, stress management (like meditation or light movement), proper hydration, and nutrient-dense meals when you break your fast. Herbal teas like tulsi or chamomile can also help.
8. Is it better to skip breakfast or dinner when fasting for hormone balance?
Research suggests skipping dinner (and finishing meals earlier in the day) may be more supportive of cortisol balance and metabolic health than skipping breakfast.
9. Can intermittent fasting lead to adrenal fatigue?
Fasting alone doesn’t cause adrenal fatigue, but fasting plus high life stress, poor sleep, and overexercising can contribute to burnout and hormone dysregulation. Listen to your body and adjust accordingly.
10. What are better alternatives if fasting doesn’t work for me?
If fasting causes issues, consider a regular, nutrient-dense meal routine focused on blood sugar balance: protein, healthy fats, fiber, and cortisol-supportive foods (like leafy greens, nuts, and adaptogens).










[…] curious how eating patterns play into cortisol balance, check out Masala Monk’s guide on “Fasting and Cortisol: Is Intermittent Fasting Stressing Your Hormones?” to explore how certain fasting habits can spike cortisol — and what you can do about […]