Pregnancy is a time of excitement — and a time when you suddenly start questioning every food on your plate.
If you’ve ever stared at a beautiful piece of cod in the market and wondered, “Can I eat this while pregnant?”, you’re not alone.
Cod is a mild, flaky white fish enjoyed all over the world — from traditional British fish & chips to Mediterranean baked fillets. But when you’re expecting, seafood questions usually boil down to two big concerns: Is it safe? And is it good for me and my baby?
In this guide, we’ll explore:
- ✅ Whether cod is safe during pregnancy
- ✅ Its nutritional benefits for expecting mothers
- ✅ How much cod you can safely eat
- ✅ Cooking tips to avoid risks
- ✅ Meal ideas you’ll actually want to eat
- ✅ Links to more pregnancy nutrition resources on MasalaMonk
Let’s dive in.
Is Cod Safe During Pregnancy?
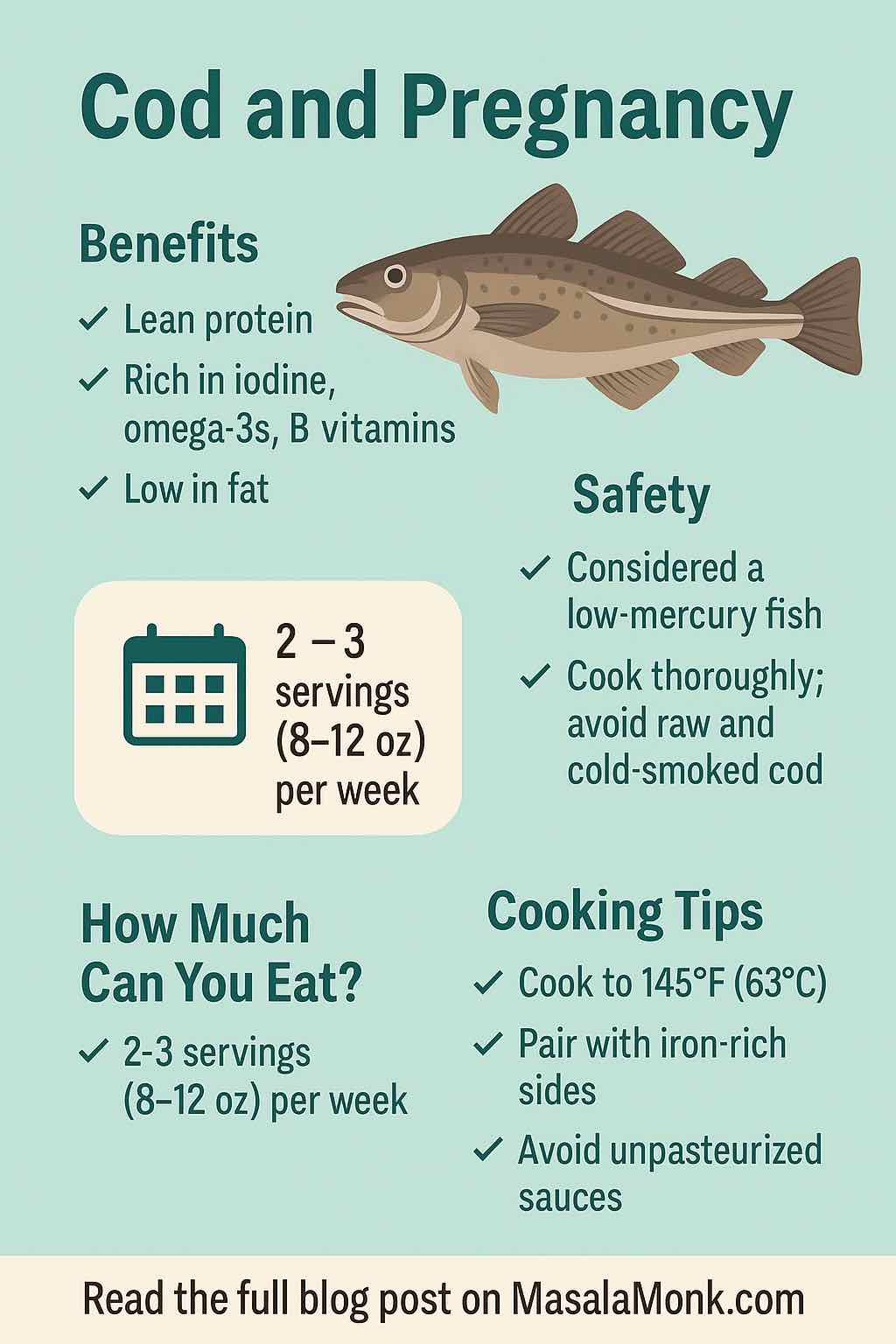
Short answer: Yes, cod is generally safe during pregnancy when eaten in moderation and cooked properly.
Here’s why:
- Low mercury content — Cod is considered a low-mercury fish by both the U.S. FDA and EPA, meaning it’s safer than high-mercury fish like swordfish, shark, and king mackerel.
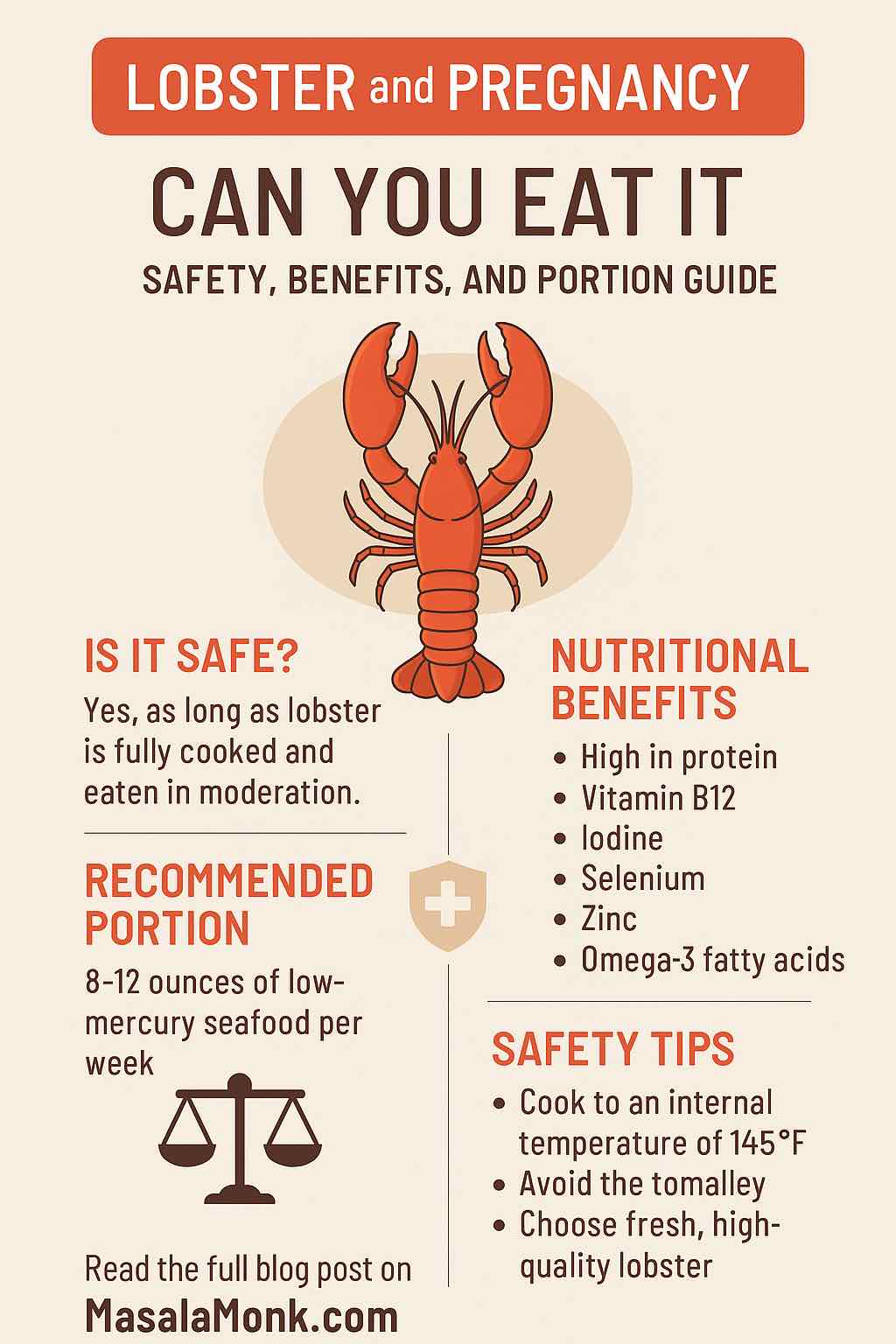
- Recommended serving size — The FDA suggests 2–3 servings (8–12 oz) per week of low-mercury fish for pregnant women.
- Cooking is key — Always cook cod to an internal temperature of 145°F (63°C) to kill any harmful bacteria or parasites.
💡 Tip: If you enjoy a variety of seafood, check out our Guide to Seafood and Pregnancy for a breakdown of safe choices.
Nutritional Benefits of Cod in Pregnancy
Cod is not just safe — it’s also packed with nutrients your body needs during pregnancy.
1. Lean Protein
Protein supports your baby’s growth and helps your body maintain muscle mass.
- A 100g serving of cooked cod provides around 18g of high-quality protein with very little fat.
- It’s lighter than many other protein sources, which is a plus if you’re struggling with nausea.
2. Iodine
Cod is naturally rich in iodine, essential for your baby’s brain and nervous system development.
- Iodine deficiency in pregnancy can affect cognitive development.
- A single serving of cod can provide 30–40% of your daily iodine needs.
For more on first-trimester essentials, see our First Trimester Nutrition Guide.
3. Omega-3 Fatty Acids
While cod is not as omega-3 rich as salmon, it still contains DHA and EPA, which support your baby’s eye and brain development.
- You can complement cod with other omega-rich foods like chia seeds and avocado.
Check out our Omega-Rich Chia & Avocado Meals for plant-based inspiration.
4. B Vitamins
Cod is a source of B6, B12, and niacin, all of which support metabolism, energy production, and blood formation.
5. Low Fat, High Satiety
If you’re aiming to keep your meals light yet filling, cod is a great choice. It’s low in saturated fat but still satisfying when paired with whole grains or veggies.
How Much Cod Can You Eat While Pregnant?
The FDA’s 2025 update recommends 2–3 servings of low-mercury fish per week for pregnant women.
That’s about:
- 8–12 oz (225–340g) per week
- Split into 2–3 meals
Example:
- Grilled cod with vegetables (4 oz)
- Cod curry with brown rice (4 oz)
- Baked cod with sweet potato mash (4 oz)
💡 Don’t forget variety — mix cod with other low-mercury fish like salmon, sardines, and tilapia. See our Salmon and Pregnancy guide for another safe option.
How to Cook Cod Safely During Pregnancy
Safety comes first — here’s how to prepare cod so it’s healthy and risk-free.
- Cook Thoroughly
- Internal temp: 145°F (63°C)
- Flesh should be opaque and flake easily
- Avoid Raw or Undercooked Cod
- No sushi, ceviche, or lightly cured cod while pregnant
- These can carry bacteria like Listeria or parasites
- Watch the Sauces
- Avoid unpasteurized cream sauces or raw egg-based dips (like homemade mayonnaise)
- Pair Smartly
- Serve cod with iron-rich sides like spinach or dates to support healthy blood levels.
Delicious Ways to Enjoy Cod in Pregnancy
Here are a few practical, pregnancy-friendly ideas:
- Baked Lemon Herb Cod – Cod fillet baked with olive oil, lemon, parsley, and garlic.
(Speaking of garlic — see Is it Safe to Eat Garlic During Pregnancy?) - Cod and Vegetable Curry – A mild coconut-based curry with carrots, beans, and turmeric.
- Mediterranean Cod Tray Bake – Cod with tomatoes, olives, zucchini, and oregano.
- Cod Fish Tacos (Well-Cooked) – Grilled cod in whole wheat tortillas with avocado and salsa.
For even more ideas, browse our Omega-3-Rich Seafood Recipes.
Mercury Content in Cod vs Other Fish
| Fish Type | Mercury Level | Safe Servings/Week (Pregnancy) |
|---|---|---|
| Cod | Low | 2–3 |
| Salmon | Low | 2–3 |
| Tilapia | Low | 2–3 |
| Sardines | Very Low | 2–3 |
| Tuna (canned) | Moderate | 1–2 |
| Swordfish/Shark | High | Avoid |
Who Should Limit or Avoid Cod?
While cod is safe for most pregnant women, you should limit intake if:
- You have a fish allergy
- You’re on a very low-iodine diet (rare, but possible in certain medical conditions)
- Your healthcare provider advises limiting seafood due to specific health concerns
Cod vs Other Pregnancy Superfoods
Cod is a great addition to a varied pregnancy diet — but don’t stop there.
Consider these nutrient-dense options:
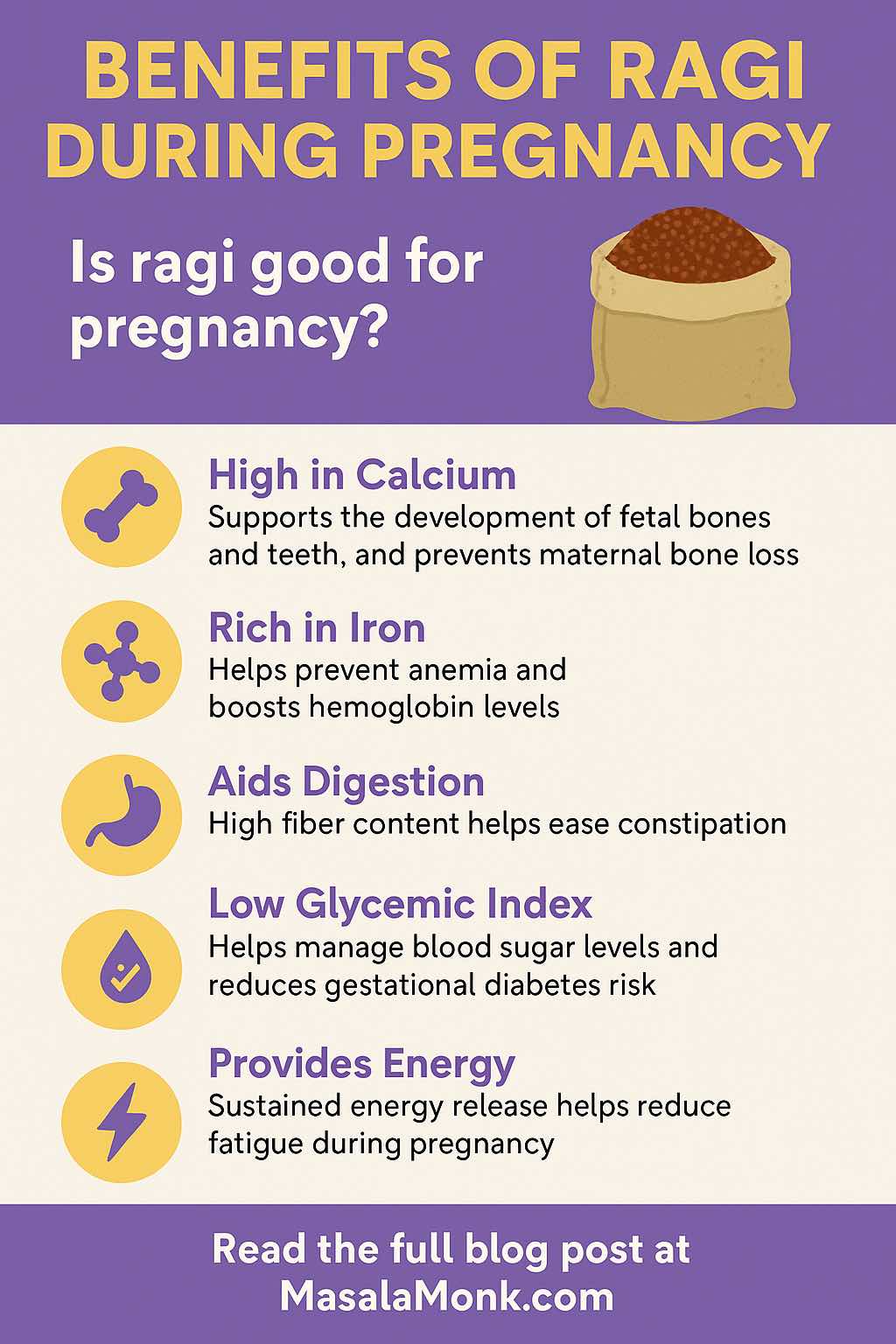
- Ragi (Finger Millet) – Iron, calcium, and fiber-rich; see Benefits of Ragi During Pregnancy
- Dates – Energy and iron boost; see Dates During Pregnancy
- Chia Seeds & Avocado – Plant-based omega-3s; see Chia & Avocado Meals
- Exotic Superfoods – Discover more in 10 Exotic Superfoods for a Healthy Pregnancy
Final Thoughts
Cod can be a safe, nutritious, and versatile part of your pregnancy diet.
It offers lean protein, iodine, omega-3s, and B vitamins — all important for you and your baby’s development.
Stick to 2–3 servings a week, cook it thoroughly, and pair it with a variety of other healthy foods.
By making thoughtful choices, you can enjoy cod’s benefits without worry.
Want to expand your pregnancy-safe seafood menu? Start with our Guide to Seafood and Pregnancy and explore more nourishing options.
Also Read: Best Fish Oil Supplements on Amazon India
10 FAQs for “Cod and Pregnancy”
1. Is cod safe to eat during pregnancy?
Yes. Cod is a low-mercury fish and considered safe in moderation (2–3 servings per week) when fully cooked.
2. How much cod can I eat while pregnant?
The FDA recommends 8–12 oz (225–340g) of low-mercury fish like cod per week, split into 2–3 meals.
3. Does cod have high mercury?
No. Cod has low mercury levels, making it a safer seafood choice during pregnancy compared to swordfish or king mackerel.
4. Can I eat cod in the first trimester?
Yes, cod can be eaten in the first trimester if cooked thoroughly. Its iodine and protein support early fetal brain and cell development.
5. Is cod good for baby’s brain development?
Yes. Cod contains iodine and omega-3s (DHA), both important for your baby’s brain and eye development.
6. Can I eat raw or smoked cod while pregnant?
No. Raw, undercooked, or cold-smoked cod can carry bacteria like Listeria, which poses pregnancy risks. Always eat fully cooked cod.
7. Is frozen cod safe in pregnancy?
Yes. Frozen cod is safe as long as it’s stored properly and cooked thoroughly before eating.
8. What are the nutritional benefits of cod during pregnancy?
Cod provides lean protein, iodine, omega-3s, B vitamins, and is low in saturated fat, making it a nutrient-dense choice for expecting mothers.
9. Can cod help with pregnancy fatigue?
Yes. Cod’s B vitamins and protein can help maintain energy levels and reduce fatigue.
10. Can I eat cod every day while pregnant?
It’s better to vary your seafood intake. Limit cod to 2–3 servings per week and mix with other low-mercury fish for balanced nutrition.